Vascular injury with proximal screw insertion is a rare but potentially dangerous complication with retrograde nail femur fixation.
Dr Ahmad Abdallatif, Department of Orthopaedic Surgery, Worcestershire Royal Hospital,Charles Hastings Way, Worcester, WR5 1DD, United Kingdom. Email: ahmad.abdallatif@nhs.net
Introduction: Retrograde femoral nailing is a frequently performed surgical procedure used to stabilize a supracondylar femur fracture. We are reporting a unique case where the insertion of the anteroposterior interlocking screw of a retrograde nail caused vascular damage. Within the elderly patient population, we anticipate the presence of significant collateral blood vessels, which increases the potential for vascular damage during the insertion of a proximal screw. In this instance, there was bleeding caused by a vascular injury after the insertion of proximal interlocking screws, which necessitated further examination and vascular embolization on the following day. The complexity above necessitates that the author makes adjustments to surgical techniques when inserting proximal screws of a retrograde nail in similar cases.
Case Report: An 82-year-old female patient presented with a right periprosthetic supracondylar femur fracture. The fracture was managed by retrograde nail femur. Vascular injury during proximal anteroposterior screw insertion results in post-operative bleeding and marked hemoglobin drop. The bleeding is managed by computed tomography emergent vascular embolization.
Conclusion: Vascular injury, due to the insertion of a proximal screw, is a rare but potentially dangerous complication that needs a high degree of suspicion to pick up and manage this rare serious complication promptly.
Keywords: Retrograde nail femur, Distal femoral fracture, Vascular injury, Complications.
The incidence of periprosthetic fracture following total knee arthroplasty continues to rise as the number of knee arthroplasty procedures increases. Management of periprosthetic fractures can be complex, with locked compression plating and intramedullary nailing being the most commonly used treatment options [1]. A supracondylar femur fracture is a common injury in the elderly population. Retrograde intramedullary nail fixation is a frequently performed procedure for treating this particular type of fracture. For proximal locking screws, freehand locking remains the most common method [2]. Using the free hand technique may result in inadequate soft-tissue protection, thereby increasing the likelihood of vascular injury. Vascular injury is uncommon during the procedure, especially during the proximal interlocking screw insertion. However, trauma and associated fractures increase the risk of displacing the vascular and nerve systems, increasing the likelihood of such injuries [3]. Due to the use of a small skin incision during surgery, many vascular injuries resulting from the placement of a proximal locking screw often go undetected. This can lead to a potentially life-threatening complication [4]. Handolin et al, reported two cases of arterial vascular injury. In the first case, the bleeding was from one of the anterolateral branches of the deep femoral artery 3 cm above the most proximal locking screws. In the second case, the bleeding was from the main trunk of the deep femoral artery at the level of the drill hole. Embolization with fiber coils was successfully done and the two patients completely recovered [5]. Aydin et al., examined the optimal location for inserting proximal interlocking screws in retrograde nails, focusing on identifying a safe zone. Safe zones are detected at a distance of 1 cm above the LT. At that level, there are no vascular structures at risk within a mediolateral dimension of 32.2 ± 7.7 and a dimension of 37.3 ± 8.4 [6].
An 82-year-old female patient presented to our Accident and Emergency Department with severe pain in her left knee following a mechanical fall. An orthopedic team examined the patient and made a preliminary diagnosis of a peripsthetic suropracondylar femur fracture. The physician requested a radiological investigation in the form of a plain X-ray of the entire femur. The request included all necessary laboratory tests, such as a complete blood count (CBC), kidney function tests (KFT), and coagulation profile (Fig. 1).
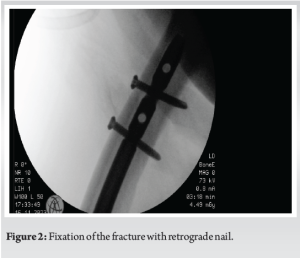
The patient had good mobility and did not require any walking aids before this incident with a history of total knee replacement on the same side about 10 years ago. In addition, the patient did not have any history of significant medical problems. We decided to use a retrograde intramedullary nail to stabilize the fracture. The patient underwent surgery on the following day. We utilized the Synthes retrograde nail with a diameter of 11 mmetres and a length of 38 mmetres. We carried out a minimally invasive procedure, and assisted open reduction, utilizing a cable for provisional fixation. The distal end of the IM nail was secured using a spiral blade and an interlocking screw, while two screws were used to lock the nail at the distal end. Two screws were secured at the level of the lesser trochanter (Fig. 2).
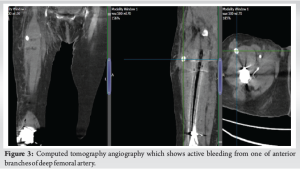
The duration of the operation was 90 min and the estimated amount of blood lost at the end of the procedure was 300 mL. The patient left the operating room and proceeded to the recovery room. On entering the recovery room, we noticed swelling at the location of the proximal interlocking screws. The diagnosis indicated an hematoma located at the level of the proximal screw, primarily caused by the muscular branch. Due to the patient’s stable hemodynamic condition and the presence of a small swelling, it was decided to perform compression and monitor the patient overnight. The following day, there was an increase in swelling accompanied by a decrease in the concentration of hemoglobin from 116 to 92. An urgent request was made for computed tomography angiography, which revealed an injury to one of the anterior branches of the profunda brachii artery with ongoing bleeding (Fig. 3).
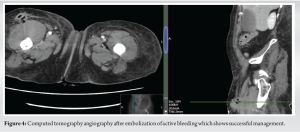
The case has been deliberated on by the radiology and vascular departments, and it has been decided to proceed with embolization under the care of the intensive radiology department using local anesthesia (Fig. 4).
