This article provides the readers with insights into the clinical manifestations of metallosis in total hip replacement, even when non-metallic bearing surfaces are involved, emphasizing its consideration as a potential differential during the diagnostic process of hip instability.
Dr. Arjun Chakrapani, Flat 8 Balakavi apartments, 8/23 thiru-vi-ka 3rd street, Mylapore, Chennai 600004, Tamil Nadu, India. E-mail: chakrapani.arjun@gmail.com
Introduction: Metallosis which is traditionally associated with Metal-on-Metal (MoM) hip arthroplasty can occur with other bearing surfaces too, posing diagnostic challenges. They can be asymptomatic or present with local and systemic symptoms. This article reports a case of metallosis in a total hip replacement (THR) with metal on polyethylene (PE) articulation who presented with dislocation. It also reviews the pathology and various presentations of metallosis following hip arthroplasty.
Case Report: A 35-year-old female patient presented 4 years after a left THR with recurrent dislocation. It was an uncemented prosthesis with metal on PE articulation. Serology and radiological investigations were done to evaluate for infection, implant loosening, implant malposition, etc. The femoral stem appeared to be in varus malposition. She was posted for revision surgery with a pre-operative plan to change the femoral stem and head if necessary. Intraoperative signs of local metallosis were noticed. Debridement was done along with the change of the femoral stem and bearing surface to ceramic on PE. Metallosis was also later confirmed by the histopathological report. The patient has been symptom-free during the 2-year follow-up period.
Conclusion: Metallosis can occur even in non-MoM articulations and a high degree of clinical suspicion is required to detect the same preoperatively. Classical signs of metallosis can often be absent in the early disease and subtle signs of instability must be looked out for even in the absence of obvious misalignment in radiographic assessment. Metallosis when combined with malposition or malalignment can be more detrimental. If detected early before osteolysis and periarticular soft tissue damage sets in, a complete revision of all the implant components and abductor damage can be avoided. In suspected cases, a lower threshold should be adopted for sending blood and joint aspirates for cobalt-chromium levels.
Keywords: Metallosis, total hip arthroplasty, hip dislocation, pseudotumor, aseptic lymphocytic vasculitis-associated lesion, adverse local tissue reactions lesion.
Total hip arthroplasty has become the standard treatment for advanced hip osteoarthritis with more than a million patients being operated on every year [1]. In the last few decades, there has been an explosion of literature regarding the various possible complications of the procedure. One such complication is metallosis which can include a subset of conditions such as adverse local tissue reactions (ALTR), pseudotumors, and aseptic lymphocytic vasculitis-associated lesions [2]. Metallosis was originally thought to be a complication of metal-on-metal (MoM) prostheses alone but there has been increasing evidence that this is also found in other non-metallic bearing surfaces [3, 4, 5]. They can present with pain, swelling, local signs, systemic consequences, or more often as asymptomatic with or without instability and dislocation, which makes the diagnosis challenging [3]. We present a case of metallosis in a metal-on polyethylene (MoP) prosthesis that presented with hip dislocation with minimal other symptoms and was incidentally found only during revision surgery for instability.
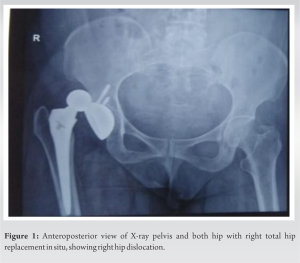
A 35-year-old female patient presented 4 years after a right total hip arthroplasty done elsewhere with a posterior dislocation following trivial trauma. It was a cementless prosthesis, with metal-polyethylene (PE) articulating surfaces. She was managed conservatively with closed reduction and maintenance under traction for a few days. She presented with a redislocation 2 weeks later (Fig. 1 and 2).
After the closed reduction, further evaluation was done with serology, radiographs, and computer tomography (CT) scanning. The femoral stem appeared to be in varus malposition. There was no other malalignment or malposition of the prosthesis components (including acetabular cup inclination and anteversion) or gross aseptic loosening noticed. Physical examination revealed no local signs of inflammation or infection. There was a mildly elevated erythrocyte sedimentation rate and C-reactive protein but no leukocytosis.
