Combining cancellous screws and ethibond suture augmentation can be an effective treatment modality for posterior cruciate ligament avulsion fracture of tibia, which demands very little instrumentation and can be reproduced in remote places as well, with the non-availability of arthroscopic instruments to produce equivalent results.
Dr. Nadir Z Shah, Department of Orthopedics, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India. E-mail: nadirzshah@gmail.com
Introduction: The posterior cruciate ligament (PCL) is a vital structure in knee biomechanics, and its avulsion fractures present a unique challenge. This prospective cohort study was conducted at Grant Government Medical College and JJ Hospital, Mumbai, aimed to assess the clinical outcomes of open reduction and internal fixation (ORIF) utilizing cancellous screws and ethibond suture augmentation for PCL avulsion fractures. PCL avulsion fractures often result from traumatic incidents, such as road traffic accidents, and are associated with complications if left untreated.
Materials and Methods: Patients aged 20–45 years with isolated PCL avulsion fractures, confirmed by clinical and radiological assessments, were included. Seven eligible patients underwent ORIF, and outcomes were evaluated through clinical assessments, radiological imaging, and the Lysholm knee scoring system. Follow-ups were conducted for a mean time of 13.2 months, assessing stability, range of motion, and complications.
Results: The study demonstrated a mean post-operative Lysholm score of 93.8, significantly improved from the pre-operative score of 49.6. Post-operative knee flexion averaged 125.2°. Fracture healing was observed in all cases, and complications were minimal. The study provides evidence of the effectiveness of ORIF with ethibond suture augmentation for PCL avulsion fractures.
Conclusion: The study concludes that the proposed surgical technique yields positive outcomes, including enhanced knee functionality, successful fracture healing, and minimal complications. This approach, combining cancellous screws and ethibond suture augmentation, presents a promising option for the management of PCL avulsion fractures, contributing to the diverse landscape of effective treatment modalities.
Keywords: PCL avulsion fracture, Ethibond suture augmentation, Open reduction and internal fixation (ORIF)
The posterior cruciate ligament (PCL) stands as a crucial intra-articular yet extra-synovial structure within the knee joint, playing a pivotal role in preventing posterior translation of the tibia and providing essential rotational stability [1]. Injuries to the PCL can manifest as either intrasubstance tears or avulsion fractures at the femoral or tibial insertion points [2]. The biomechanics and stability of the knee joint are significantly influenced by the central role of the PCL, acting as the primary deterrent against posterior tibial translation (PTT) [1, 2]. While PCL avulsion fractures are relatively rare, they are typically associated with dashboard injuries, where a force directed posteriorly impacts the pretibial area in a flexed knee position [2]. The mechanism of injury parallels that of intrasubstance PCL tears, with road traffic accidents (RTA), particularly motorcycle injuries, being the most common mode. In addition, dashboard strikes against the proximal tibia with a flexed knee, and injuries resulting from falls from height contribute to the occurrence of PCL avulsion fractures [2, 3]. Notably, associated injuries are frequently observed in PCL avulsion cases, with meniscus injuries reported in 16.8% of patients, and other ligamentous injuries reported in 19% of patients [2]. The classification of PCL avulsion fractures includes type I (non-displaced), type II (upward displacement of the posterior aspect of the avulsed tibial bone fragment), and type III (totally displaced avulsed bone fragment) [4]. Non-operative treatment may be considered for cases with a displacement <5 mm [5]. Non-operative treatment of isolated PCL injuries may have good outcomes but also lead to knee problems and lower fracture union rates. Operative treatment of PCL avulsion fractures can reduce PTT and improve fracture healing [3, 5]. The complications of untreated PCL avulsion fractures include knee joint instability, secondary osteoarthritis (OA), and non-union [2]. Hence, surgical intervention is recommended for fractures exhibiting significant displacement or posterior translation of the tibia. Surgical management options for PCL avulsion fractures involve arthroscopic repair or open reduction and internal fixation (ORIF) [2, 5]. While arthroscopic repair is minimally invasive, it presents challenges in fixation and reduction compared to ORIF, but recent literature shows the comparable outcome of both arthroscopic and open techniques [2, 6, 7]. This study aims to assess the clinical outcomes of ORIF using direct bony fixation with a cancellous screw and augmentation with a pull-out ethibond suture with endobutton for PCL avulsion fractures of the tibia and to compare them with other fixation methods reported in the literature. Selected for its ability to provide stable fixation and facilitate early post-operative rehabilitation across various fracture types, this technique is investigated in the context of a patient cohort at GGMC and JJH, Mumbai, Maharashtra, India, between December 2021 and June 2022.
