Skin necrosis following total knee arthroplasty may be successfully treated with eschar preservation, oral antibiotics, an antimicrobial silver dressing, and allowing the wound to heal by secondary intention.
Dr. Gary L Ulrich, Research Fellow, Department of Orthopaedic Surgery and Sports Medicine, University of Kentucky College of Medicine, 740 S. Limestone, Suite K401, Lexington, KY 40536-0284. E-mail: garyulrich94@gmail.com
Introduction: Skin necrosis following total knee arthroplasty (TKA) represents a rare, but serious complication that can lead to deep infection. In the setting of a lateral release performed during TKA, the incised retinaculum unveils a potential pathway to the joint should the superficial skin and tissue be compromised. Thus, the conventional treatment of debridement in this setting may risk infection to the joint, whereas eschar preservation may serve as a biological protective barrier to prevent infection.
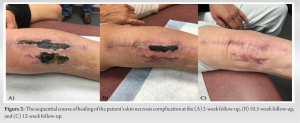
Case Report: We present a patient with end-stage tricompartmental knee osteoarthritis who underwent a TKA with a concomitant lateral release. The patient developed necrosis in two distinct areas measuring 14 cm × 2 cm along the length of the primary TKA incision, and 7 cm × 4 cm laterally. The patient was treated with eschar preservation, oral doxycycline, an antimicrobial silver dressing, and allowed to heal by secondary intention. The patient’s skin necrosis healed fully at 12-week post-operatively, and they have had a successful TKA outcome at 5 years.
Conclusion: Eschar preservation, oral doxycycline, an antimicrobial silver dressing, and allowing the wound to heal by secondary intention may represent a viable, less invasive treatment for skin necrosis following TKA with lateral release.
Keywords: Skin necrosis, wound complication, eschar preservation, total knee arthroplasty.
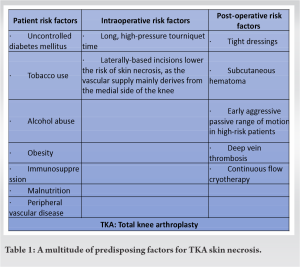
Skin necrosis following total knee arthroplasty (TKA) represents a rare yet serious post-operative complication of TKA. It can lead to extended hospital stays, increased cost, decreased healing expectancy, and surgical interventions, which ultimately may require removal of the prosthesis due to deep infection [1-3]. A multitude of predisposing factors for TKA skin necrosis has been described (Table 1) [4]. The conventional treatment options for TKA skin necrosis include local wound care, debridement, and soft-tissue coverage with muscle or skin grafting. A major determinant in choosing the treatment method is whether the wound is superficial (confined to the dermis and subcuticular tissue) or deep to the fascia [5]. In the setting of a superficial wound, previous literature has advocated for the complete debridement of TKA necrotic eschar [6]. However, performing debridement is under the assumption that there is no underlying sinus tract or violation of tissue creating an avenue to the joint, as would be in case of a lateral release. In this scenario of a lateral release, eschar preservation may actually aid in the healing process as it forms a biological barrier to infection and protects the underlying avenue to the joint. The eschar preservation can then further be supplemented with antibiotics and antimicrobial dressings, and lead to successful healing by secondary intention. We report a case of a primary TKA with a lateral release that developed acute skin necrosis occurring in two distinct areas measuring the size of 14 cm × 2 cm along the length of the primary TKA incision and 7 cm × 4 cm laterally. These necrotic areas were successfully treated with eschar preservation, oral doxycycline, and an antimicrobial silver dressing, and allowed to heal by secondary intention. The patient has had a successful TKA outcome at 5-year postoperatively to date.
A 57-year-old female with a history of tobacco use presented with severe right knee pain that had been occurring for approximately 2 years. The patient also presented with difficulty ambulating not only due to the pain but also complicated by a history of femoral rotational malunion through an intramedullary rodding for a right distal 1/3 diaphyseal femur fracture at age 12. Physical examination of the right knee revealed a 20° external rotatory distal femoral deformity affecting her gait. In addition, there was a 10° flexion contracture, slight varus alignment, and the ability to only flex the knee to 70°. Moreover, a previous scar from the femoral rodding was noted at the posterolateral aspect of the knee. Radiographs demonstrated severe degenerative tricompartmental arthritis with complete loss of joint space and large marginal osteophytes (Fig. 1a-c). The patient had previously attempted activity modification, physical therapy, and corticosteroid injections, but these were unsuccessful, leading to the decision to proceed with elective TKA.
