Percutaneous hamstring lengthening is as effective as open hamstring lengthening in improving knee function in children with spastic diplegic cerebral palsy, with potential advantages in muscle preservation and mobilization.
Dr. Syed Faisal Afaque, Department of Paediatric Orthopaedics, King George Medical University, Lucknow, Uttar Pradesh, India. E-mail: syedfaisalafaque@gmail.com
Introduction: Cerebral palsy (CP) often manifests with crouch gait due to hamstring spasticity, necessitating surgical intervention like hamstring lengthening surgery. Percutaneous techniques are emerging as an alternative to traditional open approaches in orthopedic surgeries.
Objectives: This randomized controlled trial aimed to compare the outcomes of percutaneous hamstring lengthening (pHSL) versus open hamstring lengthening (oHSL) in pediatric patients with spastic diplegic CP, focusing on improvements in gait and knee function.
Materials and Methods: One hundred children diagnosed with spastic diplegic CP were randomized into pHSL (n = 50) and oHSL (n = 50) groups. Surgical procedures were performed using single-event multilevel surgery techniques. Pre-operative and post-operative assessments included range of motion, popliteal angle, gross motor function classification system (GMFCS) score, and gait analysis (functional independence measure [FIM], observational gait scale [OGS], physician gait scale). Statistical analyses were conducted using Statistical Packages for the Social Sciences v25.
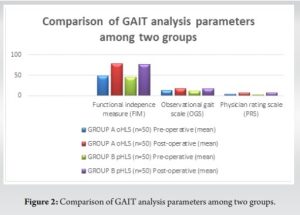
Results: Both pHSL and oHSL groups showed significant improvements in popliteal angle and GMFCS scores postoperatively (P < 0.001 within each group). However, there were no significant differences between the groups in terms of these outcomes (P > 0.05). FIM, OGS, and physician gait scale also showed comparable improvements between groups (P > 0.05).
Conclusion: pHSL is as effective as oHSL in improving gait and knee function in pediatric patients with spastic diplegic CP. The percutaneous approach offers a safe and efficient alternative to traditional open surgery, potentially minimizing muscle damage and promoting quicker recovery.
Keywords: Cerebral palsy, hamstring lengthening surgery, percutaneous surgery, gait analysis, pediatric orthopedics.
Cerebral palsy (CP) is a non-progressive condition impacting movement and posture, stemming from early brain development injury [1]. It represents the most prevalent cause of enduring motor impairment; with an estimated prevalence of 3.3/1000 live births in the US [2]. Individuals with CP commonly experience crouch gait, attributed to hamstrings’ spasticity, contractures, and diminished hip and knee extensor strength [3, 4]. Surgical hamstring lengthening is frequently conducted to address crouch gait. Previous research indicates that hamstring lengthening surgery (HLS) can enhance knee extension along with static and dynamic range of motion (ROM) [5, 6]. Specifically, studies involving children with CP have demonstrated advancements in knee extension during initial contact and throughout the stance phase of the gait cycle post-HLS [7, 8]. HLS encompasses diverse types, including medial and/or lateral hamstring lengthening, with some patients necessitating supplementary procedures such as rectus femoris transfers, iliopsoas lengthening, and bony surgeries [9]. In contemporary orthopedics, percutaneous surgical methods have increasingly emerged as a viable alternative to traditional open approaches. Studies have indicated that percutaneous HLS (pHLS) offer advantages in terms of maximizing muscle strength preservation and facilitating rapid mobilization compared to open techniques [10-12]. Although open HLS (oHLS) has been extensively explored, the available literature on the efficacy of pHLS in CP patients remains limited. A study by Gordon et al. reported improvements in long-term dynamic gait parameters in children with CP following percutaneous medial HLS; however, a comparable group that underwent open lengthening was not included for the assessment [8]. The effectiveness of pHLS compared to oHLS in improving crouch gait and knee function is uncertain. Therefore, our study was designed to assess the influence of open versus percutaneous hamstring lengthening (pHSL) on knee movements in pediatric patients with CP. Specifically, our study involved a comparison of alterations in the popliteal angle, gross motor function classification system (GMFCS) grade [13], functional independence measure (FIM) [14], observational gait scale (OGS) [15], and physician rating scale (PRS) [16].
