Double plating with locking fixation and spanning of the entire scapular spine and acromion when fixing fractures and non-unions related to reverse shoulder arthroplasty are essential to achieve durable results.
Dr. Stefan Bauer, Department of Orthopaedics, Shoulder and Elbow Surgeon, Hôpital de Morges, EHC, 1110 Morges, Switzerland. E-mail: stef11bau@yahoo.co.uk
Introduction: This article presents a simultaneous operative technique, which allowed to successfully treat a Cuff Tear Arthropathy (CTA), instability and Levy-type III scapular spine fracture non-union with 90°-double plating, humerus-to-scapula grafting and simultaneous reverse shoulder arthroplasty.
Case Report: We present a 64year-old woman with previously known cuff arthropathy (2012/53yo). She fell in 2017 (58 years old with minor shoulder disability) before dislocating the shoulder in 2020 (60 years old) with evidence of a medial Levy-type III scapular spine fracture non-union and severe apprehension, unable to anterior elevate her arm more than 90°. She underwent ORIF of a flexed scapular spine with locked 90°-double plating and bone grafting as well as simultaneous lateralized reverse shoulder arthroplasty (RSA) with an excellent outcome at 3.5 years of follow-up (Constant score of 84 points and a subjective shoulder value of 99%).
Conclusion: The radiographic sequence suggests an abduction fracture mechanism due to an axial force. RSA with simultaneous locked 90°-double plating with grafting from the humeral head achieved correction and union with an outstanding result despite tensioning the deltoid with a lateralized RSA. To deal with excessive forces, five important practical recommendations are essential: (1) assess the bone stock with a CT-scan, (2) span the scapular spine and acromion with a long superior plate and its screws, (3) use at least two locking screws on either side of the fracture on each plate, (4) avoid stress risers from erroneous drilling, and (5) protection with an abduction sling for 6–8 weeks.
Keywords: Scapular Spine fracture, fracture Non-union, open reduction and internal fixation, 90°-double plating, reverse shoulder arthroplasty.
Scapula fractures make up 1% of all fractures, and only 10% of all scapula fractures involve the scapular spine (SS) and/or acromion [1]. The acromion and scapular spine origin of the deltoid muscle often apply flexion forces leading to a downward tilt of the distal acromion fragment exposing the patient to sub-acromial impingement. Open reduction and internal fixation (ORIF) in Levy type II-III fractures should thus be considered [2, 3]. Non-union is a complex orthopedic problem and may be defined as the absence of bone-healing after a period of nine months without any sign of bone-healing for a period of at least three months [4]. Biological and mechanical aspects impact bone healing [5] and the presence of adequate blood supply and tissue oxygenation as well as mechanical stability of the fracture site are essential for healing [6]. In 1995, Bauer et al. recommended ORIF (open reduction and internal fixation) for displaced fractures of the SS and the acromion to allow for reduction, fixation, and stability of the fracture site [7]. Acromial and SS fractures also occur as a complication of reverse shoulder arthroplasty (RSA) with an estimated occurrence varying from 2.2% to 4.4% [8-11]. Whether fractures should be reduced and internally fixed or treated nonoperatively is currently still controversial [11]. At present, it has been reported in the literature that the non-operative approach should rather be chosen, which has been documented to lead to similar reduced functional outcomes as the operative approach [12,13] when compared with the results of RSA without this complication. However, the operative techniques used in the past were inhomogeneous including single plates, non-locking plates, screws, tension band wiring, and bone strut plates. As we witnessed an excellent outcome and bony union in the treatment of an acute SS fracture after RSA with locked 90° double plating of the scapular spine [14], we aimed to apply the same technique for this case of a hypertrophic non-union with additional humerus-to-scapula bone grafting, and a simultaneous RSA for the cuff tear arthropathy and shoulder.
We present a 60-year-old female who suffered from a cuff tear arthropathy, documented at first on radiographs in 2012 after a fall (Fig. 1).