A TKA was performed through a 14 cm anterior midline incision and medial parapatellar arthrotomy. Intraoperatively, it was found that the lateral retinaculum was extremely tight and scarred onto the distal femur, which resulted in the lateral gutter having to be recreated through extensive dissection. Furthermore, due to the severe tightness of the extensor mechanism, a lateral release was performed through incision and extensive electrocautery from the superolateral aspect of the patella to the tibia.
For the femoral component preparation, the normal transepicondylar axis was used for rotational alignment despite the patient’s external rotatory distal femoral deformity since the extensor mechanism had been tracking centrally. However, to address the rotational malunion of the extremity, the tibial component was placed in an external rotation to match the external rotation of the femoral component. Finally, the medial collateral ligament was found to be deficient and was reconstructed with a posterior tibial tendon allograft. During final range of motion checks following closing the arthrotomy with #1 Vicryl suture, the patella would begin to track medially and then snap into the trochlear groove. Thus, the lateral retinaculum was repaired with #1 Vicryl suture which corrected this problem as the patella then glided smoothly within the trochlear groove throughout a range of motion. Final closure was then completed with #0 Vicryl to close the deep fat, 2–0 Vicryl for the dermis skin, and then 3–0 subcuticular Monocryl running suture superficially. A sterile dressing was applied and all wound edges were viable at the time of closure.
At 2-week follow-up, the patient returned with two distinct areas of skin necrosis with one area measuring 7 cm × 4 cm located laterally and another area 14 cm × 2 cm located along the length of the primary TKA incision (Fig. 2a). Given that the surgery involved a lateral release, the decision was made to treat the skin necroses with nonoperative management, which involved eschar preservation, doxycycline antibiotic prophylaxis, and a silver impregnated wound dressing. Over close subsequent follow-up visits, the wound demonstrated progressive healing with secondary intention. At no point was the skin necrosis debrided; rather, the skin necrosis was preserved and allowed to come off naturally. Furthermore, per the protocol and given the patient’s stiffness and flexion contracture preoperatively, the patient was enrolled in physical therapy.
At the 10.5-week follow-up, the lateral skin necrosis had come off completely and revealed healthy healed skin underneath (Fig. 2b). The central skin necrosis was still healing and was raised relative to its healthy skin edges as the wound healed up from its depths by secondary intention. At this point, the patient was switched to trimethoprim/sulfamethoxazole (Bactrim) from doxycycline. At the 12-week follow-up, the central skin necrosis had come off and also revealed healthy healed skin underneath (Fig. 2c). At this time, the silver-impregnated wound dressing was discontinued, but the patient was kept on prophylactic trimethoprim/sulfamethoxazole (Bactrim) for an additional 3 months. The implants were found to be stable, well-aligned, and showed no signs of infection at 1-year post-operatively (Fig. 3a-c). The patient went on to have a successful TKA outcome that at a 5-year follow up had no pain, a functional range of motion of 0-120°, and improved gait from a pre-operative arthritic state. Moreover, there were no complications of infection, stiffness, or loosening throughout the patient’s course at the point of 5-year follow-up.