This study was a randomized controlled trial conducted at a tertiary center and approved by the institutional research ethics board. Gait analysis and clinical data were collected for 100 children with spastic diplegic CP exhibiting crouch, jumping, or scissor gait (flexed knee gait). These patients underwent surgical hamstring lengthening using the single-event multilevel surgery technique, which was performed by a single surgeon. All patients had spastic diplegia affecting both lower limbs to a similar extent. The study encompasses patients aged up to 18 years diagnosed with spastic diplegic CP, demonstrating dynamic contractures resulting in crouch/jump gait, and presenting with moderate or severe spasticity (Ashworth Scale scores 3 and 4), subject to their provision of consent. However, exclusion criteria encompass patients with static/bony contractures, other forms of CP, a history of prior fracture/dislocation, or contractures developed due to secondary causes such as burns. All patients diagnosed with spastic diplegic CP who presented at the outpatient department and met the predefined inclusion criteria were enrolled in the study. The patients were randomly divided into two groups using the Excel random number technique. Group A underwent pHLS, whereas Group B underwent oHLS. In both groups, treatment commenced with medial hamstring release, involving the semitendinosus and gracilis muscles, with or without semimembranosus release. For Group A, all procedures were conducted with the patient in the supine position. The tendinous portion of the semitendinosus was percutaneously tenotomized along with the gracilis. If the knee extension did not reach at least 20°, partial tenotomy of the semimembranosus was performed. Conversely, patients in Group B underwent procedures in the prone position. The midline posterior approach was utilized, and classic Z-lengthening of the hamstrings was performed. Bilateral above-knee casts, with the knee in full extension, were applied and maintained for a duration of 6 weeks. Patients were permitted to bear weight as tolerated immediately after the removal of the cast. Preoperatively and postoperatively at 1-year follow-up, all patients underwent an evaluation to assess ROM, popliteal angle, GMFCS score, and gait analysis using FIM, OGS, and PRS. Statistical analyses were conducted utilizing Statistical Packages for the Social Sciences v25 (IBM Corp, Armonk, NY, USA). Outcome variables were compared both within and between groups, using paired t-tests. The Chi-square test was utilized to examine the relationship between continuous and categorical variables. Notably, a P < 0.05 denoted statistical significance.
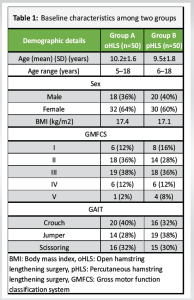
The mean ages of the participants at the time of surgery were 10.2±1.6 years (range: 5-18 years) and 9.5±1.8 years (range: 6-18 years) for the open and percutaneous groups, respectively. Both groups exhibited a female predominance, with 64% in group I and 60% in group II. Other characteristics, including BMI, GMFCS score, and type of gait, demonstrated similarities between the two groups preoperatively (refer to Table 1).
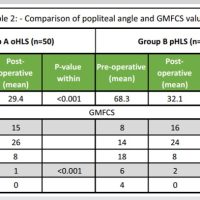
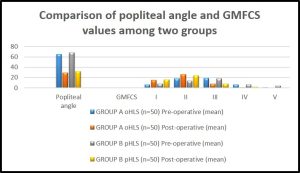
A significant difference was noted within each group (P value <0.001) in terms of popliteal angle improvement. However, such significance was not observed when comparing between groups (P value: 0.84). The GMFCS score within each group showed significant improvement (P < 0.001). Nevertheless, such significance was not observed when comparing between groups (P value: 0.86) (refer to Table 2 and Fig. 1).