She dislocated her right shoulder after a fall in 2020, which she reduced herself. Two more episodes of shoulder luxation occurred, the last requiring reduction under sedation in the emergency department. Her fear about to dislocate again prompted her to seek consultation with a shoulder surgeon. During the clinical examination, she presented with apprehension, slight pain – which occurred only during movement (2/15 VAS), as well as reduced range of motion (ROM) (Table 1). The radiographs and CT-scan confirmed the diagnosis of hypertrophic scapular spine non-union and rotator cuff arthropathy of the right shoulder (Fig. 2). The patient had attended the emergency department twice before, once in 2012 at age 53 and again in 2016 at age 57, each time due to falls. No fractures were detected on radiographs. She was treated with simple analgesia, and her shoulder was mobilized as tolerated. She had not received any other treatment for her shoulder.
Indication and treatment
Recurrent dislocations associated with a flexed scapular spine non-union and a radiographically severe CTA required simultaneous correction of the flexed acromion with ORIF and RSA. A two-staged approach, with primary ORIF and grafting before RSA as most recently reported [15], was not considered, as it would not have adequately addressed the instability and would have required an additional site for autologous grafting, such as the iliac crest. The patient was positioned in beach chair position (80°) with an adjustable arm holder in abduction (Fig. 3).
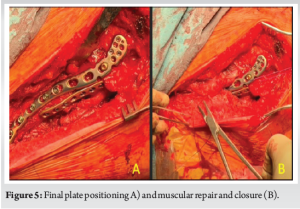
A double approach was used: First a direct posterior approach to the scapular spine, revealing a hypertrophic L-shaped non-union with posterolateral flexion of the acromion. It was debrided and freshened up with an awl and small 2.0 drill bit. The ORIF was planned with a long superolateral titanium clavicle plate (Depuy Synthes) contoured for optimal fit. A second posterior 2.4-mm LCP (Depuy Synthes compact foot set) was used (Fig. 4). The RSA was performed with a deltopectoral approach. In situ, the humeral head osteotomy (20° retroversion) was incompletely performed before decorticating the head segment proximal to the osteotomy with a saw for autologous humerus-to-scapula grafting. After decortication of the humeral head, the osteotomy was completed and the graft stored on the back table. The humeral rasp (Ascend flex, Stryker, Kalamazoo, MI, USA) was inserted and the wound packed with a sponge and temporarily closed. Several graft wedges from the head were impacted between bleeding bony surfaces and the spine of scapula extended up and reduced to an anatomical position. The ORIF was completed with clusters of angular stable screws angled 90° to each other on both sides of the fracture. Erroneous attempts of drilling must be avoided not to create stress risers. The deltoid and trapezius muscles were meticulously repaired to the scapular spine and plate (Fig. 5,6).
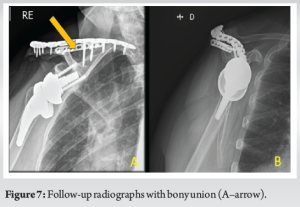
The deltopectoral approach was resumed, and the lateralized platform RSA (Aequalis Ascend Flex stem and Perform glenoid implants, Stryker, Kalamazoo, MI, USA) was implanted like in a primary setting (Fig. 7: MIO-RSA, 25 mm long post baseplate +3+2 mm lateralized, size 1B stem, +6 mm insert B, 1.5 mm offset tray in position 6, 36 mm + 2 mm eccentric glenosphere).
Based on our previous experience of ORIF of a Levy type IIa fracture associated with an RSA with the complication of plate adjacent secondary fracture [14], we recommend paying attention to eight recommendations for a successful ORIF of Levy-type II-III fractures associated with RSA, some of which we have applied progressively to our cases.
- CT evaluation of the bone stock. Is double plating possible? A 3D reconstruction and model are helpful to make this decision.
- Use of an adjustable arm holder to reduce and off-load the fracture during ORIF (Fig. 3A).
