Synovial chondromatosis with valgus deformity, leading to secondary osteoarthritis at in young age, is a correctable cause of knee pain and can be treated with total synovectomy and wedge osteotomy, even in a Wilson’s disease patient, as copper is osteogenic that helps in healing of the osteotomy site.
Dr. Amit Kumar, Department of Orthopaedics, All India Institute of Medical Sciences, Kalyani, West Bengal, India. E-mail: amit.ortho@aiimskalyani.edu.in
Introduction: Wilson’s disease is an autosomal recessive condition where excessive amount of copper accumulates in the body, especially in the liver, brain, and eyes. It is caused by a mutation in the ATP7B gene on chromosome 13. In 25–30% of patients, joint involvement occurs at the later course of disease; osteoarthritis being the commonest manifestation. Synovial chondromatosis (SC) is a benign metaplasia which occurs in the synovial membrane and it results in the formation of intra-articular loose bodies (LB), but its occurrence in a patient of Wilson’s disease has not yet been reported in medical literature.
Case Report: A young male in his 30s, a diagnosed case of Wilson’s disease on maintenance therapy of d-penicillamine, zinc, trientine, and lithium presented to the hospital with restriction of movement at the knee joints and a valgus deformity. Examination showed firm to hard globular swellings which were partly mobile around the knee joint. The Magnetic Resonance Imaging (MRI) findings were suggestive of a SC after which the patient underwent corrective surgery and debridement and removal of the LB and a histopathology report confirmed the diagnosis. The patient was followed up at 12 weeks and was found to have pain-free movements with minimal support. His 24-h urinary copper excretion was found to be within normal limits and his maintenance therapy was optimized. The patient was initiated on speech therapy for his persistent slurring of speech and psychiatric counseling for rehabilitation in social and personal life. The patient was advised for 6 monthly follow-up.
Conclusion: This case summarizes the unique presentation of SC with genu valgum in a patient of Wilson’s disease and hence warrants a keen eye for the physician and orthopedician alongside osteoarthritis; which has been widely reported in Wilson’s disease, thus providing an opportunity for early correction of valgus deformity of the subject.
Keywords: Wilson disease, synovial chondomatosis, genu valgum, osteoarthritis.
Wilson’s disease is an autosomal recessive condition where excessive amounts of copper accumulate in the body, especially in liver, brain, and eyes. It is caused by a mutation in the ATP7B gene on chromosome 13. In 25–30% of patients, joint involvement occurs at the later course of disease; osteoarthritis being the commonest manifestation. Synovial chondromatosis (SC) is a benign metaplasia which occurs in the synovial membrane and it results in the formation of intra-articular loose bodies (LB), but its occurrence in a patient of Wilson’s disease has not yet been reported in medical literature.
A male in his early 30s had initially presented with choreoathetoid movements at the age of 15 years, to a neurology center. He had delayed developmental milestones, slurred speech with drooling of saliva, and abnormal posturing of hands. He is a 2nd born child of non-consanguineous parentage with normal birth and no significant family history was found in consecutive three generations. Ophthalmological findings revealed the presence of Kayser-Fleischer (K-F) rings bilaterally (Fig. 1).
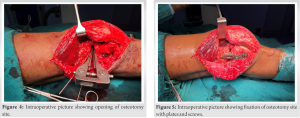
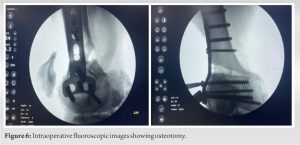
On examination, he had dystonia of all four limbs, dystonia of tongue along with dysarthria. He had dragging of the lower limbs while walking. All deep tendon reflexes were increased and bilateral plantars were flexor. Investigation showed deranged liver enzymes, low levels of ceruloplasmin, thrombocytopenia, and elevated 24-h urinary copper. Leipzig’s score was 4. His diagnosis was confirmed to be Wilson’s disease after his genetic workup was found to be positive for a mutation of ATP7B on chromosome 13. The patient was started on d-penicillamine and zinc acetate. Trientine was started in view of choreoathetoid movements and lithium to alleviate his neuropsychiatric symptoms. The patient confirmed that he was compliant with the treatment since the initiation of the same. The patient now came to us with an inability to walk and flex the right knee, attributed to the LB in the knee, restricting the movements along with valgus deformity of the right knee. On examination, multiple firm to hard swellings were found in the right knee joint. Radiographs demonstrated the presence of multiple radio-opacities in the right knee along with valgus deformity and osteoarthritic changes (Fig. 2). Ultrasound of the right knee showed effusion with few LB in the knee joint. Further confirmation by MRI of the right knee joint showed extensive knee joint effusion with multiple LB in the suprapatellar bursa, posterior recess, and Hoffa’s fat pad, suggestive of SC, along with Kellgren Lawrence Grade III osteoarthritis of tibiofemoral joint, more in the lateral compartment. On a scanogram the Hip-Knee-Ankle (HKA) angle was found to be 196° on the right side and 188° on the left. The differentials of this case might include pigmented vilonodular synovitis, hemangiomas of the synovium, or lipoma arborescens which can be distinguished from each other based on imaging and microscopic appearance. The patient underwent total synovectomy of the right knee and excision of the LB, along with distal femoral lateral open wedge osteotomy to correct the valgus deformity and subsequent iliac crest bone grafting followed by plate fixation (Fig. 3-6).