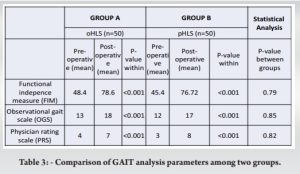
Functional Independence Measure (FIM), Observational Gait Scale (OGS), and Physician Rating Scale (PrS) also revealed no significant differences between the two groups (refer to Table 3 and Fig. 2).
HLS is a crucial operative intervention for addressing spastic CP. This procedure can significantly enhance the gait, posture, and functional abilities of ambulatory children with spastic CP [17]. Moreover, it has demonstrated effectiveness in improving posture and activities of daily living for non-ambulatory CP patients. It is noteworthy that the percutaneous technique, when meticulously executed in the tendinous segment of the muscles by a proficient surgeon, has been proven to be safe and efficacious [17]. In our study, it was observed that the correction of the popliteal angle in the pHLS subgroup corresponded with that of the oHLS subgroup. In addition, comparable changes in GMFCS and GAIT analysis parameters were identified in both subgroups. Khaje Mozafari et al. conducted a study involving 54 patients and concluded that pHSL is a safe, efficient, and expeditious procedure that yields outcomes comparable to those of the open technique for pediatric spastic diplegia. This aligns with the results obtained in our own study [17]. Another study by Nazareth et al. reviewed 87 patients with CP who underwent open or percutaneous HSL procedures, finding no significant disparity between the groups in terms of ultimate popliteal angle and knee kinematics, which is consistent with our findings [18]. Mansour et al. conducted a prospective randomized controlled trial comparing open versus pHSL. The study, which encompassed 18 patients, yielded the finding that both open and pHSL produced significant enhancements in popliteal angle in children with CP. Nevertheless, the percutaneous technique led to unacceptable muscle damage and lesser improvement in knee extension [19]. In contrast, our study reveals similar outcomes across both techniques. Our study holds a unique position in the current literature, as only one prospective comparative study has been published thus far, and it was based on a very small sample size. Therefore, our study has the potential to lay the groundwork for further research in this area. It is important to note that our study is limited by its single-center nature and a relatively brief follow-up period.
The study findings indicate that pHSL represents a safe, straightforward, and efficient procedure for children with spastic diplegic CP. The procedure’s effectiveness mirrors that of the open technique, demonstrating its viability as an alternative approach in this population.
CP leads to persistent motor impairments like crouch gait, often necessitating HLS. This study compared percutaneous (pHLS) versus oHLS techniques in 100 children with spastic diplegic CP. Both methods significantly improved popliteal angle and GMFCS scores within groups, with no significant difference between pHLS and oHLS outcomes. Functional measures (FIM, OGS, PRS) also showed comparable results. The findings support pHLS as a safe and effective alternative to oHLS, providing clinicians with a viable option for managing CP-related gait abnormalities. Further research is warranted to validate these results across diverse clinical settings and long-term follow-up periods.