- Use of a posterior subacromial incision for finger palpation of the acromion and posterior-anterior drilling to prevent any erroneous drilling creating stress risers.
- Use of autologous bone graft in non-unions and if considered necessary.
- Filling of every drilled hole with a screw to prevent stress risers (avoid erroneous drilling).
- Preferred use of 90° locking plates with a minimum of five screws on either side of the fracture and a minimum of two locking screws per plate on either side of the fracture.
- Spanning of the acromion and spine of scapula with long plates and screws to avoid stress risers.
- Use of an abduction orthosis and passive ROM from the abducted position only for 8 weeks after the ORIF to let the fracture heal.
Outcome and follow-up
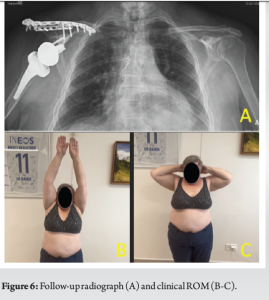
The patient did not suffer from post-operative complications (Fig. 6). A 30° abduction orthosis was used for 6-weeks and passive mobilization of the shoulder as tolerated above 90° was allowed for 4 weeks followed by active-assisted mobilization after the 4th week. During the 1st year of follow-up, we noted a significant improvement in ROM and clinical outcomes. There was a notable increase of 30 points in the Constant score and a remarkable 49% improvement in the subjective shoulder value (SSV) (Table 1).
This positive outcome is particularly noteworthy for a younger patient who had previously experienced substantial shoulder-related disability in both, work and activities of daily living. Bony union was observed on radiographs and a CT-scan on the 02.02.2021. Excellent clinical results persisted at the follow-up of more than 3 years after surgery (Fig. 7).
Isolated traumatic fractures of the scapular spine are infrequent and are often associated with a notable delay in both, diagnosis and definitive treatment. Notably, our review of the literature reveals a higher incidence of Levy type II and type III fractures resulting from falls. In a study by Nyffeler et al. (2020), seven scapular spine fractures were attributed to falls, with 6 of those leading to Levy type II or III fractures, while only one resulted in a Levy type I fracture [16]. Studies measuring the impact of forces from falls on the hand reported values ranging from approximately 1000 N for a fall from a shoulder height of 1 meter on a padded surface to 2800 N for a fall from a height of only 0.75 m [17,18]. Furthermore, cadaveric studies have observed fibula fractures, a bone which has a similar thickness compared to the acromion, already occurring at torque values of around 45 Nm during forced external rotation of the foot [19]. Considering the acromion, with an average length of 41 mm [20], as a potential lever arm for a cranial-directed force during a fall on an abducted arm, we postulate that sufficient torque could be generated to induce a fracture at the base of the acromion from an abduction-type mechanism. This hypothesis may be a plausible explanation for medially sited Levy type II and III fractures associated with falls and an upward directed force. Levy type I fractures often do not impose an important functional deficit after a phase of acute pain [12,21]. This can be elucidated through an examination of the anatomy of the deltoid muscle. Its posterior portion attaches to the scapular spine, the middle portion to the acromion, and the anterior portion to the clavicula [22]. Consequently, a fracture on the lateral side of the acromion would primarily affect the function of the middle portion of the deltoid enabling compensatory actions by the anterior and posterior portions for the overall function of the deltoid to be maintained. Non-operative treatment of medially sited SS fractures is associated with severely impaired ROM of the shoulder, loss of strength, and persistent pain [21,23]. The existing literature offers evidence supporting operative management of these fractures. However, there is inconsistency in both, reported outcomes and surgical techniques [24-27]. Following ORIF, the scapular spine becomes subjected to multidirectional forces, encompassing cranial forces of the trapezius, caudal pull of the deltoid, and various muscle insertions of the scapula. Given this complex biomechanical environment, we contend that the operative fixation technique and device configuration need to be sufficient to withstand these forces to achieve sustainable fixation over a sufficient time to allow for bony union and locked 90°-double plating has biomechanically been proven to be superior compared to a single locking plate [28]. In this case, we demonstrate durable mechanical stability and an excellent clinical outcome after correction, grafting and ORIF of a SS non-union with a previously described locked 90°-double plating technique with simultaneous lateralized RSA. Our aim is to contribute supplementary data to reinforce the evidence that operative intervention for Levy Type II and III scapular spine fractures can result in excellent clinical outcomes despite adverse forces generated from a lateralized RSA design.
