Posterior Knee pain even after conservative treatment needs thorough examination and radiological evaluation and should not be neglected and mucoid degeneration of PCL may be one of the causes.
Amit Kumar Jha, Consultant Arthroscopic Surgeon, Department of Orthopedics, Apex Superspeciality Hospital, Varanasi, Uttar Pradesh, India. E-mail: jha2401@gmail.com
Introduction: Mucoid degeneration of the cruciate ligament is a well-known entity, but symptomatic lesions are rare. It is even rarer to find symptomatic posterior cruciate ligament mucoid degeneration than the anterior cruciate ligament.
Case Report: A 63-year-old male presented to our hospital complaining of posterior knee pain was induced when the knee approached full flexion without episodes of trauma, despite conservative treatment over the preceding 8 months, his symptoms persisted. Physical examination of the right knee revealed on terminal flexion and cross-leg sitting pain get exaggerated. Right knee ROM 0–110° and a further terminal flexion was limited and painful. On ligament examination, posterior sagging and Lachman test were negative, and no clinical finding indicative of ligament insufficiency was noted. Magnetic resonance imaging showed a diffusely thickened posterior cruciate ligament with increased signal intensity on the T2-weighted sequence. A intact PCL fibers were observed with continuous margins from origin to insertion. Based on the patient’s history and the magnetic resonance imaging findings, we suspected mucoid degeneration of the posterior cruciate ligament as the cause of the patient’s symptoms. Since conservative treatment had failed to relieve the symptoms, arthroscopic treatment was indicated. Arthroscopic examination revealed yellowish crumbly tissues along the thickened posterior cruciate ligament. Tension and bulk of the posterior cruciate ligament were well preserved. Curettage of degenerative tissue and decompression of the posterior cruciate ligament resulted in symptom relief without instability of the knee joint. We did a notchplasty of the medial wall and roof to accommodate the posterior cruciate ligament and avoid impingement.
Conclusions: Arthroscopic decompression of the posterior cruciate ligament may relieve knee pain and facilitate early return with good functional results.
Keywords: Mucoid degeneration of PCL, posterior knee pain, arthroscopic decompression of PCL
Mucoid degeneration of the anterior cruciate ligament (ACL) is a benign knee pathology with a frequency of 1.8–5.3% [1-8]. Prevalence in magnetic resonance imaging (MRI) is 1.8–5.3%, but not all lesions are symptomatic. Mucoid degeneration of ACL is more common and literature has also reported many cases, but for PCL only a few cases have been reported in English literature. Because unlike meniscal tears and chondral defects, reported mucoid degeneration of PCL is a rare cause of knee pain. However, there are some situations that make knee pain. We herein describe a case of PCL mucoid degeneration presented with impingement symptoms.
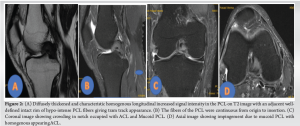
A 63-year-old male presented to our hospital complaining of posterior knee pain was induced when the knee approached full flexion without episodes of trauma. Despite conservative treatment over the preceding 8 months, his symptoms persisted. Physical examination of the right knee revealed on terminal flexion and cross-leg sitting pain get exaggerated. Right knee ROM 0–110° and a further terminal flexion was limited and painful. On ligament examination, posterior sagging and Lachman test were negative, and no clinical finding indicative of ligament insufficiency was noted. The radiograph of the knee was normal (Fig. 1). Magnetic resonance imaging (MRI) revealed longitudinal increased signal intensity area within the PCL on T2-weighed images with an adjacent defined rim of hypointense PCL fibers (Fig. 2). The characteristics of those images were coincident with a “Tram-Track” appearance according to the description by McMonagle et al. [3]. Based on the patient’s history and the MRI findings, we suspected mucoid degeneration of the PCL as the cause of the patient’s symptoms. Since conservative treatment had failed to relieve the symptoms, arthroscopic treatment was indicated. On arthroscopic observation, the yellowish tissue was present in deeper regions while retention of fluid was not observed within the ligament substance.
Arthroscopic treatment consists of PCL reduction-plasty by debridement of yellowish material in the PCL fiber and radiofrequency ablation (RFA) proves to reduce the volume of the hypertrophied PCL (Figure 03 and 04). The goal was to return the PCL to its original volume. Tension and bulk of the PCL were well preserved. Other intra-articular tissues such as ACL, menisci, and cartilage were intact. The PCL tissue was split, and evidently, degenerated tissue was carefully removed while meticulous care was taken to preserve the longitudinal fiber of the PCL. We restricted curettage when the thickness of PCL decreased because the extensive curettage would cause damage of PCL tensions. We did medial wall notchplasty and checked again for impingement in flexion and extension. After the arthroscopic procedure, the Lachman test was negative ruling out instability. The meniscus was normal. The cartilage of the femoral condyle and patella was normal.

