Resistant and refractory non union of distal tibia fractures can be managed effectively with a free fibular graft used as a biological intramedullary nail
Dr. S Aravind, Department of Orthopaedics, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai, Tamil Nadu, India. E-mail: aravinds918@gmail.com
Introduction: Resistant and refractory non-union of distal tibia extra-articular fractures is very common even following internal fixation due to poor blood supply to the distal tibia metaphyseal region. The management can be challenging.
Case Report: A 50-year-old diabetic male had sustained closed distal tibia extra-articular fracture at the junction of diaphysis and metaphysis. Intramedullary interlocking nailing was done elsewhere. The fracture did not unite. Nail removal, bone grafting, and plate fixation were done elsewhere. The fracture did not unite and implant failure occurred. The nonunion was successfully managed by plate removal, intramedullary free fibula bone grafting, and Ilizarov fixation. Union required 6 months but patient finally was able to return to his work with good function and without any signs of infection.
Conclusion: This case illustrates the successful incorporation of a stabilized intramedullary fibula graft which enabled union of a resistant distal tibia fracture nonunion.
Keywords: Resistant tibia non-union, avascular fibular strut graft, distal tibia non union, ilizarov fixation
Fractures of tibia are relatively common with incidence of about 16.9/100,000/year [1]. Distal tibia fractures tend to heal slowly due to poor blood supply to the distal metaphyseal region and its longer subcutaneous border [2]. Delayed union is defined as the absence of radiographic healing 3–5 months following the injury in tibia diaphyseal fractures. For fractures that had not healed after 9 months, non-union was described [3]. Tibial non-union can be treated with revision nailing with a larger nail or with plating along with bone grafting. A subset of the patients who fail to unite will develop hypertrophic non-unions, which are due to excessive motion at the fracture site, preventing full mineralization of the fibrocartilaginous callus [4-6]. After repeated implant failures, non-unions are resistant to treatment [7]. Resistant non-union – cases which have been treated at least twice to achieve union – pose a challenge to the treating surgeon and the patient [8-12]. These are refractory to repeated treatment. In this case report, we discuss the case of a resistant non-union of distal tibia treated with a simple technique of intramedullary fibular graft along with an Ilizarov fixation. Patient was able to achieve union in a period of 6 months and is mobilizing well without external support.
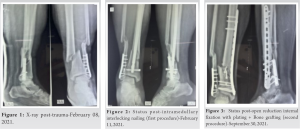
A 50-year-old diabetic obese male sustained a closed distal one third shaft of tibia and fibula fracture (Fig. 1). Patient was managed with closed reduction and intramedullary interlocking nailing elsewhere (Fig. 2).
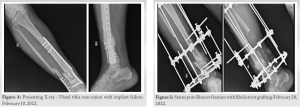
Seven months after nailing patient had no signs of union. The cause of the non-union seems to be improper reduction of the fracture and unstable fixation as there is deformity at the fracture site. He underwent nail removal, plate fixation along with bone grafting for the same elsewhere (Fig. 3). Three months after plating and bone grafting, patient presented to us with difficulty in weight bearing and pain over right leg. Fortunately he did not have any signs of infection. Patient had a history of right distal fibula plate fixation 19 years back. Presenting X-ray of right leg showed implant failure which is the cause of non-union of tibia in the second procedure and a malunited fibula fracture (Fig. 4).
Initially implant exit for tibia and fibula was done. Free fibula graft of length 10 cm was removed from middle third of fibula, with the distal 8–9 cm of the fibula being left in place for ankle stability. But unfortunately, the full thickness fibula graft was found to be thicker than the medullary canal and could not be inserted into the canal as an intramedullary graft. Graft was split longitudinally into two halves and was inserted into the fracture gap and the medullary canal of proximal and distal fragments. Cancellous bone grafting from iliac crest was packed around the fibula graft. The wound was partially closed. The fracture was stabilized using an Ilizarov fixation (Fig. 5). Ilizarov fixation was chosen since the distal fragment was small and did not have enough bone stock for screws fixation due to the previous plate fixation. Patient had a procurvatum deformity at the fracture site with Anterior Distal Tibial Angle of 93.3 degrees which was not corrected as it was acceptable.
Due to the deformity, arc of motion of the ankle changed which resulted in decreased dorsiflexion and increased plantar flexion at the ankle joint. Patient had dorsiflexion of 10° and plantar flexion of 30°. It did not cause any significant difficulty in gait. Malalignment in the sagittal plane is better tolerated and is of less significance than similar degrees of malalignment in the frontal plane as it is compensated by the hip, knee, ankle, subtalar, and foot joints [13]. The posterior proximal tibial angle was 100.2° (Normal-81 ± 3) and the anterior distal tibial angle was 93.3° (Normal-80 ± 2) (Fig. 6-10).
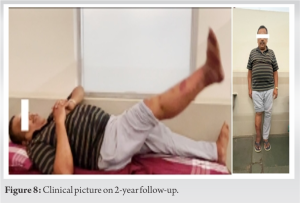
Patient was allowed partial weight bearing mobilization with support following the surgery. Radiographs were taken at 6 weeks, 3 months and 6 months to assess healing of the fracture. After 6 months, Ilizarov fixator was removed and patient was put on patella tendon bearing (PTB) cast. After 45 days, the PTB cast was removed and the patient was mobilized. Patient is mobilizing well and does not have pain or any signs of infection. Patient has returned back to his work with a follow-up of 2 years (Fig. 6 and 7).
