Combination of 2 minimally invasive pain and spine interventions procedures can effectively treat low back pain with radiculopathy along with improvement in quality of life in patients with steppage gait, especially for those who do not want to undergo any surgical procedure.
Dr. Sasmit Dipak Lotliker, Department of Anesthesia and Pain Medicine, Manipal Hospital, Panaji, Goa, India. E-mail: sasmit4u2000@rediffmail.com
Introduction: Low back pain is one of the most common reasons for loss of productivity. Herniated lumbar discs can often cause muscle weakness, reduced motor function, and change in walking capacity including foot drop and gait abnormalities like steppage gait.
Case Report: Here, we present the case report of a 52-year-old shopkeeper who had been suffering from low back pain for 5 years along with a steppage gait since childhood, which had grossly affected his business as well as his quality of life. The patient did not want a surgical procedure.
Discussion: Given these conditions, we opined that minimally invasive pain and spine intervention procedures like transforaminal epidural neuroplasty along with cooled radiofrequency ablation of medial branches can be effective in managing back pain as well as improving the quality of life.
Keywords: Global perceived effect, herniation, low back pain, lumbar disc, quality of life, radiofrequency ablation, steppage gait, transforaminal epidural.
Low back pain is the leading cause of persons living with disability worldwide and the most common reason for loss of productivity [1]. The prolapsed intervertebral disc has been found to be one of the most common pathologies associated with treatable low back pain [2]. Herniated lumbar discs often cause muscle weakness, reduced motor function, and change in walking capacity including foot drop and gait abnormalities like steppage gait [3]. Steppage gait may be defined as an inability to lift the foot while walking, caused by calf muscle weakness. It may lead to dorsiflexion of the ankle joint which may result in traumatic injuries, pelvic fractures, tibia or fibular head fractures, peripheral and axonal neuropathies, herniated lumbar discs, Guillain-Barre syndrome, and Charcot–Marie–Tooth disease [4]. Various tests used for diagnosing this condition include X-rays of the pelvis (anteroposterior [AP] view) and bones of the lower limb to rule out traumatic fracture or dislocation, magnetic resonance imaging (MRI) to look for herniated discs, electromyography (EMG), nerve conduction velocity (NCV) studies, as well as certain blood tests such as complete blood count, rheumatoid factor, and antinuclear antibody [4, 5].
A 52-year-old male came in with a chief complaint of persistent low back pain for 5 years. The pain was a continuous dull ache, which radiated to the left lower limb, and was associated with tingling and numbness. It was aggravated by activities such as lifting heavy weights, walking for a long duration, and turning to the left side when lying in bed. It was relieved when the patient sat, lay down, and/or used a lumbar belt. The patient is a shopkeeper by profession. This pain did not let him sit or stand for long at his shop, which affected his business as well as his quality of life. The patient also had a steppage gait since childhood, for which he had never been evaluated before. He did not have any history of injury, fall, or fracture during childhood. He had no other relevant significant features in his past medical history or family history. The patient had consulted multiple orthopedics and neurosurgeons before consulting with us. He had been prescribed painkillers (celecoxib and diclofenac), steroids (prednisolone), and calcium and Vitamin D supplements, which had no effect in relieving the pain. He was also offered the option of surgery but he did not want any surgical procedure.
Lumbar spine examination revealed spinal tenderness at the L4-L5 level, with a positive left side straight leg raising (SLR) test and crossed SLR test [6, 7]. Examination of the patient through palpation also revealed a prominent steppage gait with atrophy in the calf muscles of the right leg. The patient had pain in the flexion as well as the extension of the lumbar spine (left > right). His lower limb muscle power was 4/5 in the distal component on the right side, as opposed to 5/5 on the left, with the impaired right foot and toe dorsiflexion. The patellar reflex on his right side was diminished [6]. A neurologist who was consulted in this regard advised the patient to undergo electromyogram (EMG) and NCV studies and take the medications prescribed by the pain physician. EMG and NCV showed active radiculopathy in both lower limbs with left-side dominance at L2, L3, L4, L5, and S1 levels. X-ray of the lumbosacral spine (AP and lateral views) showed significant degenerative changes and reduced intervertebral spaces with no evidence of any fracture. MRI of the lumbosacral spine showed disc degeneration and disc bulging at L2-L3, L4-L5, and L5-S1 levels, with bilateral mild neural foraminal compression, with facet joint arthropathy and ligamentum flavum hypertrophy at L2-L3 and L5-S1 disc level, seen in both sagittal and axial sections (Fig. 1 and 2). His routine laboratory examinations did not show any notable abnormalities.
His visual analog score that was recorded before the procedure was 8/10. The patient was initiated on gabapentin 200 mg twice a day, nortriptyline 10 mg twice a day, baclofen 5 mg twice a day, and thiocolchicoside 4 mg twice a day. He was also advised to undergo a proper physiotherapy regimen under the observation of a trained physiotherapist. Dosage of all the drugs was gradually increased over the next 4 weeks to gabapentin 400 mg twice a day, nortriptyline 10 mg twice a day, baclofen 10 mg twice a day, and thiocolchicoside 4 mg twice a day, along with multivitamins. Despite all these measures, the patient did not have any pain relief. Therefore, it was decided that he would be given interventional treatment. The patient was offered percutaneous endoscopic lumbar decompression but declined the treatment.
