Accurate diagnosis of soft-tissue chondromas requires a multidisciplinary approach to differentiate them from other soft tissue entities and guide effective treatment
Dr. Vijay Kumar Jain, Department of Orthopaedic Surgery, Atal Bihari Vajpayee Institute of Medical Sciences, Dr. Ram Manohar Lohia Hospital, New Delhi – 110 001, India. E-mail: drvijayortho@gmail.com
Introduction: Soft-tissue chondromas are rare, benign cartilaginous tumors predominantly affecting the extremities, often diagnosed in middle-aged individuals without a clear sex predilection. Despite their benign nature, these tumors can pose significant diagnostic challenges due to their slow growth, asymptomatic nature, and potential for mimicking other soft-tissue tumors.
Case Report: We report a case of a 27-year-old male with an 8-year history of a progressively enlarging mass on the dorsal aspect of the second toe of the left foot, leading to pain, difficulty in walking, and wearing shoes. Initial clinical examination revealed a firm, non-tender swelling with hypoesthesia over the affected area. Radiographic findings suggested a soft-tissue mass with stippled calcification, while magnetic resonance imaging indicated a large altered signal intensity lesion abutting but not arising from the bone. Fine needle aspiration cytology hinted at a benign mixed tumor/chondroid syringoma. An excisional biopsy was performed, revealing a well-circumscribed tumor with lobules of mature hyaline cartilage, consistent with a diagnosis of soft-tissue chondroma. Post-operative period recovery was uneventful except for local flap necrosis which was managed with skin grafting. There was no recurrence at the 1-year follow-up.
Conclusion: Soft-tissue chondromas, while rare and benign, can significantly impact patients’ quality of life. Correct diagnosis, involving a comprehensive evaluation and histopathological confirmation, is crucial for effective management and prevention of unnecessary interventions. This case adds valuable insight into the clinical presentation, diagnostic challenges, and management strategies for soft-tissue chondromas.
Keywords: Chondroma, chondroid syringoma, cartilaginous, soft tissue.
Either the soft tissues or the bone may develop chondromas. Known as extraskeletal chondromas, soft-tissue chondromas are uncommon, slowly growing benign cartilaginous tumors that affect the hands and feet. These tumors predominantly involve the middle-aged group with no sex predilection. Although these tumors do not have any connection with the underlying bone however may also be found in the joint capsules of the knee, elbow, and other joints [1, 2]. Repeated microtrauma has been reported to be responsible for its occurrence. Clinically most of the soft-tissue chondromas are asymptomatic unless they enlarge enough to cause pressure symptoms, difficulty in wearing shoes, discomfort during gait, and cosmetic deformity [3, 4]. These chondromas are predominantly composed of mature hyaline cartilage with or without endochondral ossification [5, 6]. Herein, we report a rare case of soft-tissue chondroma in a 27-year-old male who presented with a mass in his left foot over the past 8 years with difficulty in walking and wearing shoes. The patient was managed with the excision of the mass with no recurrence at 1-year follow-up.
A 27-year-old male presented with a slowly progressive mass in the dorsal aspect of the second toe of the left foot of around 8-year duration. Initially, the swelling was painless until 6 months before he attended the outpatient department when he started to feel increasing pain in his left foot while walking for long distances. The pain increased in intensity on wearing shoes and progressively due to the large size of the swelling he was unable to wear shoes comfortably. The patient had a mild tingling sensation and numbness in the overlying skin associated with mild difficulty in walking and pain on flexion at the interphalangeal joint of second toe. However, there was no history of trauma. Furthermore, family history and personal history were irrelevant. General clinical assessment was normal.