Study design
-
- This prospective cohort study aimed to investigate the outcomes of surgical management in patients with isolated PCL avulsion fractures
- -The study was conducted at the Department of Orthopedics, Grant Government Medical College, and JJ Hospital, Mumbai, from December 2021 to June 2022.
Inclusion and exclusion criteria
-
- Participants were recruited from both the Outpatient Department and Emergency Department.
Inclusion criteria
The following criteria were included in the study:
-
- Patients aged 20–45 years
- Injuries with a duration of <3 months
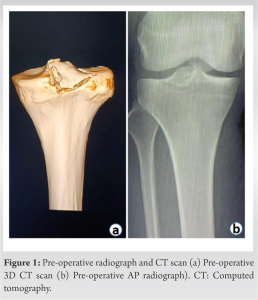
- Isolated PCL avulsion fractures were confirmed by clinical and radiological assessments (Fig. 1).
Exclusion criteria
The following criteria were excluded from the study:
-
- Patients outside the specified age range
- Injuries older than 3 months
- Patients with multi-ligament injuries or meniscal involvement
- Medical conditions or contraindications preventing surgical intervention
- Patients unwilling or unable to comply with the rehabilitation protocol.
Clinical assessment
- Patients underwent a comprehensive clinical assessment, including an evaluation for the posterior sag sign, dial test at 90° knee flexion, and posterior drawer test.
Radiological evaluation
- Anteroposterior and lateral radiographs were taken to confirm the PCL avulsion injury.
- Magnetic resonance imaging was performed to assess the associated ligament injuries to the knee.
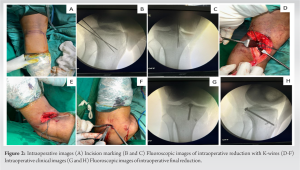
Surgical procedure (Fig. 2)
-
- Approach: A standard posterior approach to the knee was utilized, with appropriate exposure of the tibial spine fracture
- Augmentation with ethibond pull-through sutures and fixation with CC screw
- Before fixation with CC screws, ethibond sutures were passed through the insertion of the PCL over the avulsed fragment. This helped to reduce and hold the fragment while putting the K-wire for provisional fixation
- Fixation with CC screw: Following provisional fixation with the K-wire, a suitable size CC screw was chosen and carefully inserted across the fracture site to achieve stable fixation
- Additional Ethibond passage: After fixation with the screw, current ethibond sutures along with one more added ethibond thread were passed through the tunnel created with a 4-mm drill bit. 4-mm tunnel was drilled from the posterior to anterior from the insertion of PCL directed anteromedially by flexing knee 40°–50° in the prone position. The tunnel was drilled manually in such a way that the exit point was roughly ground 4 cm distal to joint line and 2 finger breath medial to the tibial tuberosity. This technique offers an advantage, that is, no advanced instrumentation is required (no PCL Jig). Subsequently, ethilon was then passed from anterior to posterior to pull all threads through the tunnel, akin to Ranawat suturing
- PCL tensioning: The tensioning of the ethibond sutures was performed with the knee in 90° of flexion and applying an anterior drawer force. This method provided additional support and reinforcement to the CC screw fixation. The sutures were manually pulled and tied over a suspensory fixation button placed anteromedially on the tibia
- Additional Time required: Additional time required after screw fixation average 15 min (ranges from 12 to 19 min)
- Final assessment:
The reduction, fixation, and augmentation were confirmed intraoperatively using fluoroscopy to ensure proper alignment and stability of the fracture fixation construct. Clinical confirmation was also obtained by performing the posterior drawer test.
Post-operative rehabilitation
- The patient was immobilized in a long knee brace for 3 weeks
- Patients started range of motion (ROM) exercise from 3-week onward, 30° every week gradually increasing to >90° at the end of 6 weeks
- A long knee brace was continued for stabilization of the knee in the first 6 weeks for weight-bearing walking.
Follow-up
-
- Monthly follow-ups for the first 3 months, followed by assessments every 3 months for a minimum of 12 months
- Initially, a monthly radiograph is taken to assess any early loss of reduction or any early complications during the rehabilitation phase. Followed by X-ray at 6 months and 12 months to see consolidation. Hence, the patients could resume high-intensity work (Figs. 3 and 4)
Outcome measures
- The Lysholm knee scoring system was utilized to calculate the final functional outcome at the end of the 1-year follow-up.
Data analysis
- Descriptive statistics summarized patient demographics
- Statistical analysis was performed using descriptive statistics (mean and standard deviation).