If bone stock is sufficient to apply multiple screws of a locked 90°-double plate construct providing sufficient mechanical stability in the context of adverse forces of a lateralized RSA, excellent function and shoulder comfort can be expected. If the ORIF is successful in achieving union, the outcome may be far beyond results of non-operative management of these fractures associated with RSA, without a difference to primary RSA outcomes. This case illustrates the possible value of the plating technique for medial Levy-3 type SS fractures which may occur after forceful abduction from falls in patients with an RSA.
Scapular spine fractures present both diagnostic and surgical challenges. Clinicians should prioritize CT scans when evaluating scapular pain, tenderness and shoulder disability following falls with axial impact to the upper limb. For planning and performing locked 90°-double plating in RSA associated with Levy-type II-III fractures, the following five clinical recommendations are essential: (1) Assess the bone stock with a CT scan, (2) use a long superior plate and screws that span the scapular spine and acromion, (3) employ at least two locking screws on either side of each plate, (4) avoid stress risers from incorrect drilling, and (5) protect the fracture with an abduction sling for 6–8 weeks.
References
- 1.Zlowodzki M, Bhandari M, Zelle BA, Kregor PJ, Cole PA. Treatment of scapula fractures: Systematic review of 520 fractures in 22 case series. J Orthop Trauma 2006;20:230-3. [Google Scholar]
- 2.Schofer MD, Sehrt AC, Timmesfeld N, Störmer S, Kortmann HR. Fractures of the scapula: Long-term results after conservative treatment. Arch Orthop Trauma Surg 2009;129:1511-9. [Google Scholar]
- 3.Copuroglu C, Tan L, Copuroglu E, Ciftdemir M, Ozcan M. Pseudo-arthrosis of the spine of the scapula: A case report with a delayed diagnosis. Strategies Trauma Limb Reconstr 2014;9:173-7. [Google Scholar]
- 4.Thomas JD, Kehoe JL. Bone nonunion. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554385 [Last accessed on 2023). [Google Scholar]
- 5.Palaniappan P, Baalann KP. Fracture nonunion. Pan Afr Med J 2021;40:93. [Google Scholar]
- 6.Sathyendra V, Darowish M. Basic science of bone healing. Hand Clin 2013;29:473-81. [Google Scholar]
- 7.Bauer G, Fleischmann W, Dussler E. Displaced scapular fractures: Indication and long-term results of open reduction and internal fixation. Arch Orthop Trauma Surg 1995;114:215-9. [Google Scholar]
- 8.Wahlquist TC, Hunt AF, Braman JP. Acromial base fractures after reverse total shoulder arthroplasty: Report of five cases. J Shoulder Elbow Surg 2011;20:1178-83. [Google Scholar]
- 9.Lau SC, Large R. Acromial fracture after reverse total shoulder arthroplasty: A systematic review. Shoulder Elbow 2020;12:375-89. [Google Scholar]
- 10.Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J Shoulder Elbow Surg 2011;20:146-57. [Google Scholar]
- 11.Kozak T, Bauer S, Walch G, Al-Karawi S, Blakeney W. An update on reverse total shoulder arthroplasty: Current indications, new designs, same old problems. EFORT Open Rev 2021;6:189-201. [Google Scholar]
- 12.Walch G, Mottier F, Wall B, Boileau P, Molé D, Favard L. Acromial insufficiency in reverse shoulder arthroplasties. J Shoulder Elbow Surg 2009;18:495-502. [Google Scholar]