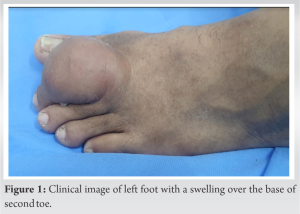
Locally, there was a firm, fixed, non-tender swelling on the dorsal aspect of second toe. The swelling was 5 × 4 cm in size with well-defined borders. It was not attached to the overlying skin (Fig. 1). Distal circulation was normal. Neurological examination showed mild hypoesthesia over the skin overlying the swelling. Routine hematological and biochemical tests were within normal limits. The radiograph of the foot with anteroposterior, lateral, and oblique views showed a soft-tissue shadow of swelling along with stippled calcification and sclerosis and extrinsic cortical pressure erosion of the cortex of the proximal phalanx of the second toe (Fig. 2).
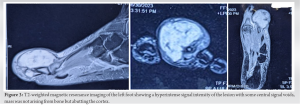
Magnetic resonance imaging (MRI) of the left foot showed a large altered signal intensity lesion of size approximately 56 × 48 mm with multiple septations seen in the first and second web space and dorsum of the foot. The lesion was predominantly involving the skin and subcutaneous plane with surrounding edema. This well-circumscribed globular soft-tissue mass was hyperintense on T2-weighted with some central signal voids, mass was not arising from bone but abutting the cortex (Fig. 3). The possibility of organized infective collection was suggested. Fine-needle aspiration cytology (FNAC) of the mass revealed abundant chondromyxoid ground substance with occasional foci of bland spindle-shaped cells and round to oval plump cells with eccentric nuclei suggesting a possibility of a benign mixed tumor/chondroid syringoma.
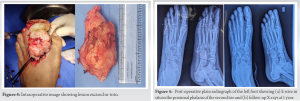
Since the patient was suffering from left foot pain with a progressive inability to wear his left shoe, he was scheduled for an excisional biopsy of the mass under spinal anesthesia with exsanguination of the limb using a pneumatic tourniquet. Intraoperatively, the mass was found to be hard, lobulated, greyish white situated over the dorsal aspect of the second metatarsal head and proximal and middle phalanx of the second toe. The swelling was excised completely (Fig. 4).
The underlying bone was scalloped, the capsule of the interphalangeal joint was repaired and a k-wire was inserted intramedullary for stabilization of the joint (Fig. 5). On the 3rd post-operative day, the skin flap at the operative site got necrosed with blackish discoloration; then, it was managed with debridement of the skin flap and autologous split-thickness skin grafting which healed uneventfully (Fig. 6).
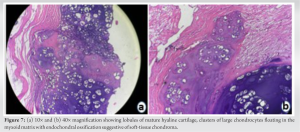
At post-operative 4 weeks, k-wire was removed and the patient was allowed to do full weight bearing. Histological assessment of the resected specimen showed a well-circumscribed tumor with lobules of mature hyaline cartilage. Clusters of large chondrocytes floating in the myxoid matrix with endochondral ossification were seen (Fig. 7). The diagnosis was consistent with soft-tissue chondroma. The patient was followed up regularly in the outpatient department. The last follow-up period was 1 year.
In many instances, soft-tissue chondromas of the foot are initially asymptomatic due to their slow growth rate. As the tumor enlarges over time, individuals may start experiencing difficulties in shoe fitting, along with pain during physical activities, and a sense of localized soreness and tenderness. Given its relatively infrequent clinical presentation, this condition often goes unrecognized in its early stages. The case in question underscores this point, with the patient seeking medical advice only after enduring walking discomfort for nearly 8 years. Clinically, this type of tumor can resemble other soft-tissue masses including lipomas, myositis, chondromatosis, chondrosarcomas, and dermal tumors [6-9], complicating its diagnosis. The diagnostic challenge is further exacerbated by the variable appearances on standard X-rays, which depend on the calcification level of the tumor [4, 10]. Hence, accurate identification of this rare benign chondroid anomaly through imaging is crucial to prevent misdiagnosis as a more aggressive lesion or a primary synovial disorder. Various hypotheses have been posited regarding the origins of extraskeletal chondroma [2, 6]. It is thought to either stem from pluripotent cells within the tenosynovium or through metaplasia within the tendon sheath [2, 11, 12]. Observations by Dahlin and Salvador [13] in a cohort of 70 patients, and Chung and Enzinger [14] in a cohort of 104 patients, revealed that these tumors are benign, predominantly appear in the distal extremities, and can be histologically confused with chondrosarcomas. Furthermore, extraskeletal chondromas can be categorized into two groups based on whether they contain mature hyaline cartilage or immature chondroblasts, with the former group possibly showing fibrosis, hemorrhage, necrosis, calcification, ossification, or granuloma formation.