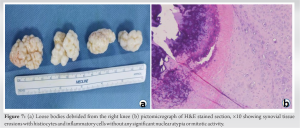
Synovial fluid cytology was negative for malignancy. Multiple irregular pieces of greyish tissue (largest 10 cm in its greatest axis) and multiple hard nodules (largest 3.5 cm) were excised (Fig. 7a). Histopathology showed pieces of tissue with erosions of the lining synoviocytes which were infiltrated by inflammatory cells admixed with histiocytes, suggestive of SC (Fig. 7b).
Synovial fluid cytology was negative for malignancy. Multiple irregular pieces of greyish tissue (largest 10 cm in its greatest axis) and multiple hard nodules (largest 3.5 cm) were excised (Fig. 7a). Histopathology showed pieces of tissue with erosions of the lining synoviocytes which were infiltrated by inflammatory cells admixed with histiocytes, suggestive of SC (Fig. 7b).
The sections were stained with rhodamine and victoria blue but were found to be negative for copper. The patient gradually improved and at his last follow-up at 16 weeks had a range of motion of 0–120° and his valgus deformity of the knee was corrected significantly. He was able to walk independently with minimal pain. He had persistent slurring of speech for which he was advised speech therapy and psychiatric counseling for rehabilitation in social and personal space.
Our patient presented with choreoathetoid movements, dystonia, dysarthria, and slurring of speech. There can be various possibilities but Wilson’s disease was established by low serum ceruloplasmin, elevated 24-h urinary copper excretion, and slit lamp examination revealing bilateral K-F rings and by genetic studies. Osteopenia and arthropathy are the common radiological features of Wilson’s disease [1]. In general, small and large joint arthropathy occurs and interphalangeal, metacarpophalangeal, wrist, hip, and knee joints are affected. Not only arthropathy, periarticular osteopenia is also associated. Kramer et al., described that the possible explanation of arthropathy is copper and iron deposition in high concentration in the synovial membrane which can be seen by X-ray energy spectroscopy. Recently a cartilage matrix glycoprotein which has homology with ceruloplasmin is described [2]. Osteophytes, sclerosis, subchondral pseudocysts, and bone fragmentation are the typical radiographic findings [3]. In 25–30% of patients, symptomatic joint disease occurs usually after the second decade of life [4]. In this case, there was a valgus deformity with an HKA angle of about 196° on the right knee and 188° on the left. As the patient was asymptomatic on the left side, we proceeded for corrective osteotomy only on the right side (Fig. 8). In planning the corrective osteotomy, we had a few challenges regarding the union of the osteotomy site as the patient was on lithium and the disease itself caused an overload of copper. Literature was searched, and we found that both lithium and copper had osteogenic potential [5]. Progression of union at the osteotomy site in this case indirectly supported the role of the same. The scanogram was repeated at 4 months and the valgus of the right HKA axis was found to be 184° and hence a correction of 12° was achieved (Fig. 9).
