In chronic neglected shoulder dislocations in the elderly population, management with Latarjet procedure is not enough. The addition of RCR and remplissage is of prime importance for addressing two different pathologies. This procedure is enough to achieve an adequate functional range of movement to carry out daily activities for the elderly population.
Dr. Nrupam Mehta, Department of Orthopaedics, Dr. D Y Patil Medical College and Hospital, Mumbai, Maharashtra, India. E-mail: nrupam.m@hotmail.com
Introduction: There is a paucity of literature regarding a neglected shoulder dislocation, as it is unusual to miss it clinically due to the apparent deformity. Nevertheless, in some cases, particularly those who receive primary treatment from a local bonesetter, they present with neglected dislocation. In the absence of comprehensive studies, health-care professionals have to resort to lower-tier evidence and practical experience to guide their treatment decisions. Therefore, most of the treatment recommendations are based on level four studies and the literature for recurrent dislocation of the shoulder.
Case Report: We have described three cases of neglected anterior dislocation of the shoulders in two patients, which were managed by open reduction and Latarjet procedure, remplissage, and rotator cuff repair (RCR). Both of our patients after 1-year follow-up had a painless joint with an improved functional range of motion. This case discussion contributes to understanding the approach to treating these patients.
Conclusion: Recurrent shoulder joint instability with bone loss in the younger and older age groups has to be managed differently. Based on this case report involving individuals older than 50 years, it can be inferred that the approach to managing neglected locked shoulder dislocations with off-track lesions is with open reduction and fixation with Latarjet procedure, coupled with RCR and remplissage, has yielded adequate joint stability and favorable post-operative outcomes.
Keywords: Locked shoulder dislocation, Latarjet procedure, neglected shoulder dislocation, remplissage.
The incidence of first-time shoulder dislocation in a UK-based study was 21.9 cases/1,00,000 population. Out of these, 7.9% sustained another dislocation, and 6.1% suffered persistent symptomatic instability [1]. A neglected anterior dislocation of the shoulder is very rare, as because of the apparent clinical deformity, it rarely goes unnoticed. However, cases that receive primary treatment from a local bonesetter eventually present with a neglected dislocation. Elderly patients, individuals with a
chronic history of alcohol consumption, and those with a seizure disorder are predisposed to an elevated risk of neglected dislocations [2]. Approximately 16% of all shoulder dislocations
prove refractory to reduction without the administration of sedation [3]. These patients might also seek medical attention at advanced health-care facilities belatedly, especially in developing nations, where primary care centers may lack the resources for reduction under anesthesia.
Case 1
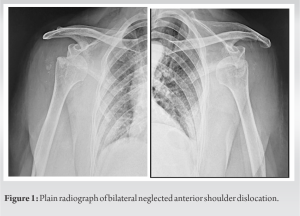
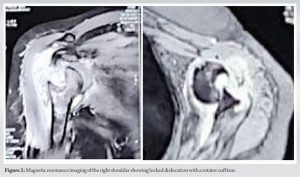
A 70-year-old female sought evaluation in our outpatient department, with the complaint of pain and limited range of motion in both shoulders over the past month. She had a history of falls and went to a bonesetter first followed by a local doctor who referred her to a higher medical facility as he was unable to reduce both suspected shoulder dislocations. Despite that, she delayed seeking assistance for an additional month. On physical examination, there was a loss of deltoid contour. There was no sensory deficit. Duga’s test was positive. The range of motion of the right and left shoulder was grossly restricted and painful. Forward flexion was possible up to 90°, external rotation to 30°, abduction to 30°, and internal rotation restricted. Radiographs revealed bilateral locked anterior shoulder dislocations (Fig. 1 and 2). The magnetic resonance imaging was suggestive of a tear of supraspinatus and infraspinatus with 3 cm retraction in both shoulders (Fig. 2). There was Goutallier grade 2 fatty atrophy.
.