A positive ultrasound-guided diagnostic lumbar facet block was obtained before the procedure. We also performed a discography at the L2-L3 level (Fig. 3) to assess the extent of annular tears or leak of contrast due to disc degeneration. Based on the Adams classification of discogram morphology, a Type 5 discogram was obtained, which suggested escape of contrast from the disc due to rupture. The patient was given a transforaminal epidural steroid injection (TFESI) (Minimally Invasive Pain and Spine Intervention [MIPSI]) through subpedicular approach (Fig. 4a), with triamcinolone 60 mg, amikacin 100 mg, and 0.5% bupivacaine, a total of 12 mL drug, given 1.5 mL each at bilateral L3, L4, and L5 levels after confirming using a dye spread on neurogram, with left L2-L3 and L5-S1 cooled radiofrequency ablation (RFA) of the medial branch (Fig. 4b).
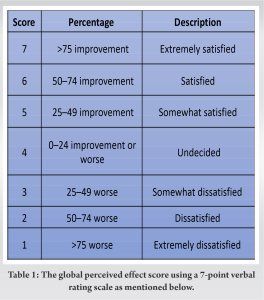
The patient had 100% pain relief (Visual Analog Scale [VAS] of 0/10) immediately after the procedure. Post-procedure, the patient was continued with the pharmacological agents (gabapentin 400 mg twice a day, nortriptyline 10 mg twice a day, baclofen 10 mg twice a day, and thiocolchicoside 4 mg twice a day) along with a physiotherapy regimen. The doses of all the drugs were slowly tapered over the next 3–4 weeks. Currently present, 2 years after the procedure, the patient still has 100% sustained pain relief and is comfortably doing his routine activities. The global perceived effect (GPE) [8] was assessed at 6 months, 9 months, 1 year, and 2 years following the procedure. The GPE was assessed using a 7-point verbal rating scale as mentioned below (Table 1).
The patient gave a rating of 7 out of 7 (extremely satisfied) on the GPE scale when he was assessed at 6 months, 7 out of 7 (extremely satisfied) at 9 months, 7 out of 7 (extremely satisfied) at 1 year, and 7 out of 7 (extremely satisfied) at 2-year post-procedure. He was able to do all his routine activities as well as run his business without any pain. The patient, however, still has the steppage gait. The patient was referred back to the neurologist for further treatment of the steppage gait.
MIPSIs such as TFESIs and cooled RFA of medial branches offer safe, effective, and low-cost definitive treatment with minimal complications, especially in patients with multiple disc level involvement [5]. Gait and balance disorders are common in medicine and are often referred for neurologic evaluation. Since the maintenance of balance and normal gait is mediated by complex neurological pathways as well as musculoskeletal, metabolic, and behavioral considerations, the list of possible contributing causes for their malfunctioning is very large. Most often, the patient’s history and neurologic examination reveal the underlying cause or causes. There may be instances, however, when there are limited neurologic findings as well as no structural abnormalities in the brain or spine MRI studies to explain the imbalance of gait [9]. A normal gait cycle is composed of a stance phase and a swing phase in the ratio of 60:40. When one foot is in the swing phase, the other foot is in the stance phase. The cycle starts with a heel strike on one side and ends with a heel strike on the same side. The foot remains flat on the ground in dorsiflexion during the stance phase, preparing for gradual lowering during the heel strike phase. Any damage or lesion of the L5 nerve root, lumbar plexus, the sciatic nerve in its path, or common peroneal or deep peroneal nerve can potentially lead to a steppage gait due to the weakness of the muscles of the anterior compartment of the leg [4, 10, 11]. Various etiologies can present with a steppage gait such as central or peripheral neuromuscular disorders, stroke, multiple sclerosis, myelopathies, lumbar radiculopathy due to disc herniation or spinal stenosis, and hereditary disorders like Charcot–Marie–Tooth disease. A thorough and detailed evaluation by multiple specialties is required to identify the exact etiology [4, 12]. Patients with a long-standing history of steppage gait will already have a reduced quality of life; and with added disc-related pain, their quality of life will deteriorate further. Furthermore, issues in the lumbar facet joints are known to be a common source of low back pain that often goes undiagnosed. Spine degeneration, also known as spondylosis, is the most common disease affecting the facet joints. It is referred to as degenerative osteoarthritis when it is secondary to abnormal mechanics of the body and natural wear and tear of the facet joints [11, 12]. History and physical examination may suggest but not confirm the diagnosis, and although imaging modalities such as X-ray, MRI, and computed tomography may be commonly performed, there are no effective correlations between clinical symptoms and degenerative spinal changes. These patients may benefit from specific interventions to eliminate facet joint pain such as neurolysis, using RFA or cryoablation [12]. In our patient’s case, since the MRI of the lumbar spine showed definitive disc herniation at multiple levels along with facet joint arthropathy, with the EMG and NCV findings also indicating radiculopathy, we decided to treat the herniated lumbar disc and the facet joint-related pain using MIPSI procedures of TFESI along with Cooled RFA of the medial branch [4]. Post-operative and rehabilitation care is of utmost importance in the recovery of such patients. A consultation with a neurologist along with repeat NCV and EMG studies is also necessary [4]. If post-procedure EMG shows complete loss of continuity along with evidence of neurotmesis or axonotmesis, an ankle-foot orthosis is recommended. The purpose of the brace is to maintain the foot in a neutral position during the toe-off phase of the gait cycle. Periodic skin checks are advisable since the anesthetic foot can develop pressure ulcers at the contact points with the brace. The patient must wear a shoe that is wide enough to accommodate the brace. Tibialis posterior tendon transfer or peroneal or tibial nerve transfer can also be considered for patients who fail to recover from their steppage gait. A home exercise program should be made an integral part of the treatment [4].
