The cases underscore the importance of initial angular stable fixation for femoral neck Pauwels’ 3 fractures and the potential to prevent hip replacement when facing non-union. The present approach, considering the diamond concept, advocates for correct osteosynthesis and supplementation with bone marrow concentrate, demineralized bone matrix, and supplementation with morselized allograft, growth factors, and bone marrow concentrate, offering insights into optimizing non-union management for future considerations
Dr. Cornu Olivier, Department of Orthopaedic and Trauma, Cliniques Universitaires Saint-Luc UCL, av Hippocrate 10 - 1200, Brussels, Belgium. E-mail: olivier.cornu@uclouvain.be
Introduction: Femoral neck fractures in young adults, particularly Pauwels’ 3 fractures with angles exceeding 70°, pose challenges in determining optimal surgical interventions due to limited clinical trial data. Complications such as avascular necrosis, non-union, and shortening hinder the healing process. Existing fixation methods, including multiple cannulated screws and sliding hip screws, have shown non-union rates of nearly 9% in young patients. Bone healing relies on various factors, both patient-independent and patient-dependent, and deficient bone regeneration may necessitate interventions such as cellular supplementation.
Case Report: Two cases of Pauwels’ 3 fractures in young individuals were treated with a multimodal approach involving mechanical stabilization and biological supplementation. Delayed fracture consolidation and non-union were observed in the initial surgical interventions, leading to the consideration of total hip arthroplasty. However, a second option, involving dynamic hip screw fixation, morselized bone allograft, demineralized bone matrix, and bone marrow concentrate, was chosen based on the patient’s age and absence of femoral head necrosis. Both patients successfully achieved bone union and full recovery 6 months postoperatively.
Conclusion: The cases underscore the importance of treating femoral neck fractures based on biomechanical principles and highlight the significance of restoring a favorable biological and mechanical environment for fracture healing. A comprehensive approach involving growth factors, bone scaffolds, and mesenchymal stem cells is crucial, along with considerations for the diamond concept, encompassing biomechanics, vascularity, patient factors, and prior bone infection.
Keywords: Femoral neck fracture, non-union, angular dynamic stable fixation, bone marrow concentrate, demineralized bone matrix, morselized cancellous bone.
In young adults (≤60 years), femoral neck fractures represent high-energy traumas, often associated with avascular necrosis, non-union, and significant shortening [1]. Determining the optimal timing, surgical technique, and implant to treat Pauwels’ 3 fractures (angles >50°) in young patients is challenging due to the lack of clinical trials [2]. A high-angle femoral neck fracture leads to increased shear forces and instability, predisposing to non-union [3, 4]. The main fixation methods for young intracapsular hip fractures are multiple cannulated screws and sliding hip screws [4]. In a meta-analysis, nearly 9% of young patients with femoral neck fractures treated with internal fixation, developed non-union [5]. Bone healing depends on factors such as the mechanical environment, vascular supply, growth factors, inflammatory mediators, osteogenic progenitor cells, and the patient’s medical history. Failure to heal can result from patient-independent (fracture type, energy intensity, displacement, injury extent, bone loss, and infection) and patient-dependent factors (age, sex, comorbidities, smoking, metabolic diseases, medication, nutritional deficiencies, and genetic disorders) [6, 7]. In cases of deficient bone regeneration, injecting healthy cells at the non-union site promotes bone healing [6]. Morselized bone allograft, growth factors from demineralized bone matrix (DBM), and bone marrow concentrate (BMC) are used together to promote healing through callus formation based on three principles: Osteoconduction, osteoinduction, and osteogenic cells [8]. A multimodal approach was employed in two reported cases, combining mechanical stabilization and biological supplementation to promote bone healing [6].
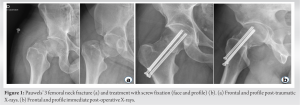
A 32-year-old male presented with a Pauwels’ 3 fracture of the right femoral neck following a skateboard fall (Fig. 1a).
This fracture was initially treated with internal fixation using three screws (Fig. 1b) but 5 months later, delayed fracture consolidation was observed (Fig. 2 and 3). The patient’s daily life was affected, and total hip arthroplasty (THA) was considered before the patient consulted our department.