The hip joint aspirate was clear and showed no obvious signs of metallosis. She was scheduled for a revision of total hip arthroplasty with a plan to change the femoral stem and the head if necessary. There were intraoperative findings of local tissue necrosis, grayish-black discoloration of the joint capsule, and periarticular soft tissues (Figs. 3a and b).
There was no gross damage to the abductors. There was minimal wear or damage to the trunnion. The pigmented and abnormal tissue sample was sent for histopathological evaluation and culture sensitivity. Debridement of the damaged tissue was performed along with a thorough wash. The femoral component was replaced. The 32–0 size metallic head was replaced with a ceramic head of 32 size diameter +4 mm offset to increase stability and reduce post-operative redislocation chances (Fig. 4).
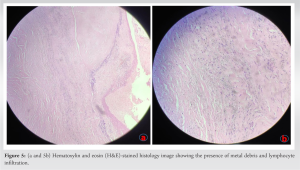
The histopathology report revealed the presence of metal particulate debris with a collection of lymphocyte-dominant inflammatory cells suggesting the diagnosis of localized metallosis (Fig. 5a and b). Culture revealed no growth. The patient has not presented with any complaints in this 2-year follow-up period.
Metallosis was first described in MoM THAs in the 1970s. In MoM, the rate of metal particle debris production is much higher compared to other bearing surfaces even after the initial run-in wear. The general incidence of metallosis in all total hip arthroplasties is around 5.3% [6]. With the shift toward ceramic and PE bearings, the incidence of metallosis is decreasing. However, metallosis can occur even with non-metallic components if there is abnormal MoM contact. Hjorth et al. through their evaluation of 148 THAs using metal artifact-reducing sequences-magnetic resonance imaging (MARS MRI) scans claimed that the incidence of metallosis in MoP articulations was no less than MoM. They inferred that these cases were missed often due to subtle presentations and less gross local and systemic manifestations. Metal nanoparticles are generated by wear between the bearing surfaces in MoM, .that is, mode one wear, whereas by wear between the bearing and non-bearing surfaces (e.g., the femoral head against the acetabular shell after the PE liner has worn out) or two non-bearing surfaces in non-MoM arthroplasties (e.g., trunion and head junction), .that is, mode two and mode four, respectively. These cobalt-chromium nanoparticles of size 50–500 nm are processed by T lymphocytes. This can trigger an inflammatory cascade leading to a benign inflammatory mass (pseudotumor) or soft-tissue necrosis. This cycle of continued excessive production of metal debris and local tissue response can lead to adverse local soft-tissue response (ALTR) with the main concern being the damage to abductors and other soft tissue [7]. This metal debris has access to the functional joint space and can lead to osteolysis at the bone-metal interface. These metal ions when in excess of 7 ppb (parts per billion) can cause systemic effects. The clinical presentation of this pathology has a constellation of signs and symptoms such as hip pain, instability, squeaking sounds, lurching due to abductor weakness, osteolysis leading to implant failure, and palpable swellings or collections in the hip and pelvic region. Systemic manifestations range from headaches, cognitive changes, hemolytic anemia, peripheral neuropathies, and other neuromuscular abnormalities [3]. A growing realization is that a significant number of patients suffering from ALTRs secondary to metallosis may be asymptomatic [3]. However, even these patients have always been found to have either subtle or rarely gross radiological signs such as an eccentrically placed femoral head, cloud sign, bubble sign, and signs of component loosening [8]. Certain factors predispose patients to excessive component wear such as female sex, obesity, MoM articulations, large femoral head, thin PE liner, harsh methods of manufacturing and sterilization of PE, and component malposition in terms of acetabular cup inclination, cup and stem anteversion [7]. Campbell et al. have described the diagnosis of metallosis as one by exclusion and also proposed a systematic approach to making the diagnosis in an arthroplasty patient with unexplained hip pain or instability [9]. This includes radiographs to exclude aseptic implant loosening, fracture, and CT scanning for assessment of cup anteversion and inclination, and femoral stem anteversion. Hematologic testing and microbiological assessment of joint aspirate are needed to rule out infection. In cases of suspected metal toxicity, serum metal concentrations can be measured. If cobalt and chromium levels >7 ug/mL, further investigation is needed with a MARS MRI to analyze soft tissue for mass or potential fluid collection which would require management with surgical intervention [10]. Debridement, replacement with non-metal bearing surfaces, and revision in the presence of malposition, loosening are the ideal management with abductor damage warranting a more extensive reconstruction. Lash et al. described a series of 10 patients with hip dislocations in MoP hip arthroplasties. All 10 patients underwent revision arthroplasty for instability and dislocation with no suspicion of metallosis before surgery, similar to our patient. Trunnion corrosion was found in all patients, causing varying degrees of pseudotumor and abductor mechanism damage. This study drew attention to the fact that metallosis could easily be missed and detected only intraoperatively much like our patient. Metallosis detected in cases with a malposition or misalignment can be a result of accelerated formation of metal debris leading to more destruction of the capsule, abductors, osteolysis, etc. In such situations, it is important to address the underlying cause of the problem along with the change to a non-metal-bearing surface.
