Tibial diaphyseal fracture fixation with humerus intramedullary nailing in patients with short limb length is one of the possible options with satisfactory outcomes.
Dr. Akshay Phupate, Department of Orthopaedics, Seth G.S Medical Collage and K.E.M Hospital, Mumbai, Maharashtra, India. E-mail: akshayphupate2@gmail.com
Introduction: There have been very few cases of intramedullary (IM) nailing for tibia shaft fracture using a humerus nail. We present to you a unique case of humerus nail used in tibia shaft fracture in a short-stature patient.
Case Report: A 26-year-old female, was brought to our emergency room, she sustained trauma to her left leg while she was walking on the road hit by an automobile (pedestrian injury) with complaints of pain and swelling in her left leg. She has a family history of short stature. X-ray suggested of left tibia diaphyseal fracture with a left calcaneum fracture (undisplaced). Preoperatively, tibia length came out to be 22 cm. The shortest tibia nail available is 26 cm. Hence, the plan was to do IM humerus nailing. Closed reduction with internal fixation was done with a similar method as in tibia nailing. Titanium nail of size 8 mm × 22 cm was used. In the humerus nail, the bend is lateral, which was kept posteriorly as Herzog bends in the tibia nail. Postoperatively, patient was given below knee slab with nil weight bearing for 6 weeks.
Conclusion: Use of IM humerus nailing in tibia diaphyseal fracture fixation is possible. It provides rotational stability, leg length control, early mobilization and is also available in smaller sizes. Tibial fracture fixation with humeral nails in patients with short limb lengths is one of the possible options with satisfactory outcomes.
Keywords: Tibia fracture, humerus nail, short limb, nailing.
Tibial shaft fractures are the most common long-bone fracture, accounting for 1.9% of all fractures [1,2]. While conservative management with closed manipulation and cast immobilization has been the mainstay of treatment for minimally displaced, low-energy tibia fractures [3] in certain circumstances, surgical stabilization may be required. Potential surgical indications include open fractures, “floating knees” (concomitant femur and tibia fracture), patients with compartment syndrome, and unstable fracture patterns that fail closed treatment. Intramedullary nailing (IMN) is the gold standard for the treatment of displaced tibial shaft fractures in adults [4,5]. Recently, there have been a few studies that reported that the small intramedullary (IM) interlocking nail, such as IM humeral nail, could be used in femoral fixation in normal adolescent patients due to the advantages of the entry point lateral to the tip of greater trochanter resulting in avoiding iatrogenic vascular injury and being the IM locking device with a smaller diameter and shorter length than a conventional femoral nail which was appropriate for small-sized adolescent femoral anatomy [6]. There have been very few cases of IM humerus nailing in tibia diaphyseal fracture. This study is a rare case report of an IM humerus nailing done in a tibia diaphyseal fracture. We discuss the patient’s clinical presentation, pre-operative planning, surgical intervention, and post-operative course.
A 26-year-old female was brought to our emergency room, she had sustained trauma to left leg while she was walking on the road hit by an automobile (pedestrian injury) with complaints of pain and swelling in her left leg. She has a family history of short stature.
On inspection, the patient’s overall health was satisfactory. The patient was conscious and aware of time, place, and person. She had stable vitals on presentation. Upon clinical examination, swelling and tenderness over the middle part of the left leg and heel were present. Her range of motion was restricted and painful. Deformity and abnormal mobility at the fracture site were presented. On vascular and neurological evaluation, the patient’s extremities were found to be unharmed. She also gave a history of fracture of the same leg tibia and fibula, which was managed conservatively with above knee slab and cast. Radiographic evaluation suggested of left tibia diaphyseal fracture with left calcaneum fracture and old united tibia and fibula fracture (Fig. 1). Pre-operative planning was carried out by measuring tibia length (taken from tibial tuberosity to medial malleolus) came out to be 22 cm (Fig. 2). The shortest tibia nail length available was 26 cm.
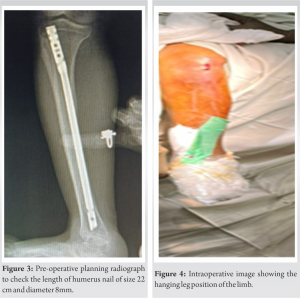
In preoperatively, planning X-ray was done with a humerus nail of size 22 cm and of diameter 8 mm (Fig. 3). Calcaneum fracture was undisplaced so was planned to conserve it with below knee (BK) slab.
Surgical procedure
Following a pre-operative assessment, the patient was scheduled for closed reduction with internal fixation was done with a similar method as in tibia nailing in a hanging leg position (Fig. 4). Incision was taken from the inferior pole of the patella to tibial tubercle. Entry was taken with awl medial to lateral tibial spine and confirmed under fluoroscopy in both anteroposterior (AP) and lateral views.
Reaming with 7 mm, 8 mm, and 9 mm number solid reamers was done. A titanium nail of size 8 mm × 22 cm (as preoperatively planned) was done. In the humerus nail, the bend is laterally which was kept posteriorly as Herzog bends in the tibia nail. Proximal locking was done with the help of a jig and distal locking was done with a perfect circle technique with a leg in extension AP screw was put. The reduction was checked under C-arm in AP and lateral views.
Postoperatively on vascular and neurological evaluation, the patient’s extremities were found to be unharmed and were given BK slab with limb elevation for calcaneum fracture (Fig. 5).
