a) Educating patients on the importance of reporting urinary symptoms preoperatively can help in early detection and prevention of complications. b) Patients should be advised on measures to prevent UTIs, such as adequate hydration and good personal hygiene, especially in the days leading up to surgery.
Dr. V Sandeep Patil, Department of Orthopaedic, Sri Madhusudan Sai Institute of Medical Sciences and Research, Sathya Sai Grama, Muddenahalli, Chikkaballapur, Karnataka, India. E-mail: sandeepvbmc@gmail.com
Introduction: The annual incidence of fractured neck of femur in the elderly continues to rise year after year. Longer lifespan also contributes to the increase in the incidence of fracture neck of femur. Contributing factors include genetic factors, reduced bone mineral density, physical inactivity, aging population, and environmental factors such as diet and vitamin D levels. Urinary tract infections (UTIs) are common in elderly population, especially females with associated risk factors such as diabetes mellitus, obesity, malnutrition, immunosuppression, and malignancies.
Case Report: A series of 10 cases of either gender above 55 years with fractured neck of femur associated with UTI were included in the study. All patients were clinically assessed for UTI supported with laboratory evidence of urine cultures followed by medical management for control of UTI, before surgery. Patient was operated using cemented modular bipolar prosthesis with antibiotic bone cement for femoral stem implantation only after the infection was under control.
Conclusion: Diagnosis and control of UTI are of utmost importance before operating patients with fracture neck of femur with hemiarthroplasty.
Keywords: hemiarthroplasty, pre operative urinary tract infection, cemented bipolar prosthesis, posterior hip approach ,neck femur fracture
The annual incidence of neck of femur fractures in aging population in India has continued to rise year after year. Apart from an increasing urbanization throughout Asia, there has also been an increase in the proportion of the elderly population due to an increase in average life span [1]. With changing world population dynamics, it has been estimated that more than half of these fractures will be concentrated in Asia by the year 2050 and although the exact reason for this geographic distribution is poorly understood, proposed contributing factors include genetic factors, less bone mineral content, physical activity, aging population, and environmental factors such as diet and vitamin D levels. The purpose of study is to identify and treat the urinary tract infection (UTI) in neck of femur fracture cases and manage them using standard protocols in rural Indian population. Osteoporotic hip fractures have become a major cause of morbidity and mortality in the adult and elderly population around the world. Hip fractures are becoming a matter of concern in Asia particularly because of a 2–3 times increase in their incidence in almost every country in the continent [1, 2]. The incidence of hip fracture is estimated to rise from 1.66 million in 1990 to 6.26 million in 2050 [3]. Apart from an increasing urbanization throughout Asia, there has also been an increase in the proportion of the elderly population due to an increase in average life span [1, 4]. To the best of our knowledge, the influence of these factors on hip fractures and their significance in Indian population has not been studied extensively till to date. The understanding of these risk factors and their significance will help policymakers and healthcare providers to develop strategies and prioritize them to reduce the rising trend of hip fractures in rural India. Hip fractures comprise about 20% of the operative workload of an orthopedic trauma unit. As a consequence, proximal femur fractures are a significant cause of morbidity and mortality in all age groups, especially in elderly. Many authors have explained many theories [5, 6] and risk factors [7] regarding the pathogenesis of infection after joint arthroplasty to prevent and control this condition. UTI is defined in accordance to 2004 Centre for Disease Control, as an infection that meets at least one of the following criteria [8].
- At least one sign and symptom – fever >38°C, urinary urgency, dysuria, or suprapubic tenderness with no other recognizable cause.
Positive urine culture with 105/cm3 or more microorganisms of urine with no more than two species of microorganisms.
- At least 2 signs and symptoms – fever >38°C, urgency, frequency, dysuria, or suprapubic tenderness with no other recognized cause and at least one of the following: positive leukocyte esterase or nitrite, pyuria (urine specimen with 10 leukocytes/mm3 or more, organisms on Gram stain of unspun urine, two positive urine cultures with the same uro-pathogen with 102 colonies/mL or more in non-voided specimens, 105 colonies/mL or less of one uro-pathogen in a patient being treated for a UTI.