Metallosis can occur even in non-MoM articulations and a high degree of clinical suspicion is required to detect the same preoperatively. Classical signs of metallosis can often be absent in the early disease and subtle signs of instability must be looked out for even in the absence of obvious misalignment in radiographic assessment. Metallosis when combined with malposition or malalignment can be more detrimental. If detected early before osteolysis and periarticular soft-tissue damage sets in, a complete revision of all the implant components and abductor damage can be avoided in cases with no abnormalities of component position or alignment. A lower threshold should be adopted for sending blood and joint aspirates for metal levels in suspected cases.
Metallosis is a clinical entity that is being increasingly recognized as a complication of total hip arthroplasty in non-metal bearing surfaces and must be suspected as such by the surgeon investigating hip pain and instability in non-MoM THA post-operative patients even when not presenting with any of the classic clinical or radiological findings.
References
- 1.Mastel M, Boisvert A, Moore R, Sutherland F, Powell J. Metallosis following hip arthroplasty: Two case reports. J Med Case Rep 2022;16:115. [Google Scholar]
- 2.Ude CC, Esdaille CJ, Ogueri KS, Ho-Man K, Laurencin SJ, Nair LS, et al. The mechanism of metallosis after total hip arthroplasty. Regen Eng Transl Med 2021;7:247-61. [Google Scholar]
- 3.Oliveira CA, Candelária IS, Oliveira PB, Figueiredo A, Caseiro-Alves F. Metallosis: A diagnosis not only in patients with metal-on-metal prostheses. Eur J Radiol Open 2015;2:3-6. [Google Scholar]
- 4.Hjorth MH, Mechlenburg I, Soballe K, Roemer L, Jakobsen SS, Stilling M. Higher prevalence of mixed or solid pseudotumors in metal-on-polyethylene total hip arthroplasty compared with metal-on-metal total hip arthroplasty and resurfacing hip arthroplasty. J Arthroplasty 2018;33:2279-86. [Google Scholar]
- 5.Cipriano CA, Issack PS, Beksac B, Della Valle AG, Sculco TP, Salvati EA. Metallosis after metal-on-polyethylene total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2008;37:E18-25. [Google Scholar]
- 6.Roth TD, Maertz NA, Parr JA, Buckwalter KA, Choplin RH. CT of the hip prosthesis: Appearance of components, fixation, and complications. Radiographics 2012;32:1089-107. [Google Scholar]
- 7.Daniel J, Holland JF, Quigley L, Sprague S, Bhandari M. Pseudotumors associated with total hip arthroplasty. J Bone Joint Surg Am 2012;94:86-93. [Google Scholar]
- 8.Paydar A, Chew FS, Manner PA. Severe periprosthetic metallosis and polyethylene liner failure complicating total hip replacement: The cloud sign. Radiol Case Rep 2007;2:115. [Google Scholar]
- 9.Campbell P, Shimmin A, Walter L, Solomon M. Metal sensitivity as a cause of groin pain in metal-on-metal hip resurfacing. J Arthroplasty 2008;23:1080-5. [Google Scholar]
- 10.Frederick MA, James HB, editors. Campbell’s Operative Orthopaedics. Amsterdam: Elsevier; 2021. p. 285. [Google Scholar]