This case demonstrates that Bone Morphogenic Protein-2 can promote healing of nonunion humeral shaft fractures in the geriatric population.
Dr. Ryan M. Tapio, Washington State University, Elson S. Floyd College of Medicine, 412 E Spokane Falls Blvd Spokane, WA 99202, USA. E-mail: ryan.tapio@wsu.edu
Introduction: Bone morphogenic protein-2 (BMP-2) is a potent growth factor cytokine, with indications for interbody spinal fusion surgery and open tibial shaft repairs due to its osteoinductive properties. Off-label usage of BMP-2 has been documented; however, there are limited studies regarding the efficacy of using BMP-2 in non-union humeral shaft fractures.
Case Report: We present a case of a comminuted left humeral shaft fracture with pseudoarthrosis in a 64-year-old woman. Due to the patient’s significant comorbidities, initial fracture management focused on non-surgical intervention with the use of a humeral cuff to correct the fracture. However, the patient’s report of persistent and significant pain and serial radiographs indicating poor healing with a non-union fracture prompted surgical intervention. The patient underwent an open reduction and internal fixation (ORIF) with the application of one pledget of BMP-2 at the fracture site to promote osteogenesis. To the best of our knowledge, there is limited information about the efficacy of using BMP-2 for humeral fractures.
Conclusion: Six months following the surgery, radiographs have shown appropriate fracture healing of the left humerus without loosening of hardware and other significant complications. The usage of BMP-2 in this patient has shown to be effective in promoting the healing of her nonunion humeral shaft fracture. Although BMP-2 has typically been FDA indicated for use in lumbar interbody spinal fusion surgery and open tibial shaft repairs, this case demonstrates that BMP-2 can also promote healing of non-union humeral shaft fractures in a safe and effective manner.
Keywords: Bone morphogenetic protein-2, humeral fracture non-union, pseudarthrosis, fracture, bone healing.
Bone morphogenetic protein 2 (BMP-2) is a growth factor belonging to the transforming growth factor-beta superfamily that has been extensively studied since its discovery in 1965 by Marshall Urist [1, 2]. BMP-2 is the main factor that differentiates mesenchymal stem cells (MSCs) into osteoblasts, playing a large osteoinductive role in adults [1, 2]. At present, the U.S. Food and Drug Administration (FDA) has approved the use of recombinant human BMP-2 (rhBMP-2) for interbody spinal fusion (approved 2002), open tibial shaft repair (approved 2004), and maxillary sinus reconstructive surgery (approved 2007) due its osteoinductive properties [1]. Although there have been numerous studies conducted since rhBMP-2 was FDA approved that have brought awareness to its adverse effects, rhBMP-2 is the only osteoinductive growth factor that is FDA approved for use as a bone graft substitute and has many medical benefits such as decreased complications and medical costs [1, 3]. The usage of rhBMP-2 has grown in popularity as it was used in only 0.7% of all spinal fusions in 2002, to 24.9% of primary spinal fusions and 36.6% revision spinal fusions in 2006 [1]. The surge in usage of rhBMP-2 since 2002 has also increased its off-label usage [1]. One potential application of rhBMP-2 is in the surgical management of midshaft humeral fractures [2]. Humeral fractures are relatively common and account for 1% to 5% of all fractures occurring in a bimodal distribution of age [4]. For the elderly population, these fractures typically occur after low-energy trauma such as a fall with an outstretched arm. Initial treatment usually involves splinting with a humeral cuff which yields appropriate alignment and union in 77.4–100% of patients [4]. In cases of non-union, surgical fixation might be the next step in the treatment plan involving open reduction internal fixation (ORIF) with compression plating or intramedullary nail [5]. Further, the usage of rhBMP-2 with surgical intervention can potentially achieve desirable union especially in patient populations that are elderly and have multiple comorbidities [2]. In this case report, we present a 64-year-old right-hand dominant female patient with multiple comorbidities, with a comminuted nonunion left midshaft humeral fracture that was initially treated with conservative management by using a humeral cuff. After persistent and significant pain and serial radiographs indicating poor healing with a non-union after 5 months of conservative management, the patient underwent an ORIF with a single pledget of rhBMP-2 (Infuse, Medtronic Sofamor Danek, Memphis, TN, USA) at the fracture site to promote osteogenesis.
