This is a case of a giant cell tumor involving the proximal tibia, which was found to be aggressive, so a resection and arthrodesis was done using a limb reconstruction system.
Dr. Karthik Loganathan, Department Of Orthopaedics, Government Stanley Medical College, Chennai, Tamil Nadu, India. E-mail: karindu1989@gmail.com
Introduction: Giant cell tumors (GCTs) are one of the most aggressive benign tumors of the bone. For tumors around the knee joint, excision with preservation of joint movement is preferred. Resection arthrodesis or an amputation might be necessary sometimes.
Case Report: In this case study, we report a 23-year-old female who had an aggressive osteolytic lesion of the proximal tibia with articular breach. The biopsy revealed an aggressive GCT.
Conclusion: Then the patient was managed with resection arthrodesis with fibular strut graft, limb reconstruction system, and augmentation plating. The limb reconstruction system was removed after the union was achieved.
Keywords: Giant cell tumors, resection, arthrodesis, limb reconstruction system.
Giant cell tumors (GCTs) are one of the most aggressive non-malignant tumors of the bone. Long bones around the knee joint are the most affected ones [1]. 20–45 years is the most commonly affected age group. An aggressive, potentially malignant tumor is the classification of GCTs given by the World Health Organization. Its histogenesis is unpredictable. In cortex-breached tumors and huge soft-tissue-involved tumors, extended curettage has not produced as fair results as in the case of tumors confined to the bone. Hence, for more aggressive tumors with soft-tissue extension wide resection is the treatment of choice. After resection of the mass, the perfect method of reconstruction is still under argument [1]. High cost, adequate motor reconstruction, and repeated surgeries are the drawbacks of endoprosthetic replacement. Many centers are utilizing massive allografts. However, time and money are the consequences, and for various reasons, it is not obtainable in numerous parts of the world. A stable limb can be achieved by an arthrodesis which might seem less attractive initially but the patient might not need a revision surgery. Some procedures such as intercalary auto graft utilize double fibular graft to link the void after removal of the tumor. Ilizarov technique can also be utilized to achieve arthrodesis. In this study, we report a case of violent osteoclastoma of the proximal tibia, managed with resection and arthrodesis of the knee.
A 23-year-old female who had 4 months of amenorrhea came to the hospital with complaints of swelling after a trivial trauma to the right knee after which she continued to weight bear until her delivery. After 15 days of her delivery, she came to the outpatient department with severe pain and swelling of the right knee.
Clinical findings
On physical examination 10 × 8 cm bony hard swelling was present in the proximal tibia anterolateral aspect. The patient had no neurological deficit. The patient did not have any comorbidities. A plain radiograph showed an expansile lytic lesion in the meta-diaphyseal region of the proximal tibia.
Diagnostic assessment
The patient received investigations such as plain X-ray, computed tomography, and magnetic resonance imaging. The involvement of the neurovascular bundle was assessed. Deciding the extent of soft-tissue involvement, its relationship with the vein, artery, nerves, articular cartilage violation, the intramedullary stretch of the tumor, and working out an accurate resection length was the main aim of the study. In the case of tumors with cortical extension, the Campanacci staging system is used [2, 3]. Based on this our case was pertaining to stage III. Preoperatively, the Enneking stage was also assessed [2, 3]. As per this system, our case was found to be in stage III. In our case, an open biopsy was done, and the patient underwent surgery after evaluation of histopathology (Fig. 1).
Therapeutic intervention
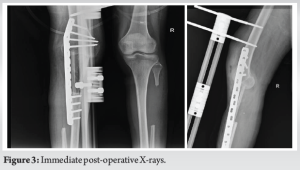
Through an anterolateral incision, the tumor was exposed and the amount of bone to be resected free from tumor margins was marked. Soft tissues were also cleared at the site of resection. All muscles invaded along with the tumor were excised. The resulting defect was around 8 cm. The void was filled with double fibular autografts. The graft length was around 10–12 cm calculated according to the size of the void. Fixation was done using a pre-contoured locking broad dynamic compression plate and supported with a limb reconstruction system (Fig. 2).
