This article addresses the challenge of positioning a below-knee amputee on an orthopedic traction table, compares various techniques, and proposes an effective non-invasive method for patients who cannot use the inverted boot technique or invasive methods due to healing issues
Dr. Igor Gossuin, Department of Orthopedic Surgery and Traumatology, Centre Hospitalier Universitaire Vaudois, Rue de Bugnon 46, 1005 Lausanne, Switzerland. E-mail: igor.gossuin@chuv.ch
Introduction: Proximal femur fractures in below-knee amputees pose significant surgical challenges due to difficulties in positioning and stabilizing the residual limb for fracture reduction. In the current literature, there is no consensus on the optimal management strategy, but the inverted boot positioning method seems to be an adequate and non-invasive technique. However, in our case, this method was not possible due to limited knee flexion, so we describe our technique and compare the different modalities described in the literature, highlighting their advantages and disadvantages.
Case Report: A 69-year-old female patient, who underwent a Burgess amputation 10 years ago, fell from her height onto her ipsilateral side and sustained an intertrochanteric fracture of the left femur. We indicated a cephalomedullary nailing procedure. The dilemma is positioning her correctly on the traction table to achieve a satisfactory reduction, especially since knee flexion was limited to 40° and an invasive method was not desired to spare the skin.
Conclusion: Our non-invasive method allowed for traction and control of rotation to achieve a sufficient reduction with no skin damage in cases where the inverted boot setup is not possible. According to the literature, the inverted traction boot method remains as a practical and effective solution, balancing traction and rotational control with minimal invasiveness among the other previously used methods but requires sufficient knee flexion and stump length for proper support. Future research should refine these techniques, develop standardized protocols, and assess comparative outcomes to improve clinical management in this challenging patient group.
Keywords: Below-knee amputation, proximal femoral fracture, traction table, intraoperative positioning.
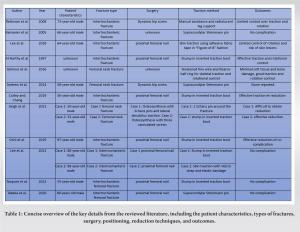
With the aging population, proximal femur fractures, including intertrochanteric fractures, are becoming increasingly common, resulting in significant health-care costs [1]. The prevalence of patients living with an amputated limb is also increasing significantly. According to demographic projections, approximately 3.5 million Americans are expected to be affected by 2030 [2]. Proximal femur fractures in patients with below-knee amputations present significant surgical challenges due to difficulties in achieving stable intraoperative positioning and effective limb manipulation, with factors such as skin condition, stump length, and knee flexion coming into play [3, 4]. The current literature lacks definitive guidance on optimal management techniques, with traditional methods often proving inadequate due to altered anatomy and biomechanical constraints. The inverted boot method, which involves positioning the stump in flexion with the boot placed upside down on the traction table, is the most commonly described non-invasive technique, but none describe an effective non-invasive method when knee flexion does not allow its use. Adhesive and non-adhesive traction methods are described as effective for traction but are less effective for rotational control, making fracture reduction difficult [5, 6].
A 69-year-old female patient, who had undergone a below-knee amputation 10 years prior due to foot necrosis from severe vasculopathy, presented to the emergency department following a fall from standing height, landing on her left side. Radiographic and clinical evaluations revealed a displaced intertrochanteric fracture (Fig. 1 and 2).
Consequently, we recommended closed reduction and osteosynthesis using a cephalomedullary nail. We needed a non-invasive method to avoid damaging the skin, taking into account that the knee had a maximum flexion of 40°, which did not allow for an inverted boot setup. The patient was positioned supine on a traction table with perineal support. Non-adhesive skin traction was applied to achieve adequate traction, and a rectangular metal bar was attached to the stump for rotational control, fixed parallel to the leg. We decided on this method due to the limitations of knee flexion and the need for an effective non-invasive technique. The non-invasive approach was particularly important due to the patient’s lower limb arteriopathy and the associated risks of poor skin healing. The contralateral leg was securely fastened to a leg support, with the limb positioned in abduction to facilitate easy access for the image intensifier (Fig. 3-5).
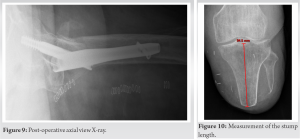
To prevent the risk of slipping, traction was applied gradually while carefully ensuring that the stump remained securely attached. Using standard reduction measures of traction and internal rotation for intertrochanteric fractures, a sufficient reduction was achieved (Fig. 6).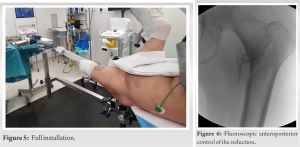
Our method was effective in ensuring adequate traction and rotational control to satisfactorily reduce the fracture and place the implant under optimal conditions. The stump’s length (9.45 cm) provided a sufficient extension for the traction to adhere adequately for reduction and for securing the bar rigidly (Fig. 10).