Ethical considerations
- Informed consent was obtained from all participants
- The study protocol received approval from the Institutional Review Board.
Limitations
- Acknowledged potential limitations, including the study’s single-center nature and the small sample size.
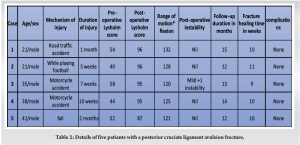
In a study involving five patients, the average age was found to be 31.2 years, with a standard deviation of 8.06 years. RTA emerged as the most common cause of injury, resulting in a mean presentation time of 4.4 weeks, with a standard deviation of 2.11 weeks. Pre-operative Lysholm scores averaged 49.6 with a standard deviation of 6.63. Following surgical intervention, the post-operative Lysholm score significantly improved, reaching an average of 93.8 with a standard deviation of 3.46, indicating substantial improvement in knee functionality. A 6-week analysis revealed patients demonstrating a ROM exceeding 90°. The study had a comprehensive follow-up period, averaging 13.2 months, during which all fractures are united. The average time for fracture healing ranged from 8 to 12 weeks. At the final follow-up, patients exhibited an average flexion of 121.9° ± 10.4° with full extension. While in one patient clinically, mild instability (1+) was confirmed through the drawer test and stress view X-ray (12 months postoperatively). The primary advantage of this technique is the additional stability provided to the PCL by combining ORIF screw fixation with ethibond suture augmentation. This method ensures strong and rigid fixation with minimal hardware, reducing the risk of screw loosening or pullout. Furthermore, this technique allows fixation without the use of advanced instruments (PCL jig). In summary, the study demonstrated positive surgical outcomes with effective fracture healing, improved knee functionality, and minimal complications in the majority of cases.
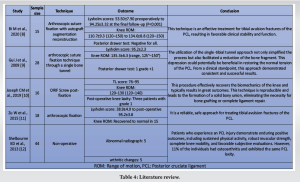
The purpose of this study was to evaluate the clinical outcomes and complications of ORIF CC screw and augmentation with ethibond suture for the treatment of PCL avulsion fracture. The main findings of this study were that ORIF CC screw and augmentation with ethibond suture achieved excellent knee function, stability, and satisfaction in patients with PCL avulsion fracture, with a low rate of complications and no revision surgery requirement. This study demonstrated that ORIF CC screws and augmentation with ethibond suture are a feasible and effective technique for the management of PCL avulsion fractures. ORIF CC screw and augmentation with ethibond suture have several advantages over other treatment modalities for PCL avulsion fracture. It combines the benefits of ORIF screw with PCL augmentation gives additional stability and provides strong and rigid fixation with minimal hardware. ORIF screws provide stable fixation and allow early mobilization, while the augmentation of PCL soft tissue provides strong and rigid fixation with minimal hardware, which reduces the risk of hardware irritation and failure. Thereby, enhances stability and prevents screw loosening or pullout by augmenting the fixation with ethibond suture, which is a non-absorbable and high-strength suture material. In a comprehensive review of studies focusing on treatment outcomes for tibial avulsion fractures of the PCL, various techniques were investigated, each presenting distinct advantages. Bi et al. (2020) demonstrated that arthroscopic suture fixation with autograft augmentation reconstruction significantly improved clinical stability, as reflected in Lysholm scores rose from 53.50 ± 7.90 preoperatively to 94.25 ± 3.32 at the final follow-up, along with positive changes in knee ROM and negative posterior drawer test results [8]. Gui et al. (2009) showed a single-tibial tunnel technique, simplifying the procedure and enhancing bony fragment depression, resulting in a notable Lysholm score of 95.2 ± 2.3 [9]. Joseph et al. (2019) employed an ORIF screw fixation technique, reporting a restoration of knee biomechanics with a predominantly excellent outcome and bony union without the need for extensive reconstruction [10]. Zhu et al. (2015) advocated for arthroscopic fixation, achieving a remarkable improvement in Lysholm scores from 38.9 ± 4.9 to 95.2 ± 3.8, and full knee ROM recovery in the majority of patients [11]. Shelbourne et al. (2013) provided a non-operative perspective, revealing good long-term outcomes in terms of activity levels, strength, and subjective scores, but with a noteworthy 11% occurrence of OA and persistent PCL laxity [12]. Overall, these studies highlight the diversity of effective approaches for managing delayed PCL avulsion fractures, each with its own unique benefits and considerations, compiled their findings in the following Tables 1, 2, 3, and 4. Our study has some limitations that should be acknowledged. First, a small sample size, hence the results may not be generalizable or conclusive. Second, this study did not include a control group, which may have been helpful for the comparison of this study with other standard modalities. Future studies should address these limitations by conducting randomized, controlled trials with larger sample sizes and longer follow-up periods.