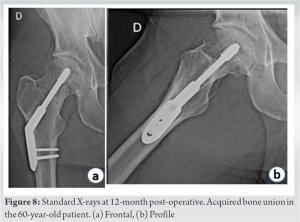
A 60-year-old male with a Pauwels’ 3 fracture of the right femoral neck following a bicycle accident also underwent surgical treatment with three screws. However, non-union occurred due to a lack of stability (Fig. 4), leading to pain and impaired walking. THA was considered before seeking a second opinion.
Non-union was defined as the failure of the fractured bone to heal properly within the expected timeframe, resulting in persistent instability and pain at the fracture site and radiological signs of lack of bone consolidation.
When diagnosing non-union of the transcervical femoral fracture, two treatment options were discussed with these patients: THA and cure of pseudarthrosis by dynamic hip screw (DHS) in conjunction with morselized bone grafting, DBM and BMC at the fracture site.
One of the two patients, a smoker, was advised to quit smoking. Considering the patient’s age and the absence of femoral head necrosis, the second option was chosen to promote healing of the cervical neck pseudarthrosis, while avoiding the need for THA.
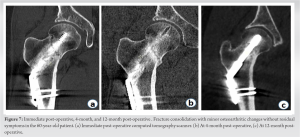
Morselized bone allografts were obtained from living donors who consented to donation. Morsels were prepared from femoral heads and processed with solvent-detergents before being sterilized by gamma irradiation at a minimal 25 kGy dose and preserved frozen. DBM was obtained from <40-year-old cadaveric donors’ long bones, in respect to the Belgian organ and tissue donation regulation. Cortical bone was cut into small fragments, chemically processed with solvent-detergent before being grounded in 400–800 µm particles, and demineralized with chlorhydric acid. DBM was further freeze-dried and sterilized by gamma irradiation at a minimum 25 kGy dose, under dry ice, and then kept at room temperature until use. The surgical procedure involved removing existing three-screw fixation and replacing it with a 135° DHS (Depuy-Synthes, Swiss) after fracture realignment. In addition, 60 cc of bone marrow was aspirated from the anterior iliac crest and concentrated by centrifugation at 3200 RPM for 15 min (BioCUE®, Zimmer-Biomet, IN, USA) (Fig. 5a). BMC was mixed with morselized, processed cancellous allograft. In addition, an osteoinductive bone substitute was added, prepared from ground cortical allograft bone, demineralized with hydrochloric acid, and sterilized by gamma irradiation. The DBM obtained from the cortical bone expresses osteoinductive growth factors (Fig. 5b). . Both patients achieved bone union and full recovery 6 months postoperatively (Fig. 6-8).
In younger patients with non-union, preserving the hip joint is preferable, dependent on activity level and comorbidities for those aged 50–60 [4]. Internal fixation remains the optimal treatment for initial femoral neck fracture with no significant difference between cannulated compression screw and sliding hip screw regarding non-union development [9]. Revision of internal fixation with bone grafting provides excellent results for healing non-union of femoral neck fractures [10]. Biologically, the three fundamental principles for bone formation are addressed in the management of femoral neck non-union [11]. Autogenous bone marrow provides osteogenic properties and centrifugation concentrates necessary elements, increasing efficiency [12]. Corticocancellous bone allograft offers osteoconductivity and mechanical support for cells differentiating into osteogenic cells, while DBM provides osteoinductive activity, enabled by bone morphogenetic proteins present in the DBM [11, 13]. Mechanically, DHS provides static and dynamic compression of the fracture line, promoting fracture healing [14]. A study on 50 patients with non-union treated with bone marrow aspirate concentrate and cancellous allograft showed no significant difference compared to the iliac crest. The combination of bone marrow aspirate concentrate with cancellous allograft resulted in a 75% non-union healing rate [15]. Percutaneous bone marrow injection offers a minimally invasive alternative, reducing complications associated with open autogenous bone grafting, and its potential morbidity [8]. The use of bone marrow aspirate concentrate could be a future solution to optimize non-union healing and prevent post-operative complications [8, 15].