References
- 1.Sadowska M, Sarecka-Hujar B, Kopyta I. Cerebral palsy: Current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat 2020;16:1505-18. [Google Scholar]
- 2.Arneson CL, Durkin MS, Benedict RE, Kirby RS, Yeargin-Allsopp M, Van Naarden Braun K, et al. Prevalence of cerebral palsy: Autism and developmental disabilities monitoring network, three sites, United States, 2004. Disabil Health J 2009;2:45-8. [Google Scholar]
- 3.Wren TA, Rethlefsen S, Kay RM. Prevalence of specific gait abnormalities in children with cerebral palsy: Influence of cerebral palsy subtype, age, and previous surgery. J Pediatr Orthop 2005;25:79-83. [Google Scholar]
- 4.Bell KJ, Ounpuu S, DeLuca PA, Romness MJ. Natural progression of gait in children with cerebral palsy. J Pediatr Orthop 2002;22:677-82. [Google Scholar]
- 5.Baumann JU, Ruetsch H, Schürmann K. Distal hamstring lengthening in cerebral palsy. An evaluation by gait analysis. Int Orthop 1980;3:305-9. [Google Scholar]
- 6.Adolfsen SE, Ounpuu S, Bell KJ, DeLuca PA. Kinematic and kinetic outcomes after identical multilevel soft tissue surgery in children with cerebral palsy. J Pediatr Orthop 2007;27:658-67. [Google Scholar]
- 7.Kay RM, Rethlefsen SA, Skaggs D, Leet A. Outcome of medial versus combined medial and lateral hamstring lengthening surgery in cerebral palsy. J Pediatr Orthop 2002;22:169-72. [Google Scholar]
- 8.Gordon AB, Baird GO, McMulkin ML, Caskey PM, Ferguson RL. Gait analysis outcomes of percutaneous medial hamstring tenotomies in children with cerebral palsy. J Pediatr Orthop 2008;28:324-9. [Google Scholar]
- 9.Van der Linden ML, Aitchison AM, Hazlewood ME, Hillman SJ, Robb JE. Effects of surgical lengthening of the hamstrings without a concomitant distal rectus femoris transfer in ambulant patients with cerebral palsy. J Pediatr Orthop 2003;23:308-13. [Google Scholar]
- 10.Hachache B, Eid T, Ghosn E, Sebaaly A, Kharrat K, Ghanem I. Is percutaneous proximal gracilis tenotomy as effective and safe as the open procedure? J Child Orthop 2015;9:477-81. [Google Scholar]
- 11.Salamon ML, Pinney SJ, Van Bergeyk A, Hazelwood S. Surgical anatomy and accuracy of percutaneous achilles tendon lengthening. Foot Ankle Int 2006;27:411-3. [Google Scholar]
- 12.Thompson N, Stebbins J, Seniorou M, Wainwright AM, Newham DJ, Theologis TN. The use of minimally invasive techniques in multi-level surgery for children with cerebral palsy. J Bone Joint Surg Br 2010;92-B:1442-8. [Google Scholar]
- 13.Von Elling-Tammen L, Stark C, Wloka KR, Alberg E, Schoenau E, Duran I. Predicting gross motor function in children and adolescents with cerebral palsy applying artificial intelligence using data on assistive devices. J Clin Med 2023;12:2228. [Google Scholar]
- 14.Functional Independence Measure - an Overview. ScienceDirect Topics. Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/functional-independence-measure [Last accessed on 2024 Jul 03]. [Google Scholar]
- 15.Rathinam C, Bateman A, Peirson J, Skinner J. Observational gait assessment tools in paediatrics - a systematic review. Gait Posture 2014;40:279-85. [Google Scholar]
- 16.Maathuis KG, van der Schans CP, van Iperen A, Rietman HS, Geertzen JH. Gait in children with cerebral palsy: Observer reliability of physician rating scale and Edinburgh visual gait analysis interval testing scale. J Pediatr Orthop 2005;25:268-72. [Google Scholar]
- 17.Khaje Mozafari J, Pisoudeh K, Gharanizade K, Abolghasemian M. Percutaneous versus open hamstring lengthening in spastic Diplegic cerebral palsy. Arch Bone Jt Surg 2019;7:373-8. [Google Scholar]
- 18.Nazareth A, Rethlefsen S, Sousa TC, Mueske NM, Wren TA, Kay RM. Percutaneous hamstring lengthening surgery is as effective as open lengthening in children with cerebral palsy. J Pediatr Orthop 2019;39:366-71. [Google Scholar]
- 19.Mansour T, Derienne J, Daher M, Sarraf D, Zoghbi Y, Ghanem I. Is percutaneous medial hamstring myofascial lengthening as anatomically effective and safe as the open procedure? J Child Orthop 2017;11:15-9. [Google Scholar]