This case report sheds light on the importance of individualized treatment plans for non-union distal femur fractures, particularly when complications such as implant failure are encountered. It underscores the significance of a multidisciplinary approach, meticulous pre-operative planning, and the judicious use of advanced fixation techniques in achieving successful outcomes in challenging orthopedic cases.
Dr. Adnan Anwer, Department of Orthopaedic Surgery, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, Uttar Pradesh, India. E-mail: dr.adnan.amu@gmail.com
Introduction: Non-union fractures of the distal femur pose significant challenges in orthopedic surgery, often requiring revision procedures to achieve successful bone healing. In cases where the initial implant has failed, innovative solutions are necessary to promote bone union and functional recovery.
Case Report: We present a case of a non-union distal femur fracture in a 22-year-old male patient, with a broken implant in situ. The patient had previously undergone internal fixation with a locking plate, which subsequently failed to promote bone healing. The patient was reoperated using a supracondylar nail and augmented with a distal femur locking plate to address the non-union. The combination of the supracondylar nail and distal femur locking plate successfully provided stability to the fracture site, promoting bone union and enabling functional recovery. Radiographic evidence and clinical assessment demonstrated excellent healing progress.
Conclusion: This case report highlights the importance of individualized treatment for non-union distal femur fractures, especially when prior implant failure occurs. The combined approach of a supracondylar nail and distal femur locking plate can be a valuable option in addressing complex non-union fractures, achieving stable fixation, and facilitating successful bone healing.
Keywords: Non-union fracture distal femur, broken implant, supracondylar nail, locking plate, revision surgery.
Non-union distal femur fractures pose a formidable challenge in orthopedic practice. These fractures, a distinct subtype of periarticular fractures, are on the rise, particularly in elderly and osteoporotic patients [1]. These complex injuries often result from a multitude of factors, including the extent of comminution, soft tissue damage, and inherent difficulties in achieving stable fixation. Accounting for approximately 6% of all femur fractures, nearly half of them are open fractures [2,3]. Despite the availability of various treatment options, the clinical and functional outcomes often involve complications such as significant morbidity, joint stiffness, and delayed union. The complexity escalates when there is the presence of a broken implant in situ from a previous surgical intervention, which further complicates non-union management. In these instances, innovative solutions and comprehensive surgical strategies become imperative to promote bone healing and restore the patient’s functional capacity. Conventionally, distal femur locking compression plate and retrograde supracondylar nailing have been the go-to modalities for treating distal femur fractures, both exhibiting similar union rates [4,5]. However, while dual plating offers a more robust fixation, the necessity for a second surgical incision introduces potential soft tissue complications, potentially hindering fracture healing. In cases with complex fracture patterns, neither of these methods provides adequate biomechanical stability for early weight-bearing and mobilization, particularly in the presence of osteoporosis [5-9]. The use of nail plate constructs (NPCs) offers a promising solution by enhancing biomechanical stability and restoring limb alignment. This approach potentially facilitates early rehabilitation, weight-bearing, and reduces the risk of fixation failure [10-14]. The biomechanics of the NPC differ from the lateral locking plate. The retrograde intramedullary nail redirects the weight-bearing axis closer to the anatomical axis of the femur, dispersing forces across the surrounding cortex and through the nail-cortical interface. This combination creates a more robust architectural foundation, enabling early patient mobilization and improving the prospects of achieving union [8,9]. Research by Liporace and Yoon [10] highlights how the intramedullary implant’s placement initially shifts the weight-bearing axis toward the femur’s anatomical axis, with the lateral locking plate providing additional stability to minimize movement at the fracture site. This article explores a compelling case in which a non-union distal femur fracture was encountered in a 22-year-old male patient, with the added complexity of a fractured implant still in place from a prior fixation attempt using a distal femur locking plate. The successful management of this challenging scenario required a unique approach. By revising the surgical strategy and implementing a combination of a supracondylar nail and a distal femur locking plate, this case provides a valuable example of the intricate decision-making and surgical technique employed to address non-union fractures in a manner that promotes bone union and reestablishes mobility.
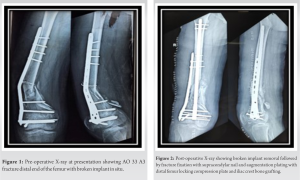
A 22-year-old male presented with a complaint of pain in the right distal thigh with a history of closed fracture in the distal femur which he got operated on with open reduction internal fixation with distal femur locking compression plate 1.5 months back. On radiological examination, it was discovered that the Arbeitsgemeinschaft fur Osteosynthesefragen (AO) 33–A3 fracture distal end femur showed no signs of healing with broken LCP in situ (Fig. 1).