Post-operatively, the patient was allowed to bear full weight on the following day. Rehabilitation protocol included early motion and quadriceps strengthening exercises.
The true incidence of PCL mucoid degeneration is difficult to assess because it is, as in our patient population, typically asymptomatic and incidentally noted. As a point of reference, Bergin et al. reported that the incidence of ACL mucoid degeneration is 1.0% (44/4221) compared with an incidence of PCL mucoid degeneration in reference was 0.1% (14/12972) [4, 9]. Mucoid degeneration of PCL has been described before and there are few case reports but these cases are of asymptomatic patients or with PCL symptoms in terms of pain on flexion with restricted terminal flexion [5, 7]. Mucoid degeneration of PCL can produce symptoms of pain on flexion or restricted terminal flexion. Our patient presented with pain on terminal deep flexion after 110°. MRI images in the sagittal plane showed PCL is thickened and characteristic homogeneous longitudinal increased signal intensity in the PCL in all planes on proton density and T2 images with an adjacent well-defined intact rim of hypo-intense PCL fibers that give the PCL a tram-track appearance and on coronal images notch is crowded with hypertrophic PCL. Thickened PCL with a yellowish hue are characteristic and the PCL was led with a yellowish substance. The yellowish hue was not liquid, but a fibrous tissue like ACL mucoid degeneration as described in reports on ACL mucoid degeneration [6, 10]. We debride a yellowish substance to debulk a PCL as precisely as possible to avoid posterior instability with medial wall notchplasty. Debulking of PCL hue resulted in immediate pain relief in full flexion and improved range of motion without instability. At 1 year follow-up, the patient remains asymptomatic without instability.
Almost Mucoid degeneration of the posterior cruciate ligament may be asymptomatic, but in the case of PCL mucoid degeneration with pain and restriction in terminal flexion, enlarged PCL can make impingement in the femoral notch with ACL. Then, Partial debulking surgery of PCL is an effective treatment to pain relief and restoring the range of motion of the knee.
Posterior cruciate ligament mucoid degeneration may be a cause of posterior knee pain and even after conservative treatment the pain may not subside. Arthroscopic decompression may be a good treatment in those cases.
References
- 1.Wang JH, Jangir RR. Mucoid degeneration of posterior cruciate ligament with secondary impingement of anterior cruciate ligament: A rare case report. J Orthop Case Rep 2015;5:44-6. [Google Scholar]
- 2.Morice A, Coupry A, Lintz F, Robert H. Reduction plasty for hypertrophic anterior cruciate ligament mucoid degeneration: Clinical and knee laxityoutcomes in 23 cases. Orthop Traumatol Surg Res 2013;99:693-7. [Google Scholar]
- 3.McMonagle JS, Helms CA, Garrett WE, Vinson EN. Tram-track appearance of the posterior cruciate ligament (PCL): Correlations with mucoid degeneration, ligamentous stability, and diferentiation from PCL tears. AJR Am J Roentgenol 2013;201:394-9. [Google Scholar]
- 4.Bergin D, Morrison WB, Carrino JA, Nallamshetty SN, Bartolozzi AR. Anterior cruciate ligament ganglia and mucoid degeneration: Coexistenceand clinical correlation. AJR Am J Roentgenol 2004;182:1283-7. [Google Scholar]
- 5.Okazaki K, Deguchi S, Katai K, Iwamoto Y. Mucoid degeneration of the posterior cruciate ligament: A case report. Knee Surg Sports Traumatol Arthrosc 2001;19:105-7. [Google Scholar]
- 6.Cha JR, Lee CC, Cho SD, Youm YS, Jung KH. Symptomatic mucoid degeneration of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2013;21:658-63. [Google Scholar]
- 7.Shoji T, Fujimoto E, Sasashige Y. Mucoid degeneration of the posterior cruciate ligament: A case report. Knee Surg Sports Traumatol Arthrosc 2010;18:130-3. [Google Scholar]
- 8.Lintz F, Pujol N, Boisrenoult P, Bargoin K, Beaufils P, Dejour D. Anterior cruciate ligament mucoid degeneration: A review of the literature and management guidelines. Knee Surg Sports Traumatol Arthrosc 2011;19:1326-33. [Google Scholar]
- 9.Kaatee R, Kjartansson O, Brekkan A. Intraarticular ganglion between the cruciate ligaments of the knee. Acta Radiol 1994;35:434-6. [Google Scholar]
- 10.Bui-Mansfield LT, Youngberg RA. Intraarticular ganglia of the knee: prevalence, presentation, etiology, and management. AJR Am J Roentgenol 1997;168:123-7. [Google Scholar]