Tensioned fine wire and ilizarov ring
Gilmour et al. describe a technique using 1.8 mm tensioned fine wire passed through the distal femur, tensioned to an Ilizarov half ring [7]. This method provides skeletal traction and rotational control with minimal soft tissue and bone damage, suitable for patients with very short residual limbs or complex fracture patterns.
Inverted traction boot technique
Initially proposed by Al-Harthy et al., this widely used method involves securing the below-knee stump in an inverted boot to apply traction and rotational control, effectively reducing fractures without invasive pin insertion [8]. Curley and Chang demonstrated its application in a 56-year-old patient with an ipsilateral intertrochanteric fracture, achieving successful reduction and stabilization using a cephalomedullary device [9]. Singh et al. also reported its efficacy in a 23-year-old patient with a femoral neck fracture requiring osteosynthesis [10]. Ochi et al., Lee et al., and et al. (2022) validated its use for achieving an adequate reduction in femoral intertrochanteric fractures without complications [4, 11, 12]. This technique offers effective rotational control and linear traction, making it practical for various fracture types and sufficient stump lengths.
Supracondylar Steinmann pin
As described by Ramseier et al., this method involves inserting a supracondylar Steinmann pin above the knee joint to provide direct femoral traction, facilitating fracture reduction while minimizing complications associated with tibial traction [13]. Berg and Bhatia applied it in a 58-year-old patient with a femoral neck fracture, enabling sufficient traction for osteosynthesis with a dynamic hip screw device [5]. Takeba et al. also found it effective for proximal femoral nail insertion in intertrochanteric fractures in an 80-year-old male without complications [6].
Skin traction
Lee et al. discussed a method of applying skin traction using adhesive fabric tape in a “Figure-of-8” fashion around the stump and traction boot [14]. Lee et al. described another method using Velcro straps and an elastic bandage, providing sufficient traction and rotational control for fracture reduction [11].
Manual assistance and radiolucent leg support
Rethnam et al. described methods involving manual assistance for traction and positioning of the stump on radiolucent leg support for undisplaced femoral intertrochanteric fractures in a 73-year-old patient requiring a dynamic hip screw implant [15]. While less invasive and suitable for minimally displaced fractures, it offers limited traction and rotational control, thus less ideal for complex cases.
Other techniques
Singh et al. employed two Schanz pins around a femoral neck fracture in a 50-year-old patient, manipulating fragments in a “joystick” fashion but found it inefficient for adequate reduction [10]. A comparative analysis of traction techniques reveals distinct advantages and limitations. The tensioned fine wire and Ilizarov ring method provide precise traction with minimal tissue damage, making it ideal for complex fractures, though it requires specialized equipment and expertise. Conversely, the inverted traction boot method is simpler and versatile, suitable for various stump lengths but dependent on the flexion of the knee. The supracondylar Steinmann pin offers effective traction in non-osteoporotic bones but carries risks of pin site infection and osteoporotic bone cutout. In terms of rotational control, the supracondylar Steinmann pin and the inverted boot method excel compared to skin traction and manual methods, crucial for accurate reduction in complex fractures. The tensioned fine wire and Ilizarov ring method also provide precise rotational control but demand significant surgical experience. Regarding invasiveness and risk of complications, skin traction, and manual methods are less invasive, thereby reducing the risk of infection and soft tissue damage, though they may fall short in severe fracture cases. In the literature, the field of proximal femur fractures in below-knee amputees remains relatively underexplored, predominantly documented through case reports that often lack comprehensive details on complications and long-term follow-up. Despite these limitations, there is a consensus favoring the inverted boot method for its simplicity and effectiveness, making it (while possible) the preferred initial approach for most cases and consistently yielding satisfactory outcomes. However, alternative methods such as supracondylar traction or tensioned fine wire with an Ilizarov ring are reserved for more complex scenarios where the inverted boot method proves inadequate or unsuccessful. While the inverted boot method emerges as the predominant approach, correlating a specific method to fracture patterns remains challenging. Singh et al. and Lee et al. illustrated this challenge, demonstrating varied installation techniques benefiting similar cases-two patients with intertrochanteric fractures and two with femoral neck fractures-by the same surgeon [10, 11]. Skin traction systems outlined by Lee et al. in 2018 and 2021 have demonstrated less efficacy in ensuring optimal traction and rotation, particularly with regard to rotational control and stabilization once the fracture is reduced. The Ilizarov fixator technique, described by Gilmour et al. (2016), although represented in only one case report among the 12 analyzed, appears optimal due to its structural design and the ability to use multiple pins, thereby reducing rotational stress, minimizing soft tissue damage, and enhancing precision during mobilization. In contrast, the use of supracondylar Steinman pins carries a notable risk of cutouts in osteoporotic bone but remains an invasive method [7]. Other innovative techniques, such as those detailed by Mitrasinovic et al., achieve optimal reduction without causing soft tissue damage, yet caution is warranted due to the proximity of the Steinmann pin to the neurovascular bundle of the proximal leg [3]. Furthermore, case reports frequently assert the superiority of their respective methods without reporting associated complications [11, 14]. This comprehensive approach underscores the necessity for continuous research and innovation to address the unique challenges presented by proximal femur fractures in below-knee amputees. Such efforts are critical to ensure that treatment strategies evolve to meet the diverse needs of patients and achieve improved clinical outcomes in this challenging domain of orthopedic care. Additional comparative studies with larger datasets, long-term follow-up, and control groups are essential to substantiate the assertion that the inverted boot method is the optimal approach for managing these fractures effectively. We describe our method as effective, and comparable to all other techniques described in the literature.
