This case report links paralabral cysts to unique anatomic neurovascular pathology. It provides a clinical example of paralabral cyst pathology and highlights the anatomic correlation while interweaving concepts founded in clinical presentation, physical examination, imaging, treatment, and recovery.
Dr. Zachary Jodoin, Department of Orthopaedics, UT Health San Antonio, San Antonio, Texas - 78229, United States. E-mail: jodoin@uthscsa.edu
Introduction: The shoulder is one of the most intricate articulation complexes in the human body. Any insult to its equilibrium can cause joint instability, pain, and dysfunction. The complex bony projections of the scapula, lengthy nature of the nerves, and extensive mobility of the joint places nerves at risk for impingement; this can, especially, be seen when examining the axillary and suprascapular nerves. Another rare cause of nerve impingement is a paralabral cyst secondary to labral tearing. If a paralabral cyst expands into the limited space occupied by the nerves, this can result in neuropraxia, muscle wasting, and loss of function. This phenomenon presents an interesting anatomic and clinical correlation.
Case Report: A 41-year-old male with no past medical history presented with left shoulder pain for 3 months. Physical examination showed a great range of motion but diffusely decreased strength. Magnetic resonance imaging of the left shoulder demonstrated posterosuperior labral tearing with an associated paralabral cyst extending into the spinoglenoid notch. An additional anteroinferior labral tear with an associated paralabral cyst was also found. Extensive infraspinatus and teres minor muscle atrophy suggesting active denervation was present. The patient failed conservative management and underwent arthroscopic labral repair with posterosuperior and anteroinferior paralabral cysts excision. The patient had an unremarkable recovery and by 1 year had full motion and 5/5 strength in all planes.
Conclusion: While paralabral cysts are well documented, there have been limited reports of cysts causing neural impingement of the axillary or the distal suprascapular nerve, let alone both occurring within the same individual. This case provides an interesting clinical scenario which very clearly depicts the neural innervation of the shoulder and pathologies that can impact function. This cystic impingement is a very interesting and rare finding that provides tremendous insight into both shoulder pathology and anatomy. This case is also useful to predict patient recovery after long-term nerve impingement and muscle denervation. This patient presented with significant loss of strength, motion, and shoulder dysfunction, but after surgical intervention, he regained complete motion and strength. This information can be used to help educate and guide patients in practice.
Keywords: Arthroscopy, paralabral cyst, superior labral anterior to posterior tear, bankart tear, sports medicine, denervation, atrophy, orthopedics.
The shoulder girdle is one of the most intricate articulation complexes in the human body. Seventeen muscles, innervated by nine nerves, cross and attach to the scapula to grant the joint unparalleled range of motion (ROM). A balance is struck between mobility and stability by both dynamic and static forces [1]. Any insult to this equilibrium can tip the scales toward joint instability, pain, and dysfunction. The lifetime prevalence of shoulder pain is almost 70% [2]. Numerous common etiologies exist for this pain including arthritis, rotator cuff pathology, and trauma. Although less common, another cause of shoulder dysfunction includes compression of the neurovascular structures that serve the joint [3-10]. The complex bony projections of the scapula, the lengthy nature of the nerves, and extensive mobility of the joint places nerves at risk for impingement; this can especially be seen when examining the axillary and suprascapular nerves [1,3-10]. Another cause of nerve impingement, which mimics baker popliteal cyst compression of the posterior tibial nerve, is a paralabral cyst [11]. These cysts can extend from the joint secondary to labral tearing [1]. If a paralabral cyst expands into the limited space occupied by the nerves, such as inferiorly at the quadrilateral space or superiorly in the spinoglenoid fossa, this can result in neuropraxia, muscle wasting, and debilitating loss of shoulder function [4-10]. This phenomenon presents an interesting anatomic clinical correlation between shoulder innervation and muscular function. Case reports of individual axillary or suprascapular nerve compression have been rarely presented in the literature, but, to the best of our knowledge, dysfunction of both nerves in a single patient has not been seen [4-10]. We present a case of axillary and suprascapular nerve compression by separate paralabral cysts secondary to both a superior labral tear from anterior to posterior (superior labral anterior to posterior tear) and an anterior inferior Bankart labrum tear (Fig. 1). This patient presented with significant loss of strength, ROM, and shoulder dysfunction, but after arthroscopic cyst excision and labral repair, he regained complete restoration of ROM and strength.