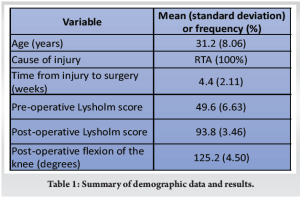
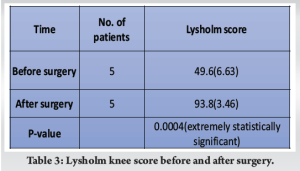
This study evaluated the feasibility and effectiveness of ORIF using CC screw and ethibond suture augmentation for PCL avulsion fractures. The study followed up with the patients for an average of 13.2 months and found that all fractures healed successfully. The patients had a significant increase in their Lysholm score (from 49.6 to 93.8) and satisfactory knee flexion (125.2° on average). The technique improved knee function, stability, and satisfaction, as well as reduced complications and revision rates Therefore, this technique is a promising option for PCL avulsion fracture management, especially in remote areas with the unavailability of advanced arthroscopic instruments. Moreover, further studies with larger sample sizes and randomized controlled trials are needed.
This study explores a technique combining cancellous screws and Ethibond suture augmentation to treat posterior cruciate ligament (PCL) avulsion fractures of the tibia. it also highlights a method that requires minimal instrumentation, making it practical for remote settings. The technique aims to provide stable fixation and facilitate early rehabilitation, offering a promising alternative to more instrument or technical skills requiring surgical procedures
References
- 1.Donno L, Galluzzo A, Pascale V, Sansone V, Frigo CA. Walking with a posterior cruciate ligament injury: A musculoskeletal model study. Bioengineering (Basel) 2023;10:1178. [Google Scholar]
- 2.Katsman A, Strauss EJ, Campbell KA, Alaia MJ. Posterior cruciate ligament avulsion fractures. Curr Rev Musculoskelet Med 2018;11:503-9. [Google Scholar]
- 3.Wang D, Graziano J, Williams RJ 3rd, Jones KJ. Nonoperative treatment of PCL injuries: Goals of rehabilitation and the natural history of conservative care. Curr Rev Musculoskelet Med 2018;11:290-7. [Google Scholar]
- 4.White EA, Patel DB, Matcuk GR, Forrester DM, Lundquist RB, Hatch GF 3rd, et al. Cruciate ligament avulsion fractures: Anatomy, biomechanics, injury patterns, and approach to management. Emerg Radiol 2013;20:429-40. [Google Scholar]
- 5.Gopinatth V, Mameri ES, Casanova FJ, Khan ZA, Jackson GR, McCormick JR, et al. Systematic review and meta-analysis of clinical outcomes after management of posterior cruciate ligament tibial avulsion fractures. Orthop J Sports Med 2023;11:23259671231188383. [Google Scholar]
- 6.Gawande V, Badge A. Clinical effectiveness of arthroscopy-assisted fixation in the treatment of avulsed posterior cruciate ligament injuries. Cureus 2023;15:e50152. [Google Scholar]
- 7.Hooper PO 3rd, Silko C, Malcolm TL, Farrow LD. Management of posterior cruciate ligament tibial avulsion injuries: A systematic review. Am J Sports Med 2018;46:734-42. [Google Scholar]
- 8.Bi M, Zhao C, Chen J, Hong Z, Wang Z, Gan K, et al. Arthroscopic suture fixation with autograft augmentation reconstruction for delayed tibial avulsion fractures of the posterior cruciate ligament. Orthop J Sports Med 2020;8:2325967120944047. [Google Scholar]
- 9.Gui J, Wang L, Jiang Y, Wang Q, Yu Z, Gu Q. Single-tunnel suture fixation of posterior cruciate ligament avulsion fracture. Arthroscopy 2009;25:78-85. [Google Scholar]
- 10.Joseph CM, Gunasekaran C, Livingston A, Chelliah H, Jepegnanam TS, Boopalan PR. Outcome of screw post fixation of neglected posterior cruciate ligament bony avulsions. Injury 2019;50:784-9. [Google Scholar]
- 11.Zhu W, Lu W, Cui J, Peng L, Ou Y, Li H, et al. Treatment of tibia avulsion fracture of posterior cruciate ligament with high-strength suture fixation under arthroscopy. Eur J Trauma Emerg Surg 2017;43:137-43. [Google Scholar]
- 12.Shelbourne KD, Clark M, Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med 2013;41:1526-33. [Google Scholar]