The key differentiating features for conditions commonly considered in the differential diagnosis of soft-tissue chondroma [15, 16] are as follows,
- Synovial chondromatosis: This condition is associated with the synovium and may present with multiple nodules within a joint, unlike the solitary nodules of soft-tissue chondromas
- Juxtacortical (periosteal) chondroma: These lesions are characterized by their attachment to the bone, which is not a feature of soft-tissue chondromas
- Soft-tissue chondrosarcoma: Greater cellularity, cytological atypia, and mitotic activity are seen in chondrosarcomas, distinguishing them from the limited atypia and mitotic figures of soft-tissue chondromas
- Tenosynovial chondromatosis: Similar to synovial chondromatosis but involves the tendon sheaths
- Nuchal fibrocartilaginous tumor: Typically occurs in the posterior neck region
- Myxochondroid metaplasia: Presents with a mix of myxoid and cartilaginous tissue
- Fibro-osseous pseudotumor of the digit: A reactive lesion often related to trauma; and
- Calcifying aponeurotic fibroma: A benign fibrous tumor that commonly calcifies, usually seen in children and young adults.
When evaluating a patient with a suspected soft-tissue chondroma, it is crucial to consider these differential diagnoses and utilize clinical presentation, imaging, and histological examination to arrive at an accurate diagnosis. Marginal resection is the standard treatment for soft-tissue chondromas, with a recurrence rate of about 15–20%. Cytopathologic examination in this case indicated a possibility of benign mixed tumor due to the presence of mature hyaline cartilage and myxoid stroma which is also a feature of chondroma. However, the resected specimen did not show any epithelial or myoepithelial component, thereby ruling out the diagnosis of benign mixed tumor or chondroid syringoma. Another morphologic differential diagnosis is synovial chondromatosis; however, there is no overlying synovial epithelium observed over the cartilaginous lobules. While FN1 rearrangements are observed in synovial chondromatosis, they are not specific and can also be seen in soft-tissue chondromas. Although juxtacortical chondroma also shows the same morphology, the absence of attachment to the bone surface and covering by attenuated periosteum excluded the diagnosis of juxtacortical/periosteal chondromas. Soft-tissue chondrosarcomas including myxoid and mesenchymal types were excluded due to the absence of typical cord-like patterns of tumor cells in the former and the biphasic nature of the latter, characterized by undifferentiated round malignant cells and lobules of mature hyaline cartilage. In addition, the foot is not a typical site for either of these tumors. The soft-tissue chondromas can clinically present as a dermal mass in the toe. The cytology of the present case is suggestive of a tumor of dermal origin, the chondroid syringoma a rare benign mixed tumor of the adnexal origin which creates a dilemma regarding the correct diagnosis. MRI and FNAC findings were not consistent toward a single diagnosis, while they ruled out the presence of malignant lesions. However, as the diagnosis was different in radiology and cytology, we decided to do an excisional biopsy of the lesion. An excisional biopsy was done in our case which confirmed the diagnosis and is the definitive management option. Local recurrence rates of around 15–18% have been reported in the literature [12]. Hence, close follow-up is needed to look for recurrence. Our patient has not shown signs of recurrence at the 1-year follow-up.
The soft-tissue chondromas are rare benign lesions. Although mainly symptomatic difficulty in gait and wearing shoes can be the complaints when they involve toes. The correct pre-operative diagnosis is important to rule out malignant pathology.