Initial presentation
A 41-year-old male patient with no significant past medical history presented to the clinic with a chief complaint of left shoulder pain. His pain progressed gradually over the 3 months and was most notable when lifting weights. His pain was located primarily in the anterior and lateral aspect of the left shoulder. The pain was constant and achy in nature and intermittently sharp with activity. On physical examination, no visible deformity of the left upper extremity was observed. Passive ROM of the left shoulder was full and equal when compared to the right with forward elevation to 180°, abduction to 160°, and internal/external rotation to 95/75°. No provocative tests were positive on the initial physical examination. Strength was diffusely diminished in the left shoulder. Notably, 4/5 strength was observed with forward elevation, internal rotation, and abduction, and 3/5 strength with external rotation. The patient was neurovascularly intact distally. Sensation was full and intact to the left upper extremity. Cervical spine examination showed full ROM without provocation of his pain.
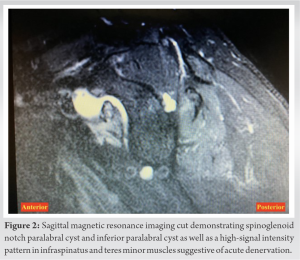
Four-view X-rays of the left shoulder demonstrated no evidence of acute fractures, arthritis, subluxation, or dislocation. The patient has already attempted a trial of home exercise and anti-inflammatories. Because of this, an magnetic resonance imaging (MRI) with arthrogram of the left shoulder was obtained to further delineate the cause of his pain. MRI of the left shoulder demonstrated both a superior and posterosuperior labral tearing with an associated 1.8 cm para-labral cyst extending into the spinoglenoid notch (Fig. 2). An additional anteroinferior labral tear with an associated 1.3 cm paralabral cyst was also found (Fig. 3). It also demonstrated infraspinatus and teres minor muscle atrophy suggesting active denervation of these muscles.
The patient was offered the option of non-operative care with continued anti-inflammatory medication and physical therapy or proceeding with a left shoulder arthroscopy with labral repair and cyst removal. After a discussion of the pros, cons, and alternatives, including continued muscle atrophy with non-operative management, the patient chose to proceed with the surgery.
Op report
Two weeks after his MRI follow-up, the patient returned for surgery. Before the surgery, the patient was given interscalene anesthetic with good effect.
The patient was positioned with a beanbag and axillary roll in the lateral position. The arm and shoulder were prepped and draped in sterile fashion. The arm was placed in a shoulder traction and rotation device with 10 pounds of traction. The shoulder was abducted to 10°. A standard posterior arthroscopy portal was established for arthroscope placement and then a second anterior portal was established in standard position through the rotator interval. Upon entry into the shoulder joint findings were significant for mild glenohumeral chondromalacia which did not require treatment. The posterosuperior labral tear extending from the 1:30 o’clock to 2:30 o’clock position and the associated para-labral cyst was visualized. The cyst was removed with a motorized shaver through the tear. The labral tear and glenoid bone were then prepared for repair with standard technique. An Arthrex FiberTak suture anchor was placed at the 2 o’clock position with good glenoid fixation, and sutures were passed in a simple suture fashion and tied with standard arthroscopic knots.
After repair of the posterosuperior labrum, the anteroinferior tear was then visualized. This tear was from the 5:30 o’clock position to the 7:30 o’clock position and had an associated para-labral cyst. The cyst was debrided with a motorized shaver through the tear and then the glenoid bone and labral tear were prepared for repair with standard technique. Two Arthrex FiberTak suture anchors were placed into the glenoid with good fixation at the 6 and 7 o’clock positions. Sutures were passed in a simple suture fashion and tied with standard arthroscopic knots. Following repair, no other internal derangements were visualized within the shoulder joint. The arthroscope and instruments were removed. The arthroscopy fluid was drained. Portals were closed with suture and steri-strips, and a sterile dressing was applied. The patient was transferred to recovery in stable condition. The patient was instructed to wear sling post-operatively for immobilization.
Post-operative follow-up
The patient presented 10 days postoperatively in his sling. His incisions appeared clean, dry, and intact without surround erythema. He had mild pain with gentle passive ROM and was neurovascularly intact distally. The patient was instructed to begin physical therapy out of his sling at this time.