The intensity of pain assessed using the VAS as well as the quality of life assessed using the GPE scale are the most important aspects in the management of such patients. At present, at the time of publishing this case report, the patient has sustained even after 2-year post-procedure.
MIPSIs have yielded good benefits for patients with chronic back pain. There is Level I evidence for the use of transforaminal injections for the treatment of lumbar radiculopathy resulting from disc herniations. Using radiofrequency ablative technologies for the nociceptive sensory innervation of the lumbar facet joints has been proven to be an effective therapy for chronic lumbar facet pain. These two MIPSIs can be effectively used for the management of chronic back pain radiating to the lower limbs. The change in the intensity of the pain can be assessed using the VAS and the quality of life can be assessed using the GPE scale. This treatment is recommended especially for patients who do not want to undergo any surgical correction or percutaneous endoscopic lumbar decompression.
References
- 1.Malik K, Nelson A. Overview of low back pain disorders. In: Benzon T, Raja N, Liu S, Fishman SM, Cohen SP, editors. Essentials of Pain Medicine. 4th ed. Netherlands: Elsevier; 2018. p. 193. [Google Scholar]
- 2.Malik K, Nelson A. Overview of low back pain disorders. In: Benzon T, Raja N, Liu S, Fishman SM, Cohen SP, editors. Essentials of Pain Medicine. 4th ed. Netherlands: Elsevier; 2018. p. 196-203. [Google Scholar]
- 3.Morag E, Hurwitz DE, Andriacchi TP, Hickey M, Andersson GB. Abnormalities in muscle function during gait in relation to the level of lumbar disc herniation. Spine (Phila Pa 1976) 2000;25:829-33. [Google Scholar]
- 4.Nori SL, Das M. Steppage gait. In: Stat Pearls. Treasure Island, FL: StatPearls Publishing; 2021. [Google Scholar]
- 5.Shrestha P, Subba L, Agarwal P, Lohani S. Outcome of transforaminal epidural steroid injection for lumbar radiculopathy: Initial three-year experience at Upendra Devkota memorial-national institute of neurological and allied sciences, Nepal. Chin Neurosurg J 2020;6:6. [Google Scholar]
- 6.Nadler F, Rigolosi L, Kim D, Solomon J. Sensory, motor, and reflex examination. In: Malanga A, Mautner K, editors. Musculoskeletal Physical Examination. 2nd ed., Ch. 2. Elsevier; 2016. p. 8-15. [Google Scholar]
- 7.Ebraheim NA, Lu J, Biyani A, Physical examination of the lumbar spine and sacroiliac joint. In: Malanga GA, Mautner K, editors. Musculoskeletal Physical Examination. 2nd ed., Ch. 7. Netherlands: Elsevier; 2016. p. 106-49. [Google Scholar]
- 8.Kamper SJ, Ostelo RW, Knol DL, Maher CG, De Vet HC, Hancock MJ. Global perceived effect scales provided reliable assessments of health transition in people with musculoskeletal disorders, but ratings are strongly influenced by current status. J Clin Epidemiol 2010;63:760-6.e1 [Google Scholar]
- 9.Shill A, Fife D. Causes of imbalance and abnormal gait that may be misdiagnosed. Semin Neurol 2013;33:270-5. [Google Scholar]
- 10.Rivera CE. Lumbar epidural steroid injections. Phys Med Rehabil Clin N Am 2018;29:73-92. [Google Scholar]
- 11.Helm Ii S, Harmon PC, Noe C, Calodney AK, Abd-Elsayed A, Knezevic NN, et al. Transforaminal epidural steroid injections: A systematic review and meta-analysis of efficacy and safety. Pain Physician 2021;24:S209-32. [Google Scholar]
- 12.Manchikanti L, Buenaventura RM, Manchikanti KN, Ruan X, Gupta S, Smith HS, et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician 2012;15:E199-245. [Google Scholar]