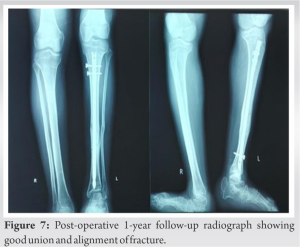
In post-operative rehabilitation started on day 1 with knee range of motion, quadriceps strengthening exercises as per pain tolerance and mobilized nil weight bearing with help of walker (Fig. 6). Suture removal was done after 2 weeks and patient was mobilized with full weight bearing after 6 weeks. Post-operative 1 year patient is fully weight-bearing also the fracture has united without any complication (Fig. 7).
The introduction of IMNs revolutionized fracture care in the years following the World War II enabling early patient mobilization and weight-bearing [7]. While multiple long bones are amenable to rigid IMN, a contraindication to this technique in the tibia is a patient with open physis with substantial growth remaining. For these instances, flexible IMNs have been developed which spare the physis and can be inserted distant from the fracture site allowing the fracture site to not have to be opened in most circumstances. Multiple studies have now shown good outcomes with this technique for unstable tibia fractures in the pediatric population [8-10]. There are several drawbacks to flexible IMNs compared with rigid locked IMNs, including the lack of construct rigidity which allows potential loss of reduction, a short period of immobilization is frequently required, and weight-bearing is typically delayed for 4–6 weeks. IM humerus nails are indicated in fractures of the humerus shaft. Comparing tibia IMN to humerus IMN (Fig. 8). Herzog’s bend proximally in the tibia is 11° while in the humerus is 4°. There have been very few cases of humerus nail used in tibia shaft fracture [11].
- First, the humeral nail compared to conventional tibial IMN, is available in smaller diameters and shorter lengths and is more suitable for these patients’ tibial anatomy with narrow medullary canal and short limb
- Second, the humeral nail has a narrow width and a lateral bend at its proximal end which allows its insertion with minimal physeal violation, and 90–100° of the cephalomedullary angle for the proximal locking blade or screw
- Third, because of the interlocking property of the nail, the humeral nail would offer superior biomechanical benefits than gold standard rush pin fixation as it provides rotational stability and leg length control.
However, there were also limitations for using a humeral nail for tibial reconstruction in these patients but are minimal, like proximal tibial physeal damage cannot be avoided, which predisposes for future growth disturbances of the proximal tibia. The absence of Herzog’s bend limits the nail entry to a more proximal and posterior area of the tibial articular surface.
This is the first study to show the use of IMN for tibia shaft fracture using a humerus nail in patients with short limb length is possible. It provides rotational stability, leg length control, early mobilization and is also available in smaller sizes. Therefore, we concluded that tibial fixation with humeral nails in patients with short limb length is one of the possible options with satisfactory outcomes.
Tibial diaphyseal fracture fixation with humerus IMN in patients with short limb length is one of the possible options with satisfactory outcomes.
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 2006;37:691-7. [Google Scholar]
- 2.Russell TA. Fractures of the tibial diaphysis. In: Orthopaedic Knowledge Update: Trauma 1 1. Rosemont, Il: American Academy of Orthopaedic Surgeons; 1996. p. 171-9. [Google Scholar]
- 3.Thompson GH, Wilber JH, Marcus RE. Internal fixation of fractures in children and adolescents. A comparative analysis. Clin Orthop Relat Res 1984;188:10-20. [Google Scholar]
- 4.Bhandari M, Guyatt G, Tornetta P 3rd, Schemitsch EH, Swiontkowski M, Sanders D, et al. Randomized trial of reamed and unreamed intramedullary nailing of tibial shaft fractures. J Bone Joint Surg Am 2008;90:2567-78. [Google Scholar]
- 5.Bong MR, Kummer FJ, Koval K, Egol KA. Intramedullary nailing of the lower extremity: Biomechanics and biology. J Am Acad Orthop Surg 2007;15:97-106. [Google Scholar]
- 6.Sa-ngasoongsong P, Saisongcroh T, Angsanuntsukh C, Woratanarat P, Mulpruek P. Using humeral nail for surgical reconstruction of femur in adolescents with osteogenesis imperfecta. World J Orthop 2017;8:735-40. [Google Scholar]
- 7.Duan X, Al-Qwbani M, Zeng Y, Zhang W, Xiang Z. Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database Syst Rev 2012;1:CD008241. [Google Scholar]
- 8.Kc KM, Acharya P, Sigdel A. Titanium elastic nailing system (TENS) for tibia fractures in children: Functional outcomes and complications. JNMA J Nepal Med Assoc 2016;55:55-60. [Google Scholar]
- 9.Heo J, Oh CW, Park KH, Kim JW, Kim HJ, Lee JC, et al. Elastic nailing of tibia shaft fractures in young children up to 10 years of age. Injury 2016;47:832-6. [Google Scholar]
- 10.Sankar WN, Jones KJ, David Horn B, Wells L. Titanium elastic nails for pediatric tibial shaft fractures. J Child Orthop 2007;1:281-6. [Google Scholar]
- 11.Pradeep H, Pillai AG, Ravikumar AS. Humerus nail for tibial reconstruction in adolescent with osteogenesis imperfecta - A rare surgical case report. Indian J Orthop Surg 2022;8:236-9. [Google Scholar]