The patient returned 6 weeks postoperatively for follow-up. He had been wearing his sling up until this visit. He also had been attending physical therapy 3 times weekly. Physical examination demonstrated healed incisions and a full passive ROM of the left shoulder. No sensory deficits were observed in the left shoulder. The patient was instructed to continue physical therapy and discontinue use of the sling at this time.
The patient returned for his third post-operative visit 2.5 months out from surgery. He subjectively reported full ROM and strength at about 60% of his normal strength. He was still attending physical therapy twice weekly. On physical examination, the patient had normal left upper extremity sensation when compared to the contralateral side. Passive external and internal rotation was noted to be limited at 45° and 45°, respectively, when compared to the right side which showed passive external and internal rotation to 75 and 95°, respectively. The patient was encouraged at this time to continue with physical therapy and to gradually increase strength.
At 4 months postoperatively, the patient returned for follow-up. He had been discharged from physical therapy and had resumed his regular gym exercise. Examination of the left shoulder at this visit demonstrated near full ROM and improving strength with only mild external rotation weakness noted.
The patient returned for follow-up at 6 months and stated he had a full ROM and good strength. On physical examination, the patient was noted to have full ROM in all planes and strength testing demonstrated 5/5 strength with abduction, forward elevation, internal rotation, and external rotation. The patient was instructed to resume all activities as tolerated and to return in 6 months for a final follow-up.
The final follow-up was at 1 year based on both patient preference, as well as substantially improved clinical presentation. The patient stated that he only experienced mild pain. He subjectively reported full ROM and an estimated 80% of full strength. Physical examination showed full ROM in all planes as well as 5/5 strength with external rotation, internal rotation, forward flexion, and abduction. The patient was assessed using the Oxford Shoulder Scoring system at 1-year post-operative with a score of 47/48. The patient stated that he was very happy with his results, and he was encouraged to follow-up as needed.
Suprascapular nerve compression
The anatomic course of the suprascapular nerve projects through multiple areas of limited space including the supraspinatus fossa, where it innervates the supraspinatus muscle, and the spinoglenoid notch, where it supplies the infraspinatus muscle [12]. Nerve entrapment in the suprascapular notch can therefore lead to denervation of both the supraspinatus and infraspinatus muscles, whereas nerve entrapment within the spinoglenoid notch will show sparing of the supraspinatus muscle but functional deficit of the infraspinatus muscle. The extension of this patient’s superior cyst into the spinoglenoid notch clearly led to a clinical picture consistent with a distal suprascapular nerve compression with infraspinatus denervation leading to atrophy and weakness in external rotation with sparing of the supraspinatus.
Axillary nerve compression
The axillary nerve also has an extensive course as it branches from the brachial plexus. The inferior cyst was recognized on MRI accompanied by extensive teres minor atrophy suggesting compression of the axillary nerve motor branch supplying it. This suspicion was confirmed intraoperatively when a second cyst protruding from the inferior tear into the quadrangular space was identified. The axillary nerve courses through this space and gives off three branches to supply deltoid motor function, teres minor motor function, and sensation over the lateral aspect of the shoulder [13]. Based on the MRI teres minor atrophy, weakness in external rotation, spared sensation over the lateral shoulder, and recovery of strength postoperatively, this inferior cyst was likely compressing the motor branch of the teres minor.
Paralabral cyst management latest advances
A recent study by Schroder analyzed 47 patients with labral tearing and isolated suprascapular nerve impingement. They found that within 2–3 months, pain was significantly less, muscle pathology, including edema, atrophy, and weakness, and bony erosion can be completely reversed with decompression and labral repair [14] Two additional studies found similar findings with paralabral cyst compression within the spinoglenoid notch and at the inferior labrum [15, 16]. As arthroscopic intervention and implant variety increase, these studies show that labral repair and cyst excision become attractive options for both successful and definitive management.