Timely recognition and multidisciplinary diagnostic evaluation are key to effectively managing soft-tissue chondromas, preventing misdiagnosis, and ensuring optimal patient outcomes.
References
- 1.Mocellin S. Extraskeletal chondroma. In: Soft Tissue Tumors : A Practical and Comprehensive Guide to Sarcomas and Benign Neoplasms. Berlin: Springer International Publishing; 2021. p. 305-6. [Google Scholar]
- 2.Kakamad FH, Salih AM, Hassan MN, Mohammed SH, Abdullah AM. A rare presentation of soft tissue chondroma: A case report. Int J Surg Case Rep 2020;72:426-8. [Google Scholar]
- 3.Vohra RR, Haseeb M, Owais M, Bokhari SF, Yaseen K. Heavily ossified soft tissue chondroma of plantar foot and the significance of radiological imaging: A case report. Cureus 2023;15:e37914. [Google Scholar]
- 4.Bahnassy M, Abdul-Khalik H. Soft tissue chondroma: A case report and literature review. Oman Med J 2009;24:296-9. [Google Scholar]
- 5.Xue S, Chen Y, Haneke E. Soft tissue chondroma: A possible diagnosis of single-digit nail clubbing. Dermatol Surg 2022;48:143. [Google Scholar]
- 6.Mariano A, Fallat LM. A rare benign soft-tissue chondroma in the plantar foot: A case report. Foot Ankle Surg Techn Rep Cases 2022;2:100105. [Google Scholar]
- 7.Adaletli I, Laor T, Yin H, Podberesky DJ. Extraskeletal chondroma: Another diagnostic possibility for a soft tissue axillary mass in an adolescent. Case Rep Orthop 2011;2011:309328. [Google Scholar]
- 8.Khandeparkar SG, Joshi A, Khande T, Kesari M. A rare case of giant soft tissue chondroma of the wrist: A cytopathological study with review of the literature. J Cytol 2014;31:40-3. [Google Scholar]
- 9.Benradi L, El Haissoufi K, Haloui A, Bennani A, Aichouni N, Belahcen M. Soft tissue chondroma of the plantar foot in a 14-year-old boy: A case report. Int J Surg Case Rep 2022;90:106688. [Google Scholar]
- 10.Ghrea M, Mathieu G, Apoil A, Soubrane P, Dumontier C, Sautet A. Soft-tissue chondroma of the hand: A case report and analysis of diagnostic procedures for extra-osseous cartilaginous lesions of the hand. Rev Chir Orthop Reparatrice Appar Mot 2003;89:261-5. [Google Scholar]
- 11.Cardia R, Favazzi CM, Fenga D, Rosa MA, Ieni A. A large extraskeletal chondroma: An unusual location in the lower extremity, huge extraskeletal chondroma: An unusual localization in the leg. J Orthop Case Rep 2019;9:74-7. [Google Scholar]
- 12.Tantawy HF, Morsy MM. Benign soft tissue chondroma of the foot. Egypt J Radiol Nuclear Med 2018;49:128-30. [Google Scholar]
- 13.Dahlin DC, Salvador AH. Cartilaginous tumors of the soft tissues of the hands and feet. Mayo Clin Proc 1974;49:721-6. [Google Scholar]
- 14.Chung EB, Enzinger FM. Chondroma of soft parts. Cancer 1978;41:1414-24. [Google Scholar]
- 15.Hung YP, Nielsen GP. Chondroma of soft parts. In: van Krieken JH, editor. Encyclopedia of Pathology. Cham: Springer International Publishing; 2019. p. 1-5. [Google Scholar]
- 16.Pathology Outlines - Soft Tissue Chondroma. Available from: https://www.pathologyoutlines.com/topic/softtissueeskchondroma.html [Last accessed on 2024 Jun 04]. [Google Scholar]