The aim of this article is to demonstrate that the use of a hybrid procedure combining the Masquelet technique with the Ilizarov external fixator and reamer-irrigator-aspirator can be an effective way to treat bone defect in an open tibial fracture classified as a Gustilo-Anderson III.
Dr. Kenny Pestiaux, Department of Orthopaedic Surgery, Pôle Hospitalier Jolimont, Réseau HELORA, Haine-Saint-Paul, Belgium. E-mail: kenny.pestiaux@student.uclouvain.be
Introduction: The induced membrane technique was initially described by Masquelet in 1986 as a treatment for tibia non-union. It then became an established method in the management of bone defects. A critical bone defect is defined by a gap larger than 25 mm, and so, has a higher probability of non-union. Many techniques have been described to resolve this problem such as segmental bone transport, free vascular fibula graft, non-vascular fibula graft, autogenous graft, or megaprothesis.
Case Report: We present the case of a 37-year-old woman who presented a multi-fragmentary open fracture of the tibia and fibula bilaterally (Gustilo-Anderson III) after a high-velocity car accident.
Conclusion: The aim of this article is to demonstrate that the use of a hybrid procedure combining the Masquelet technique with the Ilizarov external fixator and reamer-irrigator-aspirator can be an effective way to treat bone defect in an open tibial fracture classified as a Gustilo-Anderson III.
Keywords: Masquelet technique, open tibia fracture, Ilizarov external fixator, reamer-irrigator-aspirator, bone defect.
Gustilo-Anderson III fracture is very frequent in high-energy trauma such as car accidents. It is defined as an open fracture with tissue damage, bone loss, and a wound larger than 10 cm. There are three different types (A, B, and C) according to the severity of the soft-tissue injury and the need for vascular reconstruction and they are associated with a high rate of wound infection, non-union, loss of limb function, and amputation, especially in severe cases (Type C) associated with neurovascular damage. A mangled extremity severity score ≥ 7 is a predictor of limb amputation. Managing these injuries remains an orthopedic challenge because of the need to manage both the soft tissue and the skeletal component of the fracture. A critical bone defect is defined by a gap larger than 25 mm, and so, has a higher probability of non-union [1]. Many techniques have been described to resolve this problem such as the segmental bone transport, free vascular fibula graft, non-vascular fibula graft, autogenous graft, or megaprothesis [2]. As said before the induced membrane technique was initially described by Masquelet as a treatment for tibia non-union in two-stage reconstruction of bone loss [3]. Other procedures are known to be beneficial to the acute management of tibial shaft fractures with a bone defect for instance the reamer-irrigator-aspirator (RIA) [4]. In this case, we used an induced membrane technique associated with a RIA and an Ilizarov external fixator to efficiently treat a Gustilo-Anderson III-A/B tibial fracture.
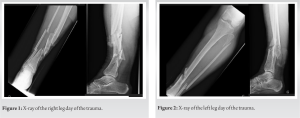
A 37-year-old woman arrived by ambulance at the emergency room after being hit at high speed by a crazy driver. She was rapidly transferred to the intensive care unit due to hypotension and blood loss. A total body scan was performed and showed multiple fractures: Costal fractures (1–9), nose fracture, mandibular, temporal and sphenoidal fracture, left clavicle fracture, multifragmentary left humeral fracture, and finally multi-fragmentary open fracture of the tibia and fibula bilaterally (Fig. 1 and 2).
Unfortunately, the patient had an extradural hematoma that needed urgent drainage and that limited the orthopedic treatment pushing us to be creative. In this context, we decided to perform a provisional fixation for the tibia and fibula bilaterally and for the humeral fracture with an aim to “damage control.” [Fig. 3]. The clavicle fracture was managed the next day by osteosynthesis.
Twelve days later (J12) we proceeded to remove the left lower limb external fixator to put an intramedullary nail. The immediate post-operative was marked by the development of an ischemic colitis that needed colonic resection. After digestive management (at J32) we removed the right leg external fixator and completed the procedure with an intramedullary nail.