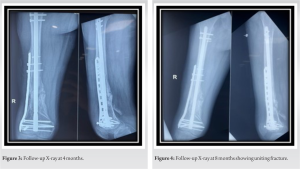
The patient was planned for revision surgery and managed by removing the broken distal femur locking plate and fixation of the fracture with retrograde supracondylar nail and augmentation plating with distal femur locking compression plate with cancellous bone grafting using ipsilateral iliac crest (Fig. 2).
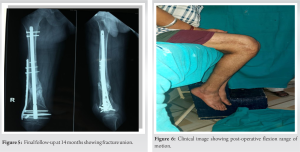
Postoperatively the patient was followed at 4, 8, and 14 months (Fig. 3-5) with the radiological examination which showed intact implants and signs of fracture healing. Final follow-up at 14 months yielded excellent range of motion in operated limb. (Fig 6-9)
The management of non-union distal femur fractures has undergone significant evolution over the years, with numerous techniques developed for their treatment. In the early 20th century, conservative approaches predominated for these fractures. It was not until around 1970 that the emerging principles of the AO were applied to address these fractures [15-18]. Despite the variety of treatment options available today, non-union distal femur fractures remain challenging and complex. The two most commonly employed fixation methods for distal femur fractures are retrograde intramedullary nails and locking plates. However, neither has conclusively demonstrated superiority over the other [4-7].
The management of non-union distal femur fractures complicated by broken implants is a challenging endeavor in orthopedic surgery. This case report highlights the potential benefits of using a combination of a supracondylar nail and distal femur locking plate to address such complex cases. Nevertheless, further research and clinical studies are needed to establish the broader applicability and long-term outcomes of this surgical approach. The importance of individualized care, a multidisciplinary approach, and meticulous surgical technique cannot be overstated in achieving favorable results in these intricate orthopedic scenarios.
Limitations study
The short duration of follow-up is the limitation of this case report. Further research, including larger clinical studies, is needed to validate the efficacy and safety of the combined surgical technique in addressing non-union distal femur fractures with broken implants.
Non-union fractures of the distal femur, especially when complicated by the presence of a broken implant, pose intricate challenges in the field of orthopedic surgery. In this case report, we have demonstrated that a combined approach involving the use of a supracondylar nail and a distal femur locking plate can be a promising solution to address such complex scenarios. The case presented here reflects several important considerations and outcomes. First and foremost, the successful management of non-union fractures requires a patient-specific approach. Each case is unique, and the treatment strategy must be tailored to the individual’s specific circumstances, taking into account factors such as the fracture pattern, bone quality, and previous implant status. Early mobilization and post-operative physiotherapy play a pivotal role in the recovery process, aiding in the restoration of function and minimizing the risk of complications. While the presented case had a positive outcome with radiographic evidence of bone healing and clinical improvement, it is essential to acknowledge that complications can still occur. Vigilance in monitoring for potential complications, such as infection, implant failure, or malalignment, is crucial for timely intervention.
This case report exemplifies the need for innovative and individualized approaches in the management of challenging non-union distal femur fractures. The use of a supracondylar nail and distal femur locking plate offers a potential solution, but the field requires more extensive research and clinical evidence to firmly establish the reliability and long-term outcomes of this approach. Despite the complexities involved, with careful planning, and a patient-centred approach, it is possible to achieve favorable results in addressing these intricate orthopedic scenarios. Furthermore, the first treatment should be optimal to avoid revision.
