Muscular echinococcosis is an extremely rare disease.
Dr. Amir Mhiri, Department of Orthopaedic Surgery, Sahloul Hospital, Sousse, Tunisia. E-mail: amirmhiri1@gmail.com
Introduction: Hydatid diseases are a parasitic infestation of human and herbivorous animals caused by a cestode, Echinococcus granulosus. The liver and lung are commonly involved organs and the involvement of muscles and bones is very unusual, even in the countries where echinococcal infestation is endemic.
Case Report: We report a case of muscular hydatidosis of the hand and forearm in a 71-year-old male without particular histories, who consulted for tumefaction of the right hand and forearm evolving for 2 years. Biology and the standard radiographs were without anomalies. The diagnosis was evoked on magnetic resonance imaging (MRI) and confirmed by surgical biopsy and excision. The operative follow-up was simple with no recurrence after 3 years.
Conclusion: Muscular echinococcosis is an extremely rare disease. An MRI evaluation should be taken into account as the gold standard in the diagnosis. Surgical cystectomy is often indicated, and an excision with wide margins is mandatory to avoid the rupture of the cyst and anaphylaxis. Adjuvant pharmacological therapy is recommended to minimize the risk of recurrence.
Keywords: Hydatidosis, cyst, muscle, hand, forearm, excision.
Hydatidosis is a zoonotic disease; human infection occurs through the consumption of food and water contaminated with the eggs of parasites of the Echinococcus type. The most frequently involved organs are the liver (70%) and lungs (20%). Other organs such as muscle, bones, and central nervous system are rarely involved. Musculoskeletal involvement, which accounts for 3% of hydatid infestation, is very rare even in endemic zones [1]. In the context of musculoskeletal involvement, the spine is the most commonly infected site, whereas the muscles are rarely infected and account for approximately <1% of cases. Hand and forearm muscle involvement is exceptionally rare to occur, with very few cases being reported in the literature [1, 2]. We describe a very unusual case of hydatidosis involving the right hand and forearm muscle in a 71-year-old male patient who presented with a tumefaction of the right hand and forearm evolving for 2 years.
A 71-year-old male was admitted to our institution complaining of a slowly growing tumefaction at the lower third of the forearm and the right hand evolving for 2 years. The patient reported moderate pain; his medical development and family histories were unremarkable. The patient lived in a rural area and he was in close contact with dogs. Physical examination showed a painless, mobile, tender mass at the ulnar edge of the forearm and right hand. There was no ecchymosis, erythema, or signs of local inflammatory or satellite lymphadenopathy (Fig. 1).
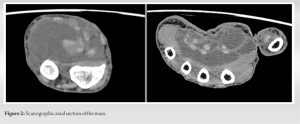
A laboratory examination, including a complete blood cell count, serum chemistries, erythrocyte sedimentation rate testing, C-reactive protein testing, and a coagulation profile, showed values within normal ranges. The computed tomography (CT) scan showed a voluminous septet fluid cystic formation dissecting the muscular masses of the right forearm (Fig. 2).
Magnetic resonance imaging (MRI) showed a multiseptated cystic lesion disseminated in the hand and forearm achieving the appearance of a multivesicular process evoking an extensive hydatidosis of the forearm to the palmar surface of the hand (Fig. 3).
The patient underwent surgical exeresis under general anesthesia. The surgical site was irrigated with hypertonic saline solution (3%), to reduce the risk of recurrence. Intraoperatively, we found multiple cysts of varying size (Fig. 4) suggestive of hydatid cysts. Histological examination of the specimen revealed the lamellar membrane of the hydatid cyst, mixed type of inflammatory cells, connective tissue, histiocytes, and necrosis. The patient received a 4-week post-operative pharmacological therapy with albendazole 400 mg/bid. At the latest available examination 3 years postoperatively, the patient showed no signs of local recurrence.
Hydatid disease is a parasitic infection caused by parasites of the Echinococcus type characterized by the formation of cysts in different organs and tissues. The Echinococcus natural habitat is the small intestine of carnivores [1,3,4]. Two species of Echinococcus (Echinococcus granulosus and Echinococcus multilocularis) cause cystic echinococcosis and alveolar echinococcosis in humans. The disease is particularly common in Asia, North and East Africa, South America, Australia, and the Middle East. Human infestation is accidental by eating food soiled with parasite eggs or by direct contact with the definitive host: Often the dog. The parasite then borrows the portal system to spread in the human body, which explains the rarity of extrahepatopulmonary involvement. Indeed, the liver is the most frequent (62%) site of involvement, followed by the lungs (20%) [1,2,5,6]. Less common sites of involvement include the kidney, heart, spleen, pancreas, and brain. Musculoskeletal echinococcosis is uncommon and accounts for only 3–5% of all cases. Engîn and Sözûer advanced the theory of a lymphatic pathway to explain the atypical and solitary localization of the soft tissues [7]. Several factors can explain the rare occurrence of muscular involvement: First, the muscle is considered an unfavorable habitat for the Echinococcus due to the high levels of lactic acid, which creates an unfavorable growth environment. Second, the role of the hepatic barrier should also be considered [2]. The clinical symptomatology of the muscular hydatidosis is