Resistant and refractory non-union of distal tibia after multiple procedures is a challenge to be treated as the bone refuses to unite. The bone also becomes osteoporotic making it more difficult to treat. In our case, patient had additional risk factors for non-union like obesity and diabetes. Options of treatment included revision internal fixation and bone grafting. But in view of the void, a large volume of bone graft would berequired. We also did not have access to bone bank and allograft. The next option would have been Ilizarov fixation, proximal tibial corticotomy and bone transport to manage the gap. However, this entails a long period of ring fixation till the regenerate consolidates. Usually, additional bone grafting would have also been required at the docking site. The fibular strut graft acts as a biological intramedullary nail providing mechanical support and also being osteoconductive at the same time, helping also to fill the bone void. In our case, patient had a small distal fragment with multiple voids due to screws from multiple procedures making us resort to Ilizarov fixation. Fibular grafting along with plating can also be done if the bone has sufficient screw purchase. In that case, incorporating an intramedullary fibular graft also helps in increasing the screw purchase. A difficulty we faced in our case – the fibular strut graft was larger in diameter than the medullary canal and we had to divide the fibular graft longitudinally to insert the graft into the medullary canal. Proper preoperative planning, involving assessment of the medullary canal, diameter of the fibula, length of the fibular graft required can be useful in avoiding difficulties intraoperatively. A narrow medullary canal might require reaming in order to accommodate the fibular strut graft. Whereas in a wide medullary canal graft, it can be placed without reaming. Kirshcner wire can also be passed into the graft to strengthen the graft [10]. Additionally cancellous bone grafting can be done for its osteoinductive properties which can augment healing and union. In our patient, 6-month postoperatively, the fracture achieved union. Nine-month postoperatively, patient was able to mobilize without any external support with good function making him return to his day-to-day activities with a visual analog score of 0/10. Patient does not have any pain or infection and is mobilizing well with a follow-up of 2 years. The fibular strut is to be inserted immediately after removal from the donor site to encourage the retention of viable properties [8]. It has been reported that if the autologous bone graft is fixed to the recipient bone immediately after it is retrieved, the osteogenic cells on and in the graft survive [10, 11]. The long bone diaphyseal non-union after intramedullary nailing occurs usually due to instability [6]. Yadav et al. stated that the free fibular graft acts as a biological nail and when the medullary canal is reamed to appropriate size of the fibular graft, three borders of the fibula fix firmly to the inner cortices of the fractured fragments and sufficiently reduce the undesirable movements that are observed with non-locking intramedullary nail. Larger the contact area between the graft and the host bone, better is the union [10]. Hence, the size of the fibular graft needed is to be planned preoperatively for better outcomes.
Fibular strut grafting is a simple and effective way to treat refractory non-union of tibia refusing to unite even after multiple procedures. It is a bone in bone fixation and is more biological which helps in healing even resistant non-union of long bone fractures.
This case report explains a simple and effective way of successfully treating resistant non-union of distal tibia fracture with a free fibular graft. This method can also be used in treating refractory non-union of any long bone.
References
- 1.Larsen P, Elsoe R, Hansen SH, Graven-Nielsen T, Laessoe U, Rasmussen S. Incidence and epidemiology of tibial shaft fractures. Injury 2015;46:746-50. [Google Scholar]
- 2.McMillan TE, Johnstone AJ. Technical considerations to avoid delayed and non-union. Injury 2017;48:S64-8. [Google Scholar]
- 3.Wiss DA, Stetson WB. Tibial nonunion: Treatment alternatives. J Am Acad Orthop Surg 1996;4:249-57. [Google Scholar]
- 4.Aronson J, Harrison BH, Boyd CM, Cannon DJ, Lubansky HJ, Stewart C. Mechanical induction of osteogenesis: Preliminary studies. Ann Clin Lab Sci 1998;18:195-203. [Google Scholar]
- 5.Brinker MR, O’Connor DP. Nonunions: Evaluation and treatment. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, Krettek C, editors. Skeletal Trauma. 4th ed. Philadelphia, PA: Saunders Elsevier; 2009. [Google Scholar]
- 6.Hak DJ. Management of aseptic tibial nonunion. J Am Acad Orthop Surg 2011;19:563-73. [Google Scholar]
- 7.Li XK, Wang HQ, Wei YY, Wu ZX. Treatment of nonunions of humeral fractures with interlocking intramedullary nailing. Chin J Traumatol 2008;11:335-40. [Google Scholar]
- 8.Cannada LK. Viable bone and circulatory factors required for survival of bone grafts. Orthop Clin North Am 2010;41:5-13. [Google Scholar]
- 9.Garnavos C. Treatment of aseptic non-union after intramedullary nailing without removal of the nail. Injury 2017;48 Suppl 1:S76-81. [Google Scholar]
- 10.Yadav SS. The Use of a free fibular strut as a “Biological intramedullary nail” for the treatment of complex nonunion of long bones. JB JS Open Access 2018;3:e0050. [Google Scholar]
- 11.Livani B, Belangero W, Medina G, Pimenta C, Zogaib R, Mongon M. Anterior plating as a surgical alternative in the treatment of humeral shaft non-union. Int Orthop 2010;34:1025-31. [Google Scholar]
- 12.Kanakeshwar RB, Jayaramaraju D, Agraharam D, Rajasekaran S. Management of resistant distal femur non-unions with allograft strut and autografts combined with osteosynthesis in a series of 22 patients. Injury 2017;48 Suppl 2:S14-7. [Google Scholar]
- 13.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994;25:425-65. [Google Scholar]