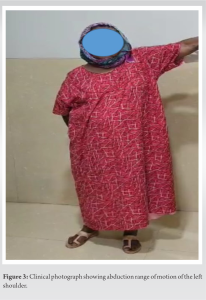
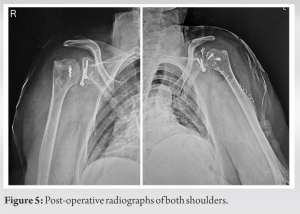
The initial surgical procedure targeted the right side and was conducted under general anesthesia with strict aseptic precautions. The patient was placed in the beach chair position, and the standard deltopectoral approach for shoulder intervention was employed. The coracoid was exposed, and the pectoralis minor muscle attached medially was released. On the lateral side, the coracoacromial ligament was incised, preserving a 1 cm stump. A coracoid osteotomy was performed at the knee of the coracoid, and the undersurface was freshened. The subscapularis muscle was split at its superior two-thirds and inferior one-third junction following which a capsulotomy was done. We then proceeded to reposition the humeral head into the glenoid fossa, and the hill sach’s defect was debrided. 5 mm anchors were inserted at the medial margin of the Hill Sach’s, multiple infranspinatus bites were taken with fibrewire of the anchors, and sutures were tied at the end of the procedure. After which coracoid was securely affixed to the anterior glenoid surface using cannulated cancellous screws. Remplissage knots were tied. The incisional site was sutured in layers. Postoperatively, the limb was kept in a sling for 3 weeks. Pendulum exercises were commenced 3 weeks postoperatively. After 6 weeks, an active range of motion was started with cuff strengthening exercises (Fig. 3). Thereafter, the left shoulder was operated with similar steps after 6 weeks. The patient was followed up at regular intervals for 1 year and has regained full functionality (Fig. 4 and 5).
Case 2
A 70-year-old female patient presented with a 1-month history of pain and restricted movements in her left shoulder. She reported a fall while walking, and she first presented to a local bonesetter. Manipulation was attempted, resulting in an exacerbation of pain and a greater tuberosity fracture. She did not seek any medical attention for another 4 weeks later at our hospital. On physical examination, deltoid muscle wasting was present, the glenoid fossa was empty, and the humeral head was palpable in the anteroinferior glenoid region, with Duga’s test positive. The range of motion in her left shoulder was painful and grossly restricted. Plain radiography showed anterior dislocation of the glenohumeral joint with associated greater tuberosity fracture (Fig. 6).
Thus, we made a diagnosis of neglected locked anterior shoulder dislocation. She was planned for an open reduction and a Latarjet procedure. The patient was placed in a supine position. Under general anesthesia, following appropriate draping and disinfection of the limb, a deltopectoral approach was employed to access the joint. The surgical steps followed were similar as in the first case till coracoid osteotomy. The torn infraspinatus was sutured onto the posterolateral humeral defect with transosseous sutures. Knots were tied at the end of the procedure. The coracoid undersurface was fixed to the glenoid with two cannulated cancellous screws in a conventional manner. The greater tuberosity fracture was reduced to the humeral head and fixed with a proximal humerus locking plate to protect the medial calcar. After hemostasis was achieved, the incisional site was sutured back in layers. Postoperatively, the same rehabilitation protocol was followed as in the first case. The patient achieved full functionality after being followed up for 1 year (Fig 7).