- 13.Schenk P, Aichmair A, Beeler S, Jentzsch T, Gerber C. Clinical results of conservative versus operative treatment of acromial and scapular spine fractures following reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2022;31:2076-81. [Google Scholar]
- 14.Bauer S, Traverso A, Walch G. Locked 90°-double plating of scapular spine fracture after reverse shoulder arthroplasty with union and good outcome despite plate adjacent acromion fracture. BMJ Case Rep 2020;13:e234727. [Google Scholar]
- 15.Yu KE, Marigi EM, Austin DC, Tangtiphaiboontana J, Esper R, Barlow JD, et al. Operative treatment of acromial and scapular spine fracture nonunions complicating reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2024;S1058-2746(24):00465-8. [Google Scholar]
- 16.Nyffeler RW, Altioklar B, Bissig P. Causes of acromion and scapular spine fractures following reverse shoulder arthroplasty: A retrospective analysis and literature review. Int Orthop 2020;44:2673-81. [Google Scholar]
- 17.DeGoede KM, Ashton-Miller JA. Fall arrest strategy affects peak hand impact force in a forward fall. J Biomech 2002;35:843-8. [Google Scholar]
- 18.Chiu J, Robinovitch SN. Prediction of upper extremity impact forces during falls on the outstretched hand. J Biomech 1998;31:1169-76. [Google Scholar]
- 19.Markolf KL, Schmalzried TP, Ferkel RD. Torsional strength of the ankle in vitro. The supination-external-rotation injury. Clin Orthop Relat Res 1989;246:266-72. [Google Scholar]
- 20.Saha S, Vasudeva N. Morphometric evaluation of adult acromion process in North Indian Population. J Clin Diagn Res 2017;11:AC08-11. [Google Scholar]
- 21.Boltuch A, Grewal G, Cannon D, Polisetty T, Levy JC. Nonoperative treatment of acromial fractures following reverse shoulder arthroplasty: Clinical and radiographic outcomes. J Shoulder Elbow Surg 2022;31:S44-56. [Google Scholar]
- 22.Moser T, Lecours J, Michaud J, Bureau NJ, Guillin R, Cardinal É. The deltoid, a forgotten muscle of the shoulder. Skeletal Radiol 2013;42:1361-75. [Google Scholar]
- 23.Groot D, Giesberts AM, van Mourik JB. Spontaneous scapular spine fracture related to rotator cuff pathology: A report of two cases. Strategies Trauma Limb Reconstr 2012;7:105-7. [Google Scholar]
- 24.Toft F, Moro F. Does ORIF of rare scapular spine fractures sustained after reverse shoulder arthroplasty benefit elderly patients? A case-series appraisal. Orthop Traumatol Surg Res 2019;105:1521-8. [Google Scholar]
- 25.Streck LE, Straub A, Boettner F, Rudert M, List K. Treatment of symptomatic pseudarthrosis following acromion fracture with a patient-specific implant customized on a 3D-printed scapula. Oper Orthop Traumatol 2023;35:270-7. [Google Scholar]
- 26.As-Sultany M, Tambe A, Clark DI. Nonunion of a scapular spine fracture: Case report and management with open reduction, internal fixation, and bone graft. Int J Shoulder Surg 2008;2:64-7. [Google Scholar]
- 27.Cassidy JT, Paszicsnyek A, Ernstbrunner L, Ek ET. Acromial and scapular spine fractures following reverse total shoulder arthroplasty-a systematic review of fixation constructs and techniques. J Clin Med 2022;11:7025. [Google Scholar]
- 28.Katthagen JC, Sußiek J, Frank A, Wermers J, Schliemann B, Raschke MJ. Double plating is associated with higher fixation strength than single plating in osteoporotic fractures of the scapular spine: A biomechanical study. Arch Orthop Trauma Surg 2022;142:1859-64. [Google Scholar]