The patient was authorized to weight bearing with crutches and was discharged from hospital care. Six months after the trauma, the patient came back to the emergency room due to increased pain in her right leg. Imaging showed a deep abscess at the site of the fracture associated with osteomyelitis and devascularisation of the bone.[Fig. 4] Bacteriology showed a multi-resistant Staphylococcus aureus treated with vancomycin than linezolid.
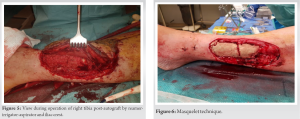
Surgical treatment was divided into two stages: The first stage: Removal of the intramedullary nail, debridement of all necrotic bone, and application of an external fixator. Bone loss resulted in a gap above 7 cm so we practiced the “Masquelet Technique” using an antibiotic-impregnated cement spacer (PALACOS R+G) as a biological chamber (Fig. 6). At the same time, our plastic surgery team performed a large dorsal free lap transplantation to cover the surgical site.
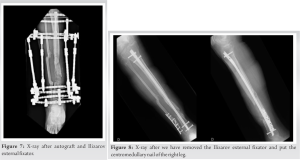
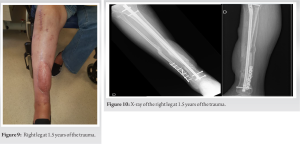
Second stage: 6 weeks after the Masquelet Technique, we finally removed the cement spacer and replaced it with an autograft. Two techniques were combined to create the graft: We used a RIA in the femoral shaft to achieve a high volume of mesenchymal stem cells and we used a piece of the iliac crest as an autograft. Once w had enough graft, we removed the spacer to recanalize the tibia and apply our graft (Fig. 5). We completed the procedure by applying an Ilizarov external fixator (Fig.7). The patient was authorized to weight-bearing after 3–4 weeks after the wound had healed. As the graft evolved correctly and because the patient could not tolerate the fixator any longer, we decided to remove the Ilizarov external fixator after 6 months and replace it with a Sarmiento orthosis. She could not weight bearing for 2 weeks. Follow-up at 1 month showed recurvatum of the tibia as the junction between the graft and the distal tibia was not strong enough. In addition, the fibula was badly consolidating, and a vicious cal was responsible for fibula recurvatum. We attempted to resolve the issue by applying an intramedullary nail in the tibia, doing a corrective osteotomy, and fixation of the malunion of the fibula and finally, we had to perform a tenotomy of the Achilles tendon (Fig. 8). The procedure was a success. The initiative to put the nail allowed quicker and better rehabilitation for our patients. A follow-up at 5 months showed correct wound healing and perfect skeletal axis (Fig. 9 and 10). There was no residual pain.
Open fractures are complex injuries. The Gustilo-Anderson classification helps evaluate the risk of infection and guide antibiotic therapy but there are still unpredictable complications associated with these fractures that make them difficult to treat. The high rate of amputation should push orthopedics to be creative and find new ways to manage Gustilo-Anderson fractures, especially type III B and III C. With this case report, we aim to demonstrate how we managed different complications to preserve the function of the limb and especially how we managed a large bone loss due to infection. Different techniques are used to treat bone loss according to the size and location [5]. In this case, the bone defect was moderate (7–12 cm) and so we chose to perform the Masquelet technique. The Masquelet technique allows to contain osteoprogenitor cells and growth factors that help in revascularization, bone healing, and consolidation [6]. To complete the procedure, we decided to use the Ilizarov external fixator and for the graft, we combined the reamer-irrigator with an iliac autograft. The utilization of multiple techniques is made to maximize the good results with avoiding the negative aspects of each technique [7]. The choice of graft was based on the size of the gap. An iliac graft alone would not had been sufficient. A reamer-irrigator allows a reliable and large amount of autologous bone graft with few morbidities. The usual complications are the risk of cortical perforation and blood loss. The blood loss was anticipated thanks to our anesthesia team [8-10]. Thanks to our plastic surgery team, we used a free tissue transfer to cover our Masquelet and graft techniques that is considered a viable option in great bone defects with large soft-tissue deficits in the lower limb [11]. We used an Ilizarov external fixator after applying the graft because the efficacity of the Ilizarov is higher than an AO external fixator in terms of soft tissue complications and weight-bearing [12].