Positioning a below-knee amputee patient for the reduction of a proximal femur fracture is a challenge. Our method allowed for traction and control of rotation to achieve a sufficient reduction with no skin damage. Future research should concentrate on refining these techniques, investigating hybrid approaches, assessing long-term outcomes, and measuring patient satisfaction. This will enhance current knowledge and facilitate the development of specific protocols to manage these complex cases.
Description of a non-invasive technique for managing proximal femur fractures in below-knee amputees, which employs non-adherent skin traction and a metal bar for effective positioning on a traction table, ensuring optimal traction and rotational control when traditional methods are not applicable.
References
- 1.Adeyemi A, Delhougne G. Incidence and economic burden of intertrochanteric fracture. JBJS Open Access 2019;4:e0045. [Google Scholar]
- 2.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008;89:422-9. [Google Scholar]
- 3.Mitrasinovic S, Kiziridis G, Wellekens S, Roslee C, Anjum SN. Innovative method of traction in a bilateral diaphyseal femur fracture in a polytrauma below-knee amputee. Case Rep Orthop 2019;2019:8691398. [Google Scholar]
- 4.Tanpure S, Chaugule C, Date J, Naikwade D. Intertrochanteric femur fracture fixation in a patient with below-knee amputation presents a surgical dilemma: A case report. J Orthop Case Rep 2022;12:105-8. [Google Scholar]
- 5.Berg AJ, Bhatia C. Neck of femur fracture fixation in a bilateral amputee: An uncommon condition requiring an improvised fracture table positioning technique. BMJ Case Rep 2014;2014:bcr2013203504. [Google Scholar]
- 6.Takeba J, Imai H, Kikuchi S, Matsumoto H, Moriyama N, Nakabayashi Y. Learning point of the article: A simple method for positioning the traction table during fixation surgery for a displaced femoral trochanteric fracture in a patient following ipsilateral above-the-knee amputation: A case report. J Orthop Case Rep 2020;10:76-9. [Google Scholar]
- 7.Gilmour L, Kassam AM, Hughes AM. Tensioned Fine Wire for Proximal Femur Traction Table Reduction in Amputees. Exeter, UK: Royal Devon and Exeter NHS Foundation Trust; 2017. [Google Scholar]
- 8.Al-Harthy A, Abed R, Campbell AC. Manipulation of hip fracture in the below-knee amputee. Injury 1997;28:570. [Google Scholar]
- 9.Curley AJ, Chang ES. Operative positioning technique for an intertrochanteric fracture in a patient with an ipsilateral below-the-knee amputation: A case report. JBJS Case Connect 2019;9:e1. [Google Scholar]
- 10.Singh D, Dhammi IK, Jain A, Shahi P, Kumar S, Bansal K. Osteosynthesis in femoral neck fracture in two patients with ipsilateral lower limb amputation. BMJ Case Rep 2021;14:e239060. [Google Scholar]
- 11.Lee SM, Suh KT, Oh YK, Shin WC. Manipulation of intertrochanteric fractures in patients with below- or above-knee amputation using a fracture table: Two case reports. Medicine (Baltimore) 2021;100:e24233. [Google Scholar]
- 12.Ochi H, Baba T, Hamanaka T, Ozaki Y, Watari T, Homma Y, et al. Safe and effective reduction technique for intertrochanteric fracture with ipsilateral below-knee amputated limb. Case Rep Orthop 2017;2017:2672905. [Google Scholar]
- 13.Ramseier LE, Werner CML, Hug T, Preiss S. Suprakondyläre extension einer pertrochantären femurfraktur bei einem patienten mit unterschenkelamputation. Unfallchirurg [Supracondylar traction of a pertrochanteric femur fracture in a patient amputated below the knee]. Unfallchirurg 2005;108:239-40. [Google Scholar]
- 14.Lee BH, Ho SW, Kau CY. Surgical fixation of a comminuted inter-trochanteric fracture in a patient with bilateral below knee amputation. Malays Orthop J 2018;12:54-6. [Google Scholar]
- 15.Rethnam U, Yesupalan RS, Shoaib A, Ratnam TK. Hip fracture fixation in a patient with below-knee amputation presents a surgical dilemma: A case report. J Med Case Rep 2008;2:296. [Google Scholar]