References
- 1.Griffin XL, Parsons N, Zbaeda MM, McArthur J. Interventions for treating fractures of the distal femur in adults. Cochrane Database Syst Rev 2015;2015:CD010606. [Google Scholar]
- 2.Reudi TP, Buckley RE, Moran CG. AO Principles of Fracture Management. Switzerland: AO Publishing; 2007. [Google Scholar]
- 3.Martinet O, Cordey J, Harder Y, Maier A, Bühler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury 2000;3:C62-3. [Google Scholar]
- 4.Gill S, Mittal A, Raj M, Singh P, Singh J, Kumar S. Extra articular supracondylar femur fractures managed with locked distal femoral plate or supracondylar nailing: A comparative outcome study. J Clin Diagn Res 2017;11:RC19-23. [Google Scholar]
- 5.Markmiller M, Konrad G, Südkamp N. Femur-LISS and distal femoral nail for fixation of distal femoral fractures: Are there differences in outcome and complications? Clin Orthop Relat Res 2004;426:252-7. [Google Scholar]
- 6.Demirtaş A, Azboy I, Özkul E, Gem M, Alemdar C. Comparison of retrograde intramedullary nailing and bridge plating in the treatment of extra-articular fractures of the distal femur. Acta Orthop Traumatol Turc 2014;48:521-26. [Google Scholar]
- 7.Hierholzer C, Von Rüden C, Pötzel T, Woltmann A, Bühren V. Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: A retrospective analysis. Indian J Orthop 2011;45:243-50. [Google Scholar]
- 8.Park J, Lee JH. Comparison of retrograde nailing and minimally invasive plating for treatment of periprosthetic supracondylar femur fractures (OTA 33-A) above total knee arthroplasty. Arch Orthop Trauma Surg 2016;136:331-8. [Google Scholar]
- 9.Attum B, Douleh D, Whiting PS, White-Dzuro GA, Dodd AC, Shen MS, et al. Outcomes of distal femur nonunions treated with a combined nail/plate construct and autogenous bone grafting. J Orthop Trauma 2016;31:e301-4. [Google Scholar]
- 10.Liporace FA, Yoon RS. Nail plate combination technique for native and periprosthetic distal femur fractures. J Orthop Trauma 2019;33:e64-8. [Google Scholar]
- 11.Birjandinejad A, Ebrahimzadeh MH, Ahmadzadeh-Chabock H. Augmentation plate fixation for the treatment of femoral and tibial nonunion after intramedullary nailing. Orthopedics 2009;32:409. [Google Scholar]
- 12.Wright DJ, DeSanto DJ, McGarry MH, Lee TQ, Scolaro JA. Supplemental fixation of supracondylar distal femur fractures: A biomechanical comparison of dual-plate and plate-nail constructs. J Orthop Trauma 2020;34:434-40. [Google Scholar]
- 13.Starr AJ, Jones AL, Reinert CM. The “swashbuckler”: A modified anterior approach for fractures of the distal femur. J Orthop Trauma 1999;13:138-40. [Google Scholar]
- 14.Başcı O, Karakaşlı A, Kumtepe E, Güran O, Havıtçıoğlu H. Combination of anatomical locking plate and retrograde intramedullary nail in distal femoral fractures: Comparison of mechanical stability. Eklem Hastalik Cerrahisi 2015;26:21-6. [Google Scholar]
- 15.Mahorner HR, Bradburn M. Fractures of the femur: Report of 308 cases. Surg Gynecol Obstet 1933;56:1066-979. [Google Scholar]
- 16.Wenzel H, Casey PA, Herbert P, Belin J. Die operative behandlung der distalen femurfraktur. Arbeitsgemeinschaft fur Osteosynthesefragen Bulletin; 1970. [Google Scholar]
- 17.Krettek C, Schandelmaier P, Miclau T, Bertram R, Holmes W, Tscherne H. Transarticular joint reconstruction and indirect plate osteosynthesis for complex distal supracondylar femoral fractures. Injury 1997;1:A31-41. [Google Scholar]
- 18.Neer CS 2nd, Grantham SA, Shelton ML. Supracondylar fracture of the adult femur. A study of one hundred and ten cases. J Bone Joint Surg Am 1967;49:591-613. [Google Scholar]
- 19.Jankowski JM, Szukics PF, Shah JK, Keller DM, Pires RE, Liporace FA, et al. Comparing intramedullary nailing versus locked plating in the treatment of Native distal femur fractures: Is one superior to the other? Indian J Orthop 2021;55:646-54. [Google Scholar]
- 20.Quinzi DA, Ramirez G, Kaplan NB, Myers TG, Thirukumaran CP, Ricciardi BF. Early complications and reoperation rates are similar amongst open reduction internal fixation, intramedullary nail, and distal femoral replacement for periprosthetic distal femur fractures: A systematic review and meta-analysis. Arch Orthop Trauma Surg 2021;141:997-1006. [Google Scholar]
- 21.Garala K, Ramoutar D, Li J, Syed F, Arastu M, Ward J, et al. Distal femoral fractures: A comparison between single lateral plate fixation and a combined femoral nail and plate fixation. Injury 2022;53:634-9. [Google Scholar]