After obtaining ethical clearance from the Institutional ethical committee, this prospective study was conducted in the Department of Orthopaedics in Sri Madhusudhan Sai Institute of Medical Sciences and Research from July 2022 to December 2023.We have done a study in 10 patients above 55-year age group in both genders with neck of femur fracture with UTI before surgery. Fracture diagnosis confirmed by clinical examination and radiography. Diagnosis of urinary tract infection done clinically and laboratory values – urine routine examination and urine cultures taken pre-operatively. Medical management is done for urinary tract infection until infection is controlled, proven clinically, and with laboratory values – urine routine and cultures. We have obtained informed and written consent before surgery. After control of infection, patients underwent modular bipolar hemiarthroplasty. We considered the source of UTI to be the most likely bacterial common UTI and joint infection was considered dichotomous variables (presence versus absence). Urine cultures were done which were positive as seen in Table 1.
This study was undertaken to assess the efficacy of medical management of UTI before cemented modular bipolar hemiarthroplasty and post-operative follow-up and complications.
Age
Analyzing the results as per age revealed that 5 patients (50%) were in the age group of 55–65 years. 2 patients (20%) were in the age group 65–75 years and 3 patients (30%) were in the age group 75–85 years. The observations made in the study are comparable to study by Chincholi and Prasad [4] where all the subjects are above the age group more than 55 years.
Gender
In our study, 80% were female and 2 patients (20%) were male, comparable to the study by Chincholi and Prasad [4] where 60% of study population is female and 40% are male.
Mode of injury
All the patients 10 (100%) had a history of self-fall at their residences which was a fall from standing height resulting in fracture neck of femur, suggesting a simple low-velocity injury causing the fracture indicating osteoporotic fracture.
Fracture classification (Garden’s classification of neck of femur fractures [9])
2 patients (20%) had Garden’s type 2 fracture, 3 patients (30%) had Garden’s type 3 fracture, and 5 patients (50%) had Garden’s type 4 fracture.
Pre-operative organism
Urine cultures in 6 patients (60%) yielded Escherichia coli, 2 patients (20%) yielded Klebsiella species, 1 patient (10%) yielded Staphylococcus aureus, and 1 patient (10%) yielded Pseudomonas species (Tables 1 and 2). Findings of our study are similar to findings of Lin et al. [10] where UTI is more common in females and the most common organism is E. coli.

Risk factors for UTI
6 patients out of 10 had type 2 diabetes mellitus (60%) and were on regular medications. Findings of our study are similar to findings of Abdulla et al. [11] where female gender, age, and duration of diabetes were found to be risk factors for developing UTI. E. coli was the most common organism causing UTI in diabetes
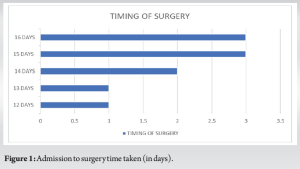
Timing of surgery
1 patient (10%) was operated 12 days after admission, 1 patient (10%) was operated 13 days after admission, 2 patients (20%) were operated after 14 days, 3 patients (30%) were operated after 15 days, and 3 patients (30%) were operated after 16 days of admission (Fig. 1).
The findings of Horner et al. [12] were similar to our study where timing from admission to surgery did not affect the incidence of post-operative infection. The delay in surgery to more than 10 days is attributed to medical management of UTI, obtaining negative urine cultures before surgery and subsidence of signs and symptoms of UTI was utmost important before surgery. All our patients were operated using posterolateral Moore’s (southern) approach. Pre-operative radiographs and post-operative radiographs are shown in Figs. 2-4.