In our case, multiple cartilaginous LB were found within the synovium which were compatible with SC on histopathology. SC, a benign metaplasia of synovial membrane, is more common in males, in the third to fifth decade, and mostly involving the knee joint which is seen in our case as well, although occurrences in temporomandibular joint, shoulder, elbow, hip, and ankle have been reported [6, 7]. This can be diagnosed by plain radiographs, computed tomography, or MRI, the latter being a superior modality for its superior soft tissue contrast. Knee can be involved intra-articularly, extra-articularly, or both. It can affect merely the cruciate ligaments to the whole joint as well causing secondary osteoarthritis, in which case it might require a total knee replacement. Although SC causing developmental defects is rare, there are two reports of valgus deformity in SC of the knee joint which is probably due to the uneven increase in vasculature causing synovitis as also seen in our case [8, 9]. Complications might include secondary osteoarthritis, malignant transformation, and recurrence, especially if a partial synovectomy is performed, reported in 7–23% of cases; hence, a total synovectomy is often preferred [8, 10]. The peculiarity of our case is the association of SC in a case of Wilson’s disease. This is probably the first ever reported case in medical literature.
Though rare in its presentation, a patient with Wilson’s disease complaining of chronic painless swelling in the knee; SC should be a differential diagnosis. The imaging appearance and the histopathology reports are sufficient to differentiate it from other causes of intra-articular pathology. Early detection and surgical excision of the LB along with total synovectomy can prevent secondary arthritis and advanced deformity in these patients.
Wilson’s disease also referred to as hepatolenticular degeneration is an autosomal recessive disease that results in impaired activity of intracellular copper transporter ATP7B resulting in its accumulation in vital organs like liver, brain, and cornea. Early diagnosis and management with copper chelating agents such as d-penicillamine and trientine and reducing copper absorption by agents like zinc salts and checking the 24 h urinary copper every 6 months along with renal and liver enzymes is the mainstay of management. Osteopenia and arthritis have been described in patients of WD but SC has never been reported prior. SC can cause developmental deformities like genu valgum at the knee probably due to differential vascularity and at later stages advanced secondary osteoarthritis. Radiological examination and histopathology can clinch the diagnosis. Removal of LB with total synovectomy is the preferable treatment. Both lithium and copper are osteogenic in nature and do not hinder bone healing.
References
- 1.Resnick D, Niwayama G, editors. Crystal induced and related disease. In: Diagnosis of Bone and Joint Disorders. Philadelphia, PA: W B Saunders; 1981. p. 1463. [Google Scholar]
- 2.Kramer U, Weinberger A, Yarom R, Zoldan J, Bahar A, Godoth N. Synovial copper deposition as a possible explanation of arthropathy in Wilson’s disease. Bull Hosp Jt Dis (United States) Winter 1993;52:46-9. [Google Scholar]
- 3.Menerey KA, Eider W, Brewer GJ, Braunstein EM, Schumacher HR, Fox IH. The arthropathy of Wilson’s disease: Clinical and pathological features. J Rheumatol 1988;15:331. [Google Scholar]
- 4.Golding DN, Walshe JM. Arthropathy of Wilson’s Disease: A Study of Clinical and Radiological Features in 32 Patients. Georgia: Atlanta R J Arthritis Foundation; 1988. p. 215. [Google Scholar]
- 5.Tan Z, Zhou B, Zheng J, Huang Y, Zeng H, Xue L, et al. Lithium and copper induce the osteogenesis-angiogenesis coupling of bone marrow mesenchymal stem cells via crosstalk between canonical Wnt and HIF-1α signaling pathways. Stem Cells Int. 2021;2021:6662164. [Google Scholar]
- 6.Dwidmuthe SC, Nemade AS, Agrawal S, Pathak A. Rare case of extra-articular synovial chondromatosis of biceps tendon sheath in 8 years male child-a literature rivew. J Orthop Case Rep 2014;4:33-6. [Google Scholar]
- 7.Santiago T, Mariano C Primary synovial chondromatosis of the ankle joint presenting as monoarthritis. BMJ Case Rep 2013;2013:bcr2013202186. [Google Scholar]
- 8.Dwidmuthe S, Sharma M. A Case report of primary synovial chondromatosis with bilateral genu valgum. J Orthop Case Rep 2017;7:92-5. [Google Scholar]
- 9.Karabila MA, Bardouni A. Chondromatose du genou compliquée d'un genou valgum secondaire avec compression de nerf sciatique poplité externe [Knee chondromatosis complicated by secondary genu valgum with common peroneal nerve compression]. Pan Afr Med J 2016;23:127. [Google Scholar]
- 10.Park JH, Noh HK, Bada LP, Wang JH, Park JW. Arthroscopic treatment for synovial chondromatosis of the subacromial bursa: A case report. Knee Surg Sports Traumatol Arthrosc 2007;15:1258-60. [Google Scholar]