basically a painless swelling of the soft tissues, progressively increasing in size without deterioration of the general status. Sometimes, a local compression chart and/or inflammatory signs simulating a hematoma, abscess, or malignancy are found [2,8]. Plain radiographs are often normal. Sometimes they can show an intracystic calcification in the cases of aged cysts. Ultrasound is the key diagnostic examination with a sensitivity of 100% in typical cases. However, there are atypical forms where the lesion can be mixed, solid, or pseudotumoral with or without a transsonous image [9]. CT scans, which may be confronted with the same diagnostic problems as ultrasound in atypical forms, will better define locoregional, especially vascular, relationships [8,10]. MRI is the most useful imaging medium for hydatid pathology of the soft tissues when the ultrasound appearance is atypical; however, it is expensive and not always available. The visualization of daughter vesicles and/or intracystic membranes allows the diagnosis, as well as the visualization of a T2-weighted relative hyposignal peripheral border, enhancing after injection of gadolinium. It also allows a better analysis of locoregional relations [8]. MRI can also demonstrate the viability of KH [8]. Serological tests such as enzyme-linked immunosorbent assay, immunoelectrophoresis, or immunoblotting can be used for the confirmation of the disease [11]. Ultrasound or CT-guided biopsy can be useful for diagnosis in doubtful and atypical cases without major risks for many authors [11]; however, the results of microscopic analysis of needle biopsy are not always conclusive. The treatment of muscular hydatidosis is often surgical [12]. The fact that the cyst is well encapsulated in the muscle fibers makes pericystectomy easier to perform, taking the entire cyst without breaking its wall [9, 10]. Intraoperative precautionary measures using fields soaked with hypertonic serum prevent local dissemination of scolex. The interest of medical treatment with benzimidazole derivatives (albendazole) in isolated localizations of the musculoskeletal system remains controversial due to their poor diffusion inside the cyst [13]. Some authors advocate that albendazole–praziquantel is more effective than albendazole alone [13]. However, we, like other authors, believe that medical treatment should be reserved for forms of KH complicated by intraoperative disruption, disseminated, or inoperable patients [13]. New techniques have been reported. Ormeci et al. [12] described three patients with five treated muscle KH by puncture–aspiration–injection of alcohol and sclerosant product with good results and concluded that it is a simple, repetitive, and inexpensive technique with simple operating sequences and is an alternative to surgery for selected patients [12].
Muscular echinococcosis is an extremely rare disease. An MRI evaluation should be taken into account as the gold standard in the diagnosis. Surgical cystectomy is often indicated, and an excision with wide margins is mandatory to avoid the rupture of the cyst and anaphylaxis. Adjuvant pharmacological therapy is recommended to minimize the risk of recurrence. Education and information of populations in endemic areas remain the best means of prevention.
Although muscle hydatidosis is very rare and can cause diagnostic difficulties, it should be suspected in any soft-tissue mass with multilocated or multicystic appearance on ultrasonography, CT scanning, or MRI imaging.
References
- 1.Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev 2004;17:107-35. [Google Scholar]
- 2.Orhan Z, Kara H, Tuzuner T, Sencan I, Alper M. Primary subcutaneous cyst hydatic disease in proximal thigh: An unusual localisation: A case report. BMC Musculoskelet Disord 2003;4:25. [Google Scholar]
- 3.Madhar M, Aitsoultana A, Chafik R, Elhaoury H, Saidi H, Fikry T. Primary hydatid cyst of the thigh: On seven cases. Musculoskelet Surg 2013;97:77-9. [Google Scholar]
- 4.Manouras A, Giannopoulos P, Toufektzian L, Markogiannakis H, Lagoudianakis EE, Papadima A, et al. Primary hydatidosis of the gluteus muscles: Report of three cases. Ir J Med Sci 2009;178:359-62. [Google Scholar]
- 5.Omezzine JS, Abid F, Mnif H, Hafsa C, Thabet I, Abderrazek A, et al. Primary hydatid disease of the thigh. A rare location. Orthop Traumatol Surg Res 2010;96:105-8. [Google Scholar]
- 6.Ozkoc G, Arkpmar S, Hersekli AM, Ozalay M, Tandogan R. Primary hydatid disease of the quadriceps muscle: A rare localization. Arch Orthop Trauma Surg 2003;123:314-6. [Google Scholar]
- 7.Engîn OK, Sözûer EM. Solitary subcutaneous hydatid cyst: A case report. Am J Trop Med Hyg 2000;62:583-4. [Google Scholar]
- 8.Bayram M, Sirikci A. Hydatic cyst located intermuscular area of the forearm: MR imaging findings. Eur J Radiol 2000;36:130-2. [Google Scholar]
- 9.Comert RB, Aydingoz U, Ucaner A, Arikan M. Water-lily sign on MR imaging of primary intramuscular hydatidosis of sartorius muscle. Skeletal Radiol 2003;32:420-3. [Google Scholar]
- 10.Mseddi M, Mtaoumi M, Dahmene J, Hamida BR, Siala A, Moula T, et al. Kyste hydatique musculaire. À propos de 11 cas. Rev Chir Orthop 2005;91:267-1. [Google Scholar]
- 11.Freedman AN. Muscular hydatid disease: Report of a case and review of the literature. Can J Surg 1974;17:232-4. [Google Scholar]
- 12.Ormeci N, Idilman R, Akyar S, Palabiyikoğlu M, Coban S, Erdem H, et al. Hydatid cysts in muscle: A modified percutaneous treatment approach. Int J Infect Dis 2007;11:204-8. [Google Scholar]
- 13.Shams-Ul-Bari, Arif SH, Malik AA, Khaja AR, Dass TA, Naikoo ZA, et al. Role of albendazole in the management of hydatid cyst liver. Saudi J Gastroenterol 2011;17:343-7. [Google Scholar]