Intra-operative images (Images 1-3)

Pre-operative radiograph of patient with neck femur fracture
None of the patients had any surgical site infection (SSI), prosthetic joint infection, or any wound-related complications during a follow-up period of 6 months after surgery. This indicates medical management before surgery, aseptic intraoperative protocols, and use of antibiotic bone cement resulted in no post-operative complications.
Follow-up and Harris hip score [13]
Post-operative radiographs – anterior posterior view
Post-operative radiographs – lateral view
Post-operative complications
Fig. 5 shows 20% of study population, and 2 patients had a Harris Hip Score between 70 and 79 (which is a fair functional outcome). 50% of study population, 5 patients had a Harris Hip Score between 80 and 89 (which is a good functional outcome). 30% of study population, 3 patients had a Harris Hip Score of 90–100 (which is an excellent functional outcome).
Signs and symptoms of UTI if seen in patients with fracture neck of femur in old age should be diagnosed at an early stage and treated till infection is controlled. Patients are to be operated after laboratory-proven negative urine cultures are obtained. Antibiotic cement was used for femoral stem fixation and intravenous antibiotics continued for 2 weeks post-operatively. No SSIs were noted in the patients in 6-month follow-up. Implementation of standard protocols and improved hygiene with antibiotics postoperatively yields better results.
Management of fracture neck of femur in the elderly with associated risk factors and UTIs is challenging. Control of infection and asepsis during surgery and post-operative antibiotic administration play a key role to achieve successful outcome.
References
- 1.Patel MC, Chandra M, Lo JC. Mortality following hip fracture in Chinese, Japanese, and Filipina women. Am J Manag Care 2016;22:e358-9. [Google Scholar]
- 2.Lau EM. The epidemiology of osteoporosis in Asia. IBMS Bonekey 2009;6:190-3. [Google Scholar]
- 3.Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos Int 1992;2:285-9. [Google Scholar]
- 4.Chincholi S, Prasad KV. Occurrence of fracture neck femur in the elderly Indian population. Int J Orthop Sci 2017;3:706-9. [Google Scholar]
- 5.Burke JP. Infection control-a problem for patient safety. N Engl J Med 2003;348:651-6. [Google Scholar]
- 6.Douglas P, Asimus M, Swan J, Spigelman A. Prevention of orthopaedic wound infections: A quality improvement project. J Qual Clin Pract 2001;21:149-53. [Google Scholar]
- 7.Koulouvaris P, Sculco P, Finerty E, Sculco T, Sharrock NE. Relationship between perioperative urinary tract infection and deep infection after joint arthroplasty. Clin Orthop Relat Res 2009;467:1859-67. [Google Scholar]
- 8.Chenoweth CE. Urinary tract infections: 2021 update. Infect Dis Clin North Am 2021;35:857-70. [Google Scholar]
- 9.Kazley JM, Banerjee S, Abousayed MM, Rosenbaum AJ. Classifications in brief: Garden classification of femoral neck fractures. Clin Orthop Relat Res 2018;476:441-5. [Google Scholar]
- 10.Lin YC, Hsu YC, Wu WT, Lee RP, Wang JH, Chen HW, et al. The incidence of severe urinary tract infection increases after hip fracture in the elderly: A nationwide cohort study. Sci Rep 2021;11:3374. [Google Scholar]
- 11.Abdulla MC, Jenner F, Alungal J. Urinary tract infection in type 2 diabetic patients: Risk factors and antimicrobial pattern. Int J Res Med Sci 2015;3:2576-9. [Google Scholar]
- 12.Horner NS, Grønhaug Larsen KM, Svantesson E, Samuelsson K, Ayeni OR, Gjertsen JE, et al. Timing of hip hemiarthroplasty and the influence on prosthetic joint infection. PLoS One 2020;15:e0229947. [Google Scholar]
- 13.Hussain SU. The outcome of hemiarthroplasty for neck of femur fractures in terms of Harris hip score. 2009. [Google Scholar]