The presented cases highlight the importance of treating femoral neck fractures based on biomechanical principles and the added value of a comprehensive approach to restore a favorable biological and mechanical environment for fracture healing. Bone restoration and regeneration involving growth factors, bone scaffolds, and mesenchymal stem cells (triangular concept) are crucial. However, the mechanical environment should not be underestimated and therefore surgeons should approach any non-union with respect to the diamond concept, including biomechanical considerations, vascularity, patient factors, and finally, potential prior bone infection.
Non-union of femoral neck fractures is a common complication requiring comprehensive management for primary healing. In the case of non-union, restoring a favorable mechanical and biological environment with bone grafts, growth factors, and mesenchymal cells, along with improving patient medical status, when needed and possible, should be prioritized. The cases emphasize the importance of initial angular stable fixation for Pauwels’ 3 fractures and the potential to avoid joint replacement through correct osteosynthesis and supplementation.
References
- 1.Slobogean GP, Sprague SA, Scott T, McKee M, Bhandari M. Management of young femoral neck fractures: Is there a consensus? Injury 2015;46:435-40. [Google Scholar]
- 2.Shen M, Wang C, Chen H, Rui YF, Zhao S. An update on the Pauwels classification. J Orthop Surg Res 2016;11:161. [Google Scholar]
- 3.Liporace F, Gaines R, Collinge C, Haidukewych GJ. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am 2008;90:1654-9. [Google Scholar]
- 4.Deakin DE, Guy P, O’Brien PJ, Blachut PA, Lefaivre KA. Managing failed fixation: Valgus osteotomy for femoral neck nonunion. Injury 2015;46:492-6. [Google Scholar]
- 5.Slobogean GP, Sprague SA, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury 2015;46:484-91. [Google Scholar]
- 6.Piuzzi NS, Oñativia JI, Vietto V, Franco JV, Griffin XL. Autologous bone marrow‐derived and blood‐derived biological therapies (including cellular therapies and platelet‐rich plasma) for bone healing in adults. Cochrane Database Syst Rev 2018;2018:CD013050. [Google Scholar]
- 7.Hak DJ, Fitzpatrick D, Bishop JA, Marsh JL, Tilp S, Schnettler R, et al. Delayed union and nonunions: Epidemiology, clinical issues, and financial aspects. Injury 2014;45:S3-7. [Google Scholar]
- 8.Kumar S, Kumar N, Kumar A. Observation on the role of bone marrow aspirate in the delayed union and non union of long bones. Int J Orthop Sci 2021;7:259-62. [Google Scholar]
- 9.Xia Y, Zhang W, Zhang Z, Wang J, Yan L. Treatment of femoral neck fractures: Sliding hip screw or cannulated screws? A meta-analysis. J Orthop Surg Res 2021;16:54. [Google Scholar]
- 10.Mathews V, Cabanela ME. Femoral neck nonunion treatment. Clin Orthop Relat Res 2004;419:57-64. [Google Scholar]
- 11.Delloye C, Cornu O, Druez V, Barbier O. Bone allografts: What they can offer and what they cannot. J Bone Joint Surg Br 2007;89:574-9. [Google Scholar]
- 12.Yang J, Zhang X, Liang W, Chen G, Ma Y, Zhou Y, et al. Efficacy of adjuvant treatment for fracture nonunion/delayed union: A network meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 2022;23:481. [Google Scholar]
- 13.Pietrzak WS, Woodell-May J, McDonald N. Assay of bone morphogenetic protein-2, -4, and -7 in human demineralized bone matrix. J Craniofac Surg 2006;17:84-90. [Google Scholar]
- 14.Baldwin P, Li DJ, Auston DA, Mir HS, Yoon RS, Koval KJ. Autograft, allograft, and bone graft substitutes: Clinical evidence and indications for use in the setting of orthopaedic trauma surgery. J Orthop Trauma 2019;33:203-13. [Google Scholar]
- 15.Lin K, VandenBerg J, Putnam SM, Parks CD, Spraggs-Hughes A, McAndrew CM, et al. Bone marrow aspirate concentrate with cancellous allograft versus iliac crest bone graft in the treatment of long bone nonunions. OTA Int 2019;2:e012. [Google Scholar]