Skin necrosis represents a potential complication of TKA that is critical to address to achieve a successful TKA outcome. Depending on the clinical circumstance, the treatment of skin necrosis is often algorithmically approached with treatment options including local wound care, debridement, and soft tissue coverage with muscle or skin grafting [5]. While debridement has conventionally been viewed as a standard of care, our case highlights that skin necrosis does not necessarily have to be debrided to achieve a successful outcome. Rather, eschar preservation may actually assist in the skin healing process as theoretically, it forms a biological barrier to infection. To the best of our knowledge, this is the first case in the literature pursuing eschar preservation as a primary treatment. Interestingly, our patient’s specific case guided our treatment decision to preserve the eschar. Because our patient underwent a lateral release, the retinaculum incision had created an avenue to the joint. Thus, when our patient developed skin necrosis, we felt that debriding the eschar would risk exposing this underlying avenue of the joint to the outside world and increase the risk of joint infection. As a result, the eschar was preserved to maintain a barrier and protect the joint from infection. Moreover, the eschar barrier was supplemented with doxycycline and a silver-impregnated wound dressing to protect any infectious breach of the eschar barrier, especially at the interface between the eschar and the healthy skin. The necrosis healed by secondary intention and the underlying healing skin eventually naturally displaced the necrotic skin and caused it to inherently debride itself with no complications. Our patient had multiple risk factors for the development of skin necrosis, including diabetes mellitus, a history of smoking, and previous surgeries at the site. Considering our patient’s lateral skin necrosis area, our patient’s previous orthopedic surgical history of a pediatric IMN procedure involving lateral incisions likely contributed to the skin necrosis. Moreover, the scar tissue that occurred from this pediatric surgery resulted in the need for extensive dissection laterally during the TKA, which included recreating the lateral gutter and performing a lateral release with incision and extensive electrocautery as the lateral retinaculum was scarred and adherent to the lateral femur. It has been demonstrated that previous scars represent a risk factor for skin necrosis after TKA [7]. Maintaining a distance of 8cm from the previous incision has been recommended to avoid skin necrosis, but this needs to be balanced with the access to underlying structures required for surgery [8]. Other reports have challenged the 8 cm rule concluding that the previous scar can be ignored without concern for skin necrosis [9, 10]. While the impact of previous scars on skin necrosis is debated, our case supports findings that previous incisions increase the risk of skin necrosis following TKA. While we report only a single case, we feel eschar preservation may represent another viable, less invasive option for treating skin necrosis. Given the size and multiple areas of our patient’s skin necrosis, our patient’s case typically would have been considered for not only debridement but also potentially soft tissue flap procedures. However, the morbidity of these procedures and the shared decision-making process guided our treatment plan to pursue eschar preservation with close follow-up, which led to a successful outcome.
Skin necrosis represents a serious complication following TKA. Eschar preservation with prophylactic antibiotic measures may represent a viable, less invasive option for treating skin necrosis following TKA with the concomitant lateral release. Each patient case should be assessed holistically to determine the appropriate treatment for skin necrosis following TKA.
Regarding skin necrosis following TKA, eschar preservation with prophylactic antibiotic measures represents a less invasive treatment option, especially in the setting of lateral release where conventional debridement risks exposure of the joint to infection.
References
- 1.Garbedian S, Sternheim A, Backstein D. Wound healing problems in total knee arthroplasty. Orthopedics 2011;34:e516-8. [Google Scholar]
- 2.Panni AS, Vasso M, Cerciello S, Salgarello M. Wound complications in total knee arthroplasty. Which flap is to be used? With or without retention of prosthesis? Knee Surg Sports Traumatol Arthrosc 2011;19:1060-8. [Google Scholar]
- 3.Vince K, Chivas D, Droll KP. Wound complications after total knee arthroplasty. J Arthroplasty 2007;22:39-44. [Google Scholar]
- 4.Sarman H, Muezzinoglu US, Memisoglu K, Baran T. Vacuum‐assisted closure for skin necrosis after revision total knee arthroplasty. Int Wound J 2016;13:843-7. [Google Scholar]
- 5.Amin NH, Speirs JN, Simmons MJ, Lermen OZ, Cushner FD, Scuderi GR. Total knee arthroplasty wound complication treatment algorithm: Current soft tissue coverage options. J Arthroplasty 2019;34:735-42. [Google Scholar]
- 6.Patella V, Speciale D, Patella S, Moretti B, Pesce V, Spinarelli A. Wound necrosis after total knee arthroplasty. Orthopedics 2008;31:807. [Google Scholar]
- 7.Ries MD. Skin necrosis after total knee arthroplasty. J Arthroplasty 2002;17:74-7. [Google Scholar]
- 8.Simons MJ, Amin NH, Scuderi GR. Acute wound complications after total knee arthroplasty: Prevention and management. J Am Acad Orthop Surg 2017;25:547-55. [Google Scholar]
- 9.Van Zyl AA, van der Merwe JF, Snyman FP. Do previous scars around the knee matter in total knee arthroplasty? Orthop Proc 2003;85B(SUPP 2):144. [Google Scholar]
- 10.Yeganeh A, Moghtadaei M, Ghaznavi A, Tavakoli N, Soleimani M, Cheraghiloohesara S, et al. The distance between new and previous incisions does not affect skin necrosis in total knee arthroplasty: A parallel-randomized controlled clinical trial. BMC Surg 2022;22:350. [Google Scholar]