Follow-up and outcomes
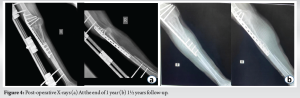
The patient was followed up once in 7 days for the initial month to identify problems such as wound infection and then monthly follow-up for the 1st year. X-rays were used for confirmation of the union of grafts at sites of osteotomy including bony borders in the middle of the dual fibular graft and the native bone [4-10]. The patient was instructed to come for follow-up once in 6 months for the rest of the interval. Touch down weight-bearing was permitted after the quickest sign of union then advised full activity after complete union of the graft which in our case was at the end of 8 months. After 18 months the limb reconstruction system was removed and allowed weight bearing freely without support (Fig. 3 and 4).
The patient was healthy and did not have any signs of local or systemic recurrence. Musculoskeletal Tumor Society’s modified system was used to functionally evaluate the outcome. The score range was around 26 out of a total 30. A systematic method was utilized for the evaluation of the radiological union of the replanted segment at both ends [5]. Complications such as graft resorption, failure of the implant, and neurovascular deficit were not experienced.
GCT is an incalculable tumor. Several authors have not been able to discover the biological or histological parameters to come to a conclusion on treatment protocol and prognostic factors [4]. Surgery is the primary treatment option for this locally aggressive tumor. Tumor recurrence can be reduced by adequate tumor resection. The main surgical goals are to remove the tumor adequately and also leave the residual native bone. Wide resection is necessary in tumors with extension beyond the cortex and invasion of soft tissue [9]. Numerous approaches are available to reconstruct the void resulting after tumor resection. There is no single successful method for managing large bony defects. Usually, when asked, both orthopedicians and patients prefer procedures that permit movement at the knee joint. However, a mobile knee requires good knee extension. Hence, arthrodesis is done for cases where the quadriceps is also resected with a tumor [6]. The use of double fibular strut graft comes into role in such situations. In a study with 52 cases, where the void was around 9–24 cm Kirschner wires were used within the grafts to supplement and to avoid stress fractures [7, 10]. Reconstruction using the callus distraction method in distal femur tumors was explained in a study by Kapukaya et al. [8].
Aggressive GCT of the proximal tibia with extensive soft-tissue involvement needs wide resection. To obtain a proper safety margin, removal of all the involved compartments is necessary, making reconstruction of the prosthesis quite difficult, thus making arthrodesis as the only viable option. Using fibular grafts, plating, and a limb reconstruction system, arthrodesis can be achieved with good to excellent results. Thus, an immobile knee in an anatomical and functional position to attain a stable and painless limb can be considered appropriate management of choice.
Giant cell tumors are non-malignant but local aggressive lesions that may affect the joint in some instances. In such cases, a wide resection and arthrodesis could be the best option to consider, especially when the lower limb is involved.
References
- 1.Dahlin DC, Cupps RE, Johnson EW Jr. Giant-cell tumor: A study of 195 cases. Cancer 1970;25:1061-70. [Google Scholar]
- 2.Campanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. J Bone Joint Surg Am 1987;69:106-14. [Google Scholar]
- 3.Szendroi M. Giant-cell tumour of bone. J Bone Joint Surg Br 2004;86:5-12. [Google Scholar]
- 4.Turcotte RE. Giant cell tumor of bone. Orthop Clin North Am 2006;37:35-51. [Google Scholar]
- 5.Hsu RW, Wood MB, Sim FH, Chao EY. Free vascularised fibular grafting for reconstruction after tumour resection. J Bone Joint Surg Br 1997;79:36-42. [Google Scholar]
- 6.Kapoor SK, Tiwari A. Resection arthrodesis for giant cell tumors around the knee. Indian J Orthop 2007;41:124-8. [Google Scholar]
- 7.Yadav SS. Dual-fibular grafting for massive bone gaps in the lower extremity. J Bone Joint Surg Am 1990;72:486-94. [Google Scholar]
- 8.Kapukaya A, Subaşi M, Kandiya E, Ozateş M, Yilmaz F. Limb reconstruction with the callus distraction method after bone tumor resection. Arch Orthop Trauma Surg 2000;120:215-8. [Google Scholar]
- 9.Wolf RE, Scarborough MT, Enneking WF. Long-term follow up of patients with autogenous resection arthrodesis of the knee. Clin Orthop Relat Res 1999;358:36-40. [Google Scholar]
- 10.Muscolo DL, Ayerza MA, Aponte-Tinao LA, Ranalletta M. Use of distal femoral osteoarticular allografts in limb salvage surgery. J Bone Joint Surg Am 2005;87:2449-55. [Google Scholar]