Thanks to our hybrid procedure, we were able to benefit from all techniques. The Masquelet technique allowed to contain osteoprogenitor cells and growth factors that helped in revascularization, bone healing, and consolidation. The use of an Ilizarov fixator reduced soft tissue complications and allowed quicker weight-bearing. The RIA allowed a reliable and large amount of autologous bone grafts. More studies and case reports are needed to support and approve this technique.
Gustilo-Anderson III fracture is very frequent in high-energy trauma such as car accidents. Managing these injuries remains an orthopedic challenge because of the need to manage both the soft tissue and the skeletal component of the fracture. This case report illustrates that the use of our hybrid technique using the Masquelet technique associated with the Ilizarov external fixator and the RIA can be an efficient way to treat bone defects in an open tibial fracture. Combining all techniques could allow a quicker and better rehabilitation for the patient.
References
- 1.Haines NM, Lack WD, Seymour RB, Bosse MJ. Defining the lower limit of a “Critical bone defect” in open diaphyseal tibial fractures. J Orthop Trauma 2016;30:e158-63. [Google Scholar]
- 2.Issaoui H, Fekhaoui MR, Jamous M, Masquelet AC. Modified masquelet technique using allogeneic graft for a Gustilo-Anderson Type III-A open fracture of the femur with an 8 cm bone defect. Case Rep Orthop 2021;2021:8829158. [Google Scholar]
- 3.Alford AI, Nicolaou D, Hake M, McBride-Gagyi S. Masquelet’s induced membrane technique: Review of current concepts and future directions. J Orthop Res 2021;39:707-18. [Google Scholar]
- 4.McCall TA, Brokaw DS, Jelen BA, Scheid DK, Scharfenberger AV, Maar DC, et al. Treatment of large segmental bone defects with reamer-irrigator-aspirator bone graft: Technique and case series. Orthop Clin North Am 2010;41:63-73. [Google Scholar]
- 5.McClure PK, Abouei M, Conway JD. Reconstructive options for tibial bone defects. J Am Acad Orthop Surg 2021;29:901-9. [Google Scholar]
- 6.Pelissier P, Masquelet AC, Bareille R, Pelissier SM, Amedee J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res 2004;22:73-9. [Google Scholar]
- 7.Khaled A, El-Gebaly O, El-Rosasy M. Masquelet-Ilizarov technique for the management of bone loss post debridement of infected tibial nonunion. Int Orthop 2022;46:1937-44. [Google Scholar]
- 8.Davis RL, Taylor BC, Johnson N, Ferrel JR, Castaneda J. Retrograde versus antegrade femoral bone graft harvesting using the reamer-irrigator-aspirator. J Orthop Trauma 2015;29:370-2. [Google Scholar]
- 9.Cox G, Jones E, McGonagle D, Giannoudis PV. Reamer-irrigator-aspirator indications and clinical results: A systematic review. Int Orthop 2011;35:951-6. [Google Scholar]
- 10.Laubach M, Weimer LP, Bläsius FM, Hildebrand F, Kobbe P, Hutmacher DW. Complications associated using the reamer-irrigator-aspirator (RIA) system: A systematic review and meta-analysis. Arch Orthop Trauma Surg 2023;143:3823-43. [Google Scholar]
- 11.Maruccia M, Vicenti G, Carrozzo M, Caizzi G, Di Summa PG, Moretti B, et al. The free tissue transfer-masquelet-reamer-irrigator-aspirator bone graft orthoplastic approach for lower extremity reconstruction. Plast Reconstr Surg 2022;149:1203e-8. [Google Scholar]
- 12.Esmaeilnejad Ganji SM, Bahrami M, Joukar F. Ilizarov versus AO external fixator for the treatment of tibia open fractures. Iran Red Crescent Med J 2011;13:868-72. [Google Scholar]