Afterward, the patient was transferred back to the inpatient ward and closely monitored for any changes in vital signs. We administered two units of blood and facilitated mobilization within the limits of the patient’s pain tolerance.
The following day, the patient’s swelling had diminished, and his vital signs had returned to normal. The patient commenced a comprehensive physiotherapy regimen on the 3rd day and was discharged 7-day post-operation. The case was deliberated on the following day during the trauma meeting, and it was also planned to be discussed during the governance meeting. Following this incident, we started to utilize a 5 mL cc syringe tube as a safeguarding cover for the insertion of the proximal locking screw (Fig. 5), as well as for the careful dissection and preservation of the soft tissue following the incision of the skin. Drilling of the proximal screw, as well as insertion of them, will happen through this radiolucent syringe. This technique was described by Perrone et al. in 2020 [7].
The placement of the proximal locking screw is a highly challenging and risky procedure in retrograde femoral nailing. According to Aydin et al. study, it was discovered that the safest distance from the neurovascular structures is 1 cm above the LT level, while the most dangerous distance is 1 cm below the LT level [6]. Additional research has substantiated the absence of a secure area, particularly in elderly patients with significant collateral blood vessels. Numerous studies have been published in the literature to enhance the reliability and simplify this process [8]. Tejwani et al. conducted a study on retrograde femoral nailing to determine the optimal termination point for the nail in terms of biomechanics. They found that the nail should ideally end at or above the LT level. The proximal termination point of the nail plays a crucial role in the prevention of subtrochanteric stress fractures [9]. Another study also assessed the proximity of the locking screw to the neurovascular structures and found, in their examination of cadavers, that the LT and superior positions were deemed safe in relation to the femoral neurovascular structures. However, they identified the area located 4 cm below the LT as potentially hazardous. One possible cause of the vascular damage was the medial penetration of the drill over the femur, resulting in vascular damage. Furthermore, the drill bit not only causes injury through direct penetration but also by encircling the muscles and causing avulsion injuries in the vessels [2, 4]. The primary risk associated with injuries that arise during the application of proximal locking screws is that the closure of the locking mechanism takes place through a small incision, making it difficult to detect any resulting vascular damage initially. Vascular damage following these injuries is observed in the literature, typically indicated by low post-operative hemoglobin levels or thigh swelling [10]. Furthermore, in patients with femoral fractures, the presence of a low post-operative CBC raises concerns about additional pathology, leading to a delay in diagnosis and unnecessary investigations, particularly when surgical procedures and trauma are taken into account. According to the literature, it has been reported that injuries associated with a femoral fracture, such as an acetabulum fracture, can lead to the displacement of neurovascular structures. Consequently, these structures may be harmed when the proximal locking screw is applied [4].
Vascular injury to the femoral branch due to the insertion of a proximal screw is a rare but potentially dangerous complication, particularly in elderly individuals with multiple comorbidities and frailty. This complication requires a high degree of suspicion, particularly if the proximal screws were inserted through a small incision in the skin. The most effective method to prevent this rare complication is by ensuring meticulous protection of the soft tissue. Rapid intervention is crucial in managing this complication, as more observation is often insufficient.
This case presents a very rare but serious complication of vascular injury during retrograde nail femur proximal screw insertion. Careful meticulous soft-tissue approach during insertion and proper timely manner of diagnosis and intervention is crucial in patient management.
References
- 1.Shah JK, Szukics P, Gianakos AL, Liporace FA, Yoon RS. Equivalent union rates between intramedullary nail and locked plate fixation for distal femur periprosthetic fractures - a systematic review. Injury 2020;51:1062-8. [Google Scholar]
- 2.Riina J, Tornetta P, Ritter C, Geller J. Neurologic and vascular structures at risk during anterior-posterior locking of retrograde femoral nails. J Orthop Trauma 1998;12:379-81. [Google Scholar]
- 3.Brown GA, Firoozbakhsh K, Summa CD. Potential of increased risk of neurovascular injury using proximal interlocking screws of retrograde femoral nails in patients with acetabular fractures. J Orthop Trauma 2001;15:433-7. [Google Scholar]
- 4.Barnes CJ, Higgins LD. Vascular compromise after insertion of a retrograde femoral nail: Case report and review of the literature. J Orthop Trauma 2002;16:201-4. [Google Scholar]
- 5.Handolin L, Pajarinen J, Tulikoura I. Injury to the deep femoral artery during proximal locking of a distal femoral nail--a report of 2 cases. Acta Orthop Scand 2003;74:111-3. [Google Scholar]
- 6.Aydin M, Surucu S, Ersin M, Ekinci M, Yilmaz M. Determination of the safest level and screw length for the proximal locking screw in retrograde femoral nailing. Jt Dis Relat Surg 2023;34:69-74. [Google Scholar]
- 7.Perrone MP, Dickherber J, Strelzow J. Use of novel and inexpensive radiolucent soft tissue protector for insertion of proximal locking screws in femoral retrograde intramedullary nailing. J Clin Orthop Trauma 2020;11:S663-6. [Google Scholar]
- 8.Collinge CA, Koerner JD, Yoon RS, Beltran MJ, Liporace FA. Is there an optimal proximal locking screw length in retrograde intramedullary femoral nailing? Can we stop measuring for these screws? J Orthop Trauma 2015;29:e421-4. [Google Scholar]
- 9.Tejwani NC, Park S, Iesaka K, Kummer F. The effect of locked distal screws in retrograde nailing of osteoporotic distal femur fractures: A laboratory study using cadaver femurs. J Orthop Trauma 2005;19:380-3. [Google Scholar]
- 10.Coupe KJ, Beaver RL. Arterial injury during retrograde femoral nailing: A case report of injury to a branch of the profunda femoris artery. J Orthop Trauma 2001;15:140-3. [Google Scholar]