Addressing a neglected shoulder dislocation is challenging due to various complexities. Factors such as soft-tissue contracture, fibrotic changes in the glenoid fossa, and bony lesions worsen the condition, complicating management. Since the dislocation often becomes locked, closed reduction is usually not feasible and may result in fractures. In addition, most patients are elderly with disuse osteoporosis. However, Raptis et al. reported a case of neglected bilateral locked anterior shoulder dislocation with greater tuberosity fractures on both sides, managed nonoperatively through closed reduction and gradual mobilization [4]. They achieved bony union within 3 months and a sufficient range of motion for routine activities within a year. Chaudhary et al. similarly documented successful closed reduction of a 6-month-old neglected dislocation [5]. 90 The management of neglected shoulder dislocation depends on multiple factors including age, bone quality, duration since dislocation, conditions of the rotator cuff, the amount of glenoid and humeral bone loss, and the patient’s activity level. According to Di Giacomo et al., the choice of a surgical procedure such as the Latarjet procedure, Bankart repair, and remplissage depends upon factors such as on-track and off-track lesions, with the percentage of glenoid bone loss seen. Itoi had advised that patients involved in contact sports and those who require a full range of motion should be operated on by a Latarjet procedure [6]. Rouhani and Navali documented outcomes of open reduction and capsulolabral repair in eight patients with non-engaging Hill Sach’s lesions [7-9]. Despite limited motion in all planes, patients managed their daily activities without significant pain. They expressed satisfaction with the intervention despite residual joint stiffness. In our reported cases, locked dislocation presented with glenoid bone loss of more than 25%, Hill Sach’s Index was 20 mm, off-track lesion, with one patient having an additional greater tuberosity fracture. Hence, a bony procedure was the only option. The major contributing factor for instability in elderly patients with shoulder dislocation is rotator cuff tear along with other lesions. In our elderly patients, there was an off track lesion with a large humeral head defect which would contribute largely to instability even after Latarjet. Hence, we performed an additional rotator cuff repair (RCR) where we did a supraspinatus repair and remplissage with infraspinatus. [5, 10].
Recurrent shoulder joint instability with bone loss in the younger and older age groups has to be managed differently. Based on this case report involving individuals older than 50 years, it can be inferred that the approach to managing neglected locked shoulder dislocations with off-track lesions is with open reduction and fixation with Latarjet procedure, coupled with RCR and remplissage, has yielded adequate joint stability and favorable post-operative outcomes.
In the elderly population who have had chronic neglected shoulder dislocations, managing them with RCR and remplissage is of prime importance for addressing two different pathologies, only a Latarjet procedure is not enough. Using RCR and remplissage additionally achieve an adequate functional range of motion to carry out daily activities for the elderly population.
References
- 1.Shields DW, Jefferies JG, Brooksbank AJ, Millar N, Jenkins PJ. Epidemiology of glenohumeral dislocation and subsequent instability in an urban population. J Shoulder Elbow Surg 2018;27:189-95. [Google Scholar]
- 2.Loebenberg MI, Cuomo F. The treatment of chronic anterior and posterior dislocations of the glenohumeral joint and associated articular surface defects. Orthop Clin North Am 2000;31:23-34. [Google Scholar]
- 3.Furuhata R, Kamata Y, Matsumura N, Kono A, Morioka H. Risk factors for failure of reduction of anterior glenohumeral dislocation without sedation. J Shoulder Elbow Surg 2021;30:306-11. [Google Scholar]
- 4.Raptis K, Koutserimpas C, Alpantaki K, Kaiafas S, Fandridis E, Bourlos D. Neglected bilateral anterior shoulder dislocation following epileptic seizure: A case report and literature review. Kurume Med J 2019;66:65-70. [Google Scholar]
- 5.Chaudhary D, Joshi D, Jain V, Mohindra M, Mehta N. A six months old neglected anterior shoulder dislocation managed by closed reduction and Latarjet procedure. Chin J Traumatol 2016;19:295-7. [Google Scholar]
- 6.Chen AL, Hunt SA, Hawkins RJ, Zuckerman JD. Management of bone loss associated with recurrent anterior glenohumeral instability. Am J Sports Med 2005;33:912-25. [Google Scholar]
- 7.Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: From “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthrosc J Arthrosc Relat Surg 2014;30:90-8. [Google Scholar]
- 8.Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow 2018;10:15-24. [Google Scholar]
- 9.Peshin C, Jangira V, Gupta RK, Jindal R. Neglected anterior dislocation of shoulder with large Hillsach’s lesion and deficient glenoid: Treated by autogenous bone graft and modified Latarjet procedure. J Clin Orthop Trauma 2015;6:273-6. [Google Scholar]
- 10.Itoi E. ‘On-track’ and ‘off-track’ shoulder lesions. EFORT Open Rev 2017;2:343-51. [Google Scholar]