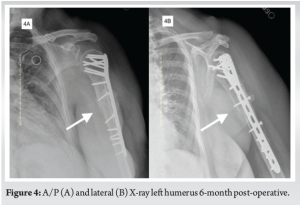
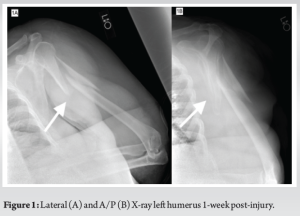
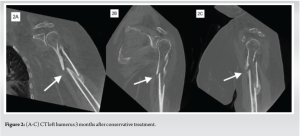
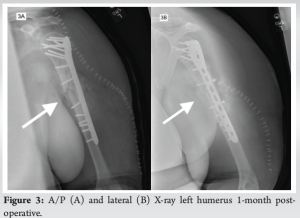
We present the case of a 64-year-old right hand dominant female with a comminuted nonunion left midshaft humeral fracture. Comorbidities include diabetes mellitus type II, morbid obesity (BMI 44.6), chronic obstructive lung disease, hypertensive disorder, hyperlipidemia, gastroesophageal reflux disease, and peripheral neuropathy. The patient suffered from chronic back pain, requiring a cane, when she fell onto her outstretched left arm while attempting to ascend stairs. X-ray imaging showed a displaced–comminuted fracture of the proximal humerus shaft with an associated butterfly fracture fragment (Fig. 1a and b). The patient opted for conservative management with a humeral cuff and physical therapy. This continued for 4 months with exacerbation of her symptoms and onset of associated shoulder pain. CT revealed a poor healing humeral fracture with a partial union (Fig. 2a-c) and an MRI of the shoulder showed acromioclavicular joint osteoarthrosis. After persistent and significant pain and serial radiographs indicating poor healing, the patient underwent an ORIF with an infusion of rhBMP-2 at the fracture site to promote osteogenesis. With consideration to patient blood sugar parameters, the patient HbA1c was recorded at 10.2 around time of initial injury when conservative management was initiated and an HbA1c of 14.3 was obtained 5 months after surgery. Due to the elevated BMI of the patient, the patient had a foley catheter placed in anticipation of a longer operation. She was also dosed with prophylactic intravenous antibiotics. The patient underwent an interscalene block followed by general endotracheal anesthesia and was positioned on a Berchtold shoulder table where she was properly secured. The patient’s left arm, elbow, shoulder, and upper neck area were cleaned and definitively prepped and draped. After a timeout, a sigmoid incision was made about the anterior and lateral aspect of the shoulder and arm, starting superiorly with a deltopectoral incision, extending laterally to produce a soft sigmoid configuration to the incision. The distal portion of the deltoid was elevated off the lateral aspect of the fracture. A subperiosteal dissection was achieved with the brachialis muscle and extended distally to the brachioradialis. The radial nerve was pressed on (posteriorly) by the large butterfly fragment and was liberated by a careful subperiosteal dissection. The dissection continued proximally to the subdeltoid and subacromial zone. After the dissection, it was noted that the patient had healing of the proximal portion of the butterfly fragment that healed into extension and was pressing on the passing radial nerve. There was proper dissection of the pseudoarthrosis utilizing sharp dissection, electrocautery, a high-speed burr, pituitary rongeurs, and standard Leksell rongeur. Proper reduction was obtained of the medial element of the fracture along the shaft. Provisional fixation consisted of a pin fixation. A synthes proximal humerus extended plate was then fitted to the lateral aspect of the humerus posterior to the bicipital groove. There was reduction of the two main elements of this fracture, namely, the shafts, exclusive of the butterfly fragment, followed by the placement of locking and non-locking screws. Once good fixation was attained, a high-speed burr was utilized to liberate the proximal portion of the butterfly fragment into forward flexion, allowing reduction of this fracture. This was fixated utilizing a cerclage of #1 PDS as well as two interfragmentary screws going from lateral to medial. The shafts associated with the humerus were cleaned of any fibrous tissue and packed with cancellous croutons. The osteotomy was then applied to the proximal butterfly fragment utilizing the high-speed burr, and then, the clamps were used to clamp this back down to the remainder of the bone utilizing simple single interfragmentary screws without compression, and then screwed into position. Once there was proper fixation and closure of the fracture, there was a window through the cortex in the proximal one third of the shaft that was filled at the fracture site with a single small Infuse pledget of BMP-2. This was followed by placement of more cancellous croutons into the cortical window. The pectoralis tendon, deltoid tendon, and portions of the brachialis were fixated down to the plate utilizing #2 FiberWire in the case of the two former and utilizing #1 Vicryl for the brachialis. The deltopectoral interval was closed with #1 Vicryl using simple interrupted stitches. The subcutaneous tissues were closed utilizing 0 Vicryl and 2-0 Vicryl and the skin itself was stapled. Sterile dressings were applied, and the patient was carefully disassembled from the Berchtold table, extubated, and transferred to the recovery room. She was hospitalized for 5 days before discharge where she was encouraged to supplement with Vitamin D3, Vitamin K2, and a multivitamin. Imaging 1 month after surgery displayed proper alignment with the intracortical window of application of BMP-2 (Fig. 3a and b). Six-month postoperatively, X-rays indicated appropriate fracture healing without hardware loosening and no significant complications were noted by the patient (Fig. 4a and b).
