Tibia diaphyseal Aneurysmal Bone Cysts (ABCs) have a rare presentation for which wide margin resection of the tumor along with ipsilateral fibula strut grafting is a viable surgical method
Dr. Sunit K Pani, Department of Orthopaedics, IMS and SUM Hospital, Siksha O Anusandhan (Deemed to be) University, Bhubaneswar, Odisha, India. E-mail: pani.sunit@gmail.com
Introduction: Aneurysmal bone cyst (ABC) is a benign, expansile hemorrhagic tumor usually presenting in the metaphyseal region of long bones. Diaphyseal ABCs are rare and prone to pathological fracture and increased morbidity. Treatment options are centered around the site and size of the lesion.
Case Report: We report a case of a large ABC in the tibia diaphysis in an 18 year female. The patient was treated with wide margin resection followed by an ipsilateral fibular bone graft of 5 cm, which was followed by good post-operative recovery without any recurrence. At 12-month follow-up, the patient had painless mobility with a full functional range of motion of the affected limb.
Conclusion: An early rehabilitation and return to active life can be achieved in diaphyseal ABCs with careful planning and post-operative care.
Keywords: Aneurysmal bone cyst, ipsilateral fibula graft, pathological fracture, bone tumor.
Aneurysmal bone cyst (ABC) usually presents as an expansile hemorrhagic tumor in the metaphysis of long bones [1]. Their presentation on the surface diaphysis of long bones is quite rare and more prone to pathological fractures [2]; hence, they pose a unique set of challenges in treatment and rehabilitation. Typically, patients present with complaints of pain at the involved site or pathological fractures. ABCs must be differentiated from other forms of bone cyst. Investigations include radiographs and magnetic resonance imaging (MRI) of the affected site. Radiographs show well-defined expansile osteolytic lesions with sclerosed margins. Multiple fluid levels on an MRI are characteristic of ABC although not specific [3]. Histopathology remains the gold standard in the diagnosis of ABC. There are a wide variety of treatment options available for treating such lesions. The standard of care for long bones ABCs is curettage and void filling bone grafts with or without local adjuvants [4]. Surgical planning is guided by the location and size of the lesion.
An 18-year-old female presented to the outpatient department with a 10 days history of acute onset right leg pain associated with swelling. The pain had gradually progressed in the last 10 days and made it difficult for her to walk. On examination, there was a swelling of approximately 2 cm × 2 cm on the anterior aspect of the right mid tibial shaft. The swelling was tender on palpation with a local rise of temperature. It was not associated with any constitutional symptoms. A plain radiograph of the right leg was obtained in both antero-posterior and lateral views with the arrow showing cystic lesion in the midshaft of the tibia (Fig. 1).
MRI showed a well-circumscribed cystic lesion (Fig. 2).
The lesion was biopsied and sent for histopathological examination which revealed large areas of hemorrhage separated by connective tissue septa, suggestive of an ABC. Due to a large size (4 cm) and location (cortical midshaft tibia) which would lead to a large post-excision defect an ideal bone graft had to be chosen. A fibular graft from the contralateral side was considered for the case. However, the parents of the patient were reluctant for any operative procedure on the contralateral side. Hence it was decided to proceed with an ipsilateral fibular graft. After a written informed consent patient was taken up for surgery under spinal anaesthesia. After thorough dissection, the involved part of the bone was resected with a 1 cm margin followed by curettage. The resected piece was measured intraoperative (5 cm). A similar length bone graft was obtained from the midshaft of the fibula and placed at the tibial defect (Fig. 3).
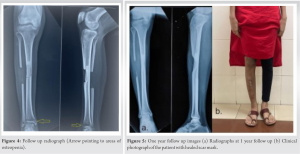
Post-surgery patient was put on an above-knee slab and advised against weight-bearing. The post-operative wound healed well. Partial weight-bearing was started at 6 weeks. The patient was kept on monthly follow-up. Gradually, the patient was symptomatically better. Radiological signs of graft uptake were visible on X-rays. At 7-month post-surgery patient was able to bear weight without a walker. On radiographs, some areas of osteopenia were noticed in the distal tibia and talar region which gradually improved back to normal in subsequent follow-up (Fig. 4).
At the end of 1-year follow-up, patient had complete graft uptake on radiographs and had pain-free ambulation with a full active range of motion of the affected leg without any limitation of activities of daily living (Fig. 5).
Since its first description as a separate pathological entity by Jaffe, ABC s have been studied extensively [5, 6]. The median age of presentation of ABC s is 13 years. The patient, in this case, was aged 18 years. ABC s have a wide variety of presentations. Although the usual presentation is in the metaphyseal part however there have been several instances of it being reported in the diaphyseal area or with physeal extension [7]. The etiopathogenesis of ABC however remains controversial with no consensus. Earlier it was believed to be reactive due to underlying arteriovenous malformations. The bone void arising out of the increased venous pressure was filled with blood, resulting in a typical ABC appearance. Though recent study by Ye et al. has shown that ABC s may be independent neoplasms with activation of the USP6 gene [8], ABC does not however have the potential for malignancy.