While paralabral cysts are well documented, there have been limited reports of cysts causing neural impingement of the axillary or the distal suprascapular nerve, let alone both occurring within the same individual. This case provides an interesting clinical scenario which very clearly depicts the neural innervation of the shoulder and pathologies that can impact its function. It is also an educational example of shoulder anatomy depicting lesions that can occur surrounding the joint. These lesions can lead to well-defined patterns of neuropraxia and muscular denervation, and therefore muscle weakness and wasting. The cystic impingement is consistent with anatomical studies performed and is a very interesting and rare finding that provides tremendous insight into both shoulder pathology and anatomy. This case is also useful to predict patient recovery after long-term nerve impingement and muscle denervation. This patient presented with significant loss of strength, ROM, and shoulder dysfunction, but after arthroscopic cyst excision and labral repair, he regained complete restoration of ROM and objective strength. This information can be used to help educate and guide patients in future practice.
This case report provides an educational and intriguing insight into the anatomical innervation of the shoulder musculature with correlation to unique paralabral pathophysiology. This case provides students and residents with a real-life example of clinical pathology with applied anatomy, while also giving providers and patients realistic expectations on the recovery process.
References
- 1.Dash S, Bheemreddy SR, Tiku ML. Posterior tibial neuropathy from ruptured Baker’s cyst. Semin Arthritis Rheum 1998;27:272-6. [Google Scholar]
- 2.Moore KL, Clinically Oriented Anatomy. 8th ed. Philadelphia, PA: LWW; 2017. [Google Scholar]
- 3.Gupta R, Kapoor L, Shagotar S. Arthroscopic decompression of paralabral cyst around suprascapular notch causing suprascapular neuropathy. J Clin Orthop Trauma 2015;6:184-6. [Google Scholar]
- 4.Hangge PT, Breen I, Albadawi H, Knuttinen MG, Naidu SG, Oklu R. Quadrilateral space syndrome: Diagnosis and clinical management. J Clin Med 2018;7:86. [Google Scholar]
- 5.Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol 2004;33:73-81. [Google Scholar]
- 6.Moore KL, Dalley AF 2nd, Agur AM. Clinically Oriented Anatomy. 8th ed, 3, Electronic Edition. PA: LWW; 2017. [Google Scholar]
- 7.Klumpp R, Gallinari G, Compagnoni R, Trevisan C. Antero-inferior paralabral cyst of the shoulder: An atypical cause of rapidly evolving axillary and musculocutaneous nerve palsy. J Clin Orthop Trauma 2020;11:S681-3. [Google Scholar]
- 8.Kokkalis ZT, Pantzaris N, Iliopoulos ID, Megaloikonomos PD, Mavrogenis AF, Panagiotopoulos E. Nerve Injuries around the Shoulder. J Long Term Eff Med Implants 2017;27:13-20. [Google Scholar]
- 9.Momaya AM, Kwapisz A, Choate WS, Kissenberth MJ, Tolan SJ, Lonergan KT, et al. Clinical outcomes of suprascapular nerve decompression: A systematic review. J Shoulder Elbow Surg 2018;27:172-80. [Google Scholar]
- 10.Drake RL, Vogl W, Adam WM, Mitchell MB. Gray’s Anatomy for Students. Netherlands: Elsevier Inc.; 2019 p. 671-821.e4. [Google Scholar]
- 11.Robinson P, White LM, Lax M, Salonen D, Bell RS. Quadrilateral space syndrome caused by glenoid labral cyst. AJR Am J Roentgenol 2000;175:1103-5. [Google Scholar]
- 12.Sanders TG, Tirman PF. Paralabral cyst: An unusual cause of quadrilateral space syndrome. Arthroscopy 1999;15:632-7. [Google Scholar]
- 13.Voloshin I, Schippert DW, Kakar S, Kaye EK, Morrey BF. Complications of total elbow replacement: A systematic review. J Shoulder Elbow Surg 2011;20:158-68. [Google Scholar]
- 14.Schrøder CP, Lundgreen K, Kvakestad R. Paralabral cysts of the shoulder treated with isolated labral repair: Effect on pain and radiologic findings. J Shoulder Elbow Surg 2018;27:1283-9. [Google Scholar]
- 15.Schroder CP, Skare O, Stiris M, Gjengedal E, Uppheim G, Brox JI. Treatment of labral tears with associated spinoglenoid cysts without cyst decompression. J Bone Joint Surg Am 2008;90:523-30. [Google Scholar]
- 16.Jeong JJ, Panchal K, Park SE, Kim YY, Lee JM, Lee JK, et al. Outcome after arthroscopic decompression of inferior labral cysts combined with labral repair. Arthroscopy 2015;31:1060-8. [Google Scholar]