Non-operative treatment is the standard of care for humeral shaft fractures, with literature reporting 89% of proximal humerus fractures being treated conservatively [4, 6]. This treatment involves immobilization of the affected upper limb with a sling for 1 to 2 weeks before placement in a humeral cuff for 10–12 weeks (about 3 months) which provides stability to aid with alignment [4]. This is particularly the preferred option for patients with medical comorbidities that make them higher risk for surgical intervention [6]. Although conservative treatment is most common, it is not always viable [4]. Operative treatment is based on patient presentation and clinical judgment and may be indicated with numerous presentations including open fractures, polytrauma, or conservative treatment failure (non-union, malunion, and delayed union) [4]. Intramedullary nail fixation (IMN) and ORIF are the two most common repair methods, with ORIF often being preferred for lower rates of post-operative shoulder complications [6]. Zhao et al. assert that minimally invasive percutaneous osteosynthesis (MIPO), which provides fixation with minimal soft-tissue damage, provides lower incidence of iatrogenic radial nerve injury than ORIF and is thus a preferred method to ORIF and IMN [7]. However, there was no significant difference in non-union or delayed union rates among these three interventions and non-union must be addressed [7]. Non-union of humeral shaft fractures is uncommon [8]. An extensive meta-analysis by van de Wall et al. reported 15.3% non-union rate in conservatively treated patients and 6.4% in those treated operatively [8]. Although this difference is significant between populations, it does not stratify the data for patients with comorbidities. Numerous factors have been considered to impede bone healing (high age, smoking, and comorbidities), although strength of association varies between studies [9]. Oliver et al. reported increasing risk of non-union (OR 1.95, CI 95%, P = 0.014) in conservatively managed humeral shaft fractures with the presence of at least one comorbidity [9]. Listed comorbidities associated with non-union include hypertension, chronic kidney disease, glenohumeral arthritis, and obesity among others [9]. Thus, improving union rates with BMP-2 could provide value in decreasing reintervention rates and overall nonunion rates in patients at higher risk for nonunion. With a growing aging population in the US, we can anticipate an increase in cases of humeral shaft fractures [4]. Every surgical intervention poses a risk (risk of infection, migration of fracture, etc.); these risks increase with each surgical reintervention, which increases the importance of bony union with the first surgery [8]. The use of BMP-2 for fracture union appears promising, but studies with BMP-2 use for humeral shaft fractures are lacking. Mariscal et al. conducted a meta-analysis of BMP-2 use versus iliac crest bone graft (ICBG) for posterolateral fusion of the lumbar spine which indicated that BMP-2 had improved fusion rates and reduced surgical morbidity compared to ICBG [10]. This research provides light to BMP-2 use for other fractures and warrants further investigation. There are limitations to rhBMP-2 use for fracture non-union and side effect profile must be considered. Local inflammatory complications and ectopic bone formation are of concern given the osteoinductive properties of BMP-2. In a review of BMP-2 use as a bone graft substitute by James et al. [1], multiple clinical side effects have been reported (ectopic bone formation, inflammatory complications, osteoclast-activated bone resorption, and tumor formation); the most common adverse effect being ectopic bone formation. James et al. also reported rhBMP-2 application in spinal canal/foramen procedures produced ectopic bone formation and subsequent post-operative radiculitis at an incidence rate 11% higher than patients not receiving rhBMP-2 [1]. However, intraosseous rather than extraosseous application in our case appeared to avoid radial nerve encasement and injury as the patient remained neurologically intact. In a study by Fuchs et al. [2], they compared union rates of long bone fracture patients who used rhBMP-2 in surgical treatment with patients who did not. They found that patients with humeral fractures and used rhBMP-2 did not have significantly higher union rates (83%) compared to patients who did not use rhBMP-2 (50%, P = 0.26). This illuminates the imperfections of rhBMP-2 application in the surgical management of humeral shaft fractures; however, given our case of an elderly patient with multiple comorbidities, rhBMP-2 can potentially be used in humeral shaft fractures when conservative management fails.