When encountering a lesion suggestive of ABC in the tibia, it is important to consider several differential diagnoses which mainly include unicameral bone cyst, telangiectatic osteosarcoma and giant cell tumour and chondroblastoma. Out of all the differentials since telangiectatic osteosarcoma is a malignant bone tumour, it is evident that it possesses the biggest diagnostic obstacle [9-11]. Histologically, ABC s are characterized by innumerable osteoclastic giant cells scattered throughout the lesion. These giant cells are multinucleated and are located centrally in the blood-filled intertrabecular spaces. The stroma of the tumor consists of fibrous tissue as well as spindle-shaped fibroblasts which are found in it [12]. The size and site of the presentation of ABC are the most crucial factor for determining the treatment course [13]. Historically, studies have shown that en bloc excision of the cyst has excellent outcomes in terms of recurrence. Studies have reported up to 100% localized control after en bloc excision [9, 14, 15]. Due to the large size and location of the lesion, it was decided to proceed with en bloc excision, followed by bone grafting. Curettage of ABCs have returned highly variable recurrence rates with some studies reporting a recurrence rate up to 59% [16]. In major weight-bearing bones such as the femur and tibia, the choice of treatment will have a grave impact on the patient’s functioning. Any recurrence can lead to the requirement for surgery and severe limitation in functional mobility. Diaphyseal fracture on progression involves the adjacent cortex and invariably may lead to pathological fracture. Excellent radiological and functional outcomes can be achieved in diaphyseal ABCs with careful planning and post-operative care.
An early rehabilitation and return to active life is possible with wide margin excision of the tumor combined with ipsilateral fibula strut grafting for surgical management of tibia diaphyseal ABCs. This surgical method has not been mentioned in the literature with a follow-up of more than a year in the management of diaphyseal ABCs.
Excellent functional results with no recurrence can be achieved by this method for management of diaphyseal ABCs.
References
- 1.Mascard E, Gomez-Brouchet A, Lambot K. Bone cysts: Unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res 2015;101:S119-27. [Google Scholar]
- 2.Sharma PK, Kundu ZS, Lamba A, Singh S. Diaphyseal aneurysmal bone cysts (ABCs) of long bones in extremities: Analysis of surgical management and comparison with metaphyseal lesions. J Clin Orthop Trauma 2021;18:74-9. [Google Scholar]
- 3.Tsai JC, Dalinka MK, Fallon MD, Zlatkin MB, Kressel HY. Fluid-fluid level: A nonspecific finding in tumors of bone and soft tissue. Radiology 1990;175:779-82. [Google Scholar]
- 4.Muratori F, Mondanelli N, Rizzo AR, Beltrami G, Giannotti S, Capanna R, et al. Aneurysmal bone cyst: A review of management. Surg Technol Int 2019;35:325-35. [Google Scholar]
- 5.Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst: With emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg 1942;44:1004-25. [Google Scholar]
- 6.Bonakdarpour A, Levy WM, Aegerter E. Primary and secondary aneurysmal bone cyst: A radiological study of 75 cases. Radiology 1978;126:75-83. [Google Scholar]
- 7.Dyer R, Stelling CB, Fechner RE. Epiphyseal extension of an aneurysmal bone cyst. AJR Am J Roentgenol 1981;137:172-3. [Google Scholar]
- 8.Ye Y, Pringle LM, Lau AW, Riquelme DN, Wang H, Jiang T, et al. TRE17/USP6 oncogene translocated in aneurysmal bone cyst induces matrix metalloproteinase production via activation of NF-κB. Oncogene 2010;29:3619-29. [Google Scholar]
- 9.Campanacci M, Capanna R, Picci P. Unicameral and aneurysmal bone cysts. Clin Orthop Relat Res 1986;204:25-36. [Google Scholar]
- 10.Rapp TB, Ward JP, Alaia MJ. Aneurysmal bone cyst. J Am Acad Orthop Surg 2012;20:233-41. [Google Scholar]
- 11.Mendenhall WM, Zlotecki RA, Gibbs CP, Reith JD, Scarborough MT, Mendenhall NP. Aneurysmal bone cyst. Am J Clin Oncol 2006;29:311-5. [Google Scholar]
- 12.Restrepo R, Zahrah D, Pelaez L, Temple HT, Murakami JW. Update on aneurysmal bone cyst: Pathophysiology, histology, imaging and treatment. Pediatr Radiol 2022;52:1601-14. [Google Scholar]
- 13.Jain M, Tripathy SK, Mishra NP, Ayyanar P, Singh AK. Primary aneurysmal bone cyst in the iliac bone: A case report. J Orthop Case Rep 2024;14:109-13. [Google Scholar]
- 14.Mankin HJ, Hornicek FJ, Ortiz-Cruz E, Villafuerte J, Gebhardt MC. Aneurysmal bone cyst: A review of 150 patients. J Clin Oncol 2005;23:6756-62. [Google Scholar]
- 15.Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK. Aneurysmal bone cyst. A clinicopathologic study of 238 cases. Cancer 1992;69:2921-31. [Google Scholar]
- 16.Biesecker JL, Marcove RC, Huvos AG, Miké V. Aneurysmal bone cysts. A clinicopathologic study of 66 cases. Cancer 1970;26:615-25. [Google Scholar]