Although BMP-2 has been FDA indicated for use in interbody spinal fusion surgery and open tibial shaft repairs, this case demonstrates that BMP-2 can also promote healing of humeral shaft fractures. Further studies are needed to investigate the efficacy of rhBMP-2 use in the setting of humeral shaft fracture non-union.
When conservative management of proximal humerus fractures fails, ORIF with BMP-2 infusion at the fracture site can be considered a viable option to promote bony union.
References
- 1.James AW, LaChaud G, Shen J, Asatrian G, Nguyen V, Zhang X, et al. A review of the clinical side effects of bone morphogenetic protein-2. Tissue Eng Part B Rev 2016;22:284-97. [Google Scholar]
- 2.Fuchs T, Stolberg-Stolberg J, Michel PA, Garcia P, Amler S, Wähnert D, et al. Effect of bone morphogenetic protein-2 in the treatment of long bone non-unions. J Clin Med 2021;10:4597. [Google Scholar]
- 3.Halloran D, Durbano HW, Nohe A. Bone morphogenetic protein-2 in development and bone homeostasis. J Dev Biol 2020;8:19. [Google Scholar]
- 4.Gallusser N, Barimani B, Vauclair F. Humeral shaft fractures. EFORT Open Rev 2021;6:24-34. [Google Scholar]
- 5.Miska M, Findeisen S, Tanner M, Biglari B, Studier-Fischer S, Gruetzner PA, et al. Treatment of nonunions in fractures of the humeral shaft according to the Diamond Concept. Bone Joint J 2016;98B:81-7. [Google Scholar]
- 6.Cadet ER, Yin B, Schulz B, Ahmad CS, Rosenwasser MP. Proximal humerus and humeral shaft nonunions. J Am Acad Orthop Surg 2013;21:538-47. [Google Scholar]
- 7.Zhao JG, Wang J, Meng XH, Zeng XT, Kan SL. Surgical interventions to treat humerus shaft fractures: A network meta-analysis of randomized controlled trials. PLoS One 2017;12:e0173634-e. [Google Scholar]
- 8.van de Wall BJ, Ochen Y, Beeres FJ, Babst R, Link BC, Heng M, et al. Conservative vs. operative treatment for humeral shaft fractures: A meta-analysis and systematic review of randomized clinical trials and observational studies. J Shoulder Elbow Surg 2020;29:1493-504. [Google Scholar]
- 9.Oliver WM, Searle HK, Ng ZH, Molyneux SG, White TO, Clement ND, et al. Factors associated with humeral shaft nonunion. J Shoulder Elbow Surg 2021;30:2283-95. [Google Scholar]
- 10.Mariscal G, Nuñez JH, Barrios C, Domenech-Fernández P. A meta-analysis of bone morphogenetic protein-2 versus iliac crest bone graft for the posterolateral fusion of the lumbar spine. J Bone Miner Metab 2020;38:54-62. [Google Scholar]