Coccyx has different mobility patterns, mobile, immobile, and hypermobile. Coccydynia is intractable pain in the coccygeal region. It is usually treated conservatively. Chronic refractory coccydynia is treated with ganglion impar block. GIB has been administered for patients with both mobile and immobile coccyges and the patient had similar outcomes in terms of pain reduction
Dr. A Ganesh, Department of Orthopaedics, Chettinad Hospital and Research Education, Chettinad Academy of Research and Education, Kelambakkam, Chengalpattu, Tamil Nadu, India. E-mail: aganesh.anantharaman6@gmail.com
Introduction: Patients with persistent coccygodynia who do not respond to conventional therapies may undergo ganglion impar block (GIB). We looked at how GIB therapy for individuals with persistent coccygodynia affected their coccygeal dynamic patterns.
Materials and Methods: Patients with persistent coccydynia with GIB once using a trans-Sacro-coccygeal technique with fluoroscopy supervision were taken up for the study. Out of 14 patients, they were categorized as Group I- mobile coccyx (8 patients) and Group 2- immobile coccyx (6 patients) using static and dynamic coccyx radiographs, based on coccygeal mobility. A visual analog score (VAS) was used to measure pain levels both before and after the intervention (at 1 hour and 2, 4 weeks). A VAS score drop of 50% or more was considered to be a meaningful reduction in pain.
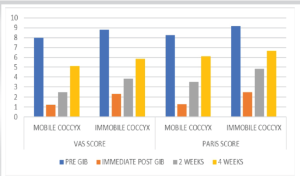
Discussion: On every subsequent visit, the VAS scores were considerably lower in both groups, the pre- and post-intervention VAS scores significantly differed between the two groups. In follow-up, there was no significant difference in the scores between the two groups.
Conclusion: Normal and immobile coccyges detected by standard and dynamic radiographs of patients with chronic coccydynia appear to be two different coccygeal dynamic patterns that do not affect the treatment outcome in Ganglion Impar Block
Keywords: Coccyx, back pain, tailbone, ganglion impar block, coccygeal mobility.
The midline confluence of the caudal ends of two paravertebral sympathetic chains forms the ganglion impar, often referred to as Walther’s ganglion, which is a sympathetic ganglion. It can be found in various forms and sizes on the ventral surface of the coccyx. The anal and perineal regions receive sympathetic innervation in addition to somatic innervation from the ganglion. It furthermore supplies the internal sympathetic innervation [1]. The anatomical variability of the ganglion’s location determines the method’s success rate, although reports of its location range from the anterior to the sacrococcygeal joint or the coccyx to the tip of the coccyx [2]. Intractable pain in the coccygeal area is the hallmark of chronic coccygodynia, also known as coccydynia, an illness that is challenging to identify and manage. Recent studies have indicated that pelvic discomfort, including pain from malignant neoplasms, and persistent, refractory coccygodynia may benefit from ganglion impar block (GIB). This approach has several benefits, including the ability to be used on patients of all ages, from adolescents to the elderly, the ability to enhance quality of life, the ability to provide repeat injections to patients experiencing only partial pain relief, and the potential to produce more positive effects. Unfortunately, between 18% and 25% of individuals receiving GIB treatment does not have a satisfactory improvement in their symptoms. In individuals with coccydynia, certain coccygeal dynamic patterns might not have an impact on GIB therapy efficacy alone. The research does not, however, include sufficient information about the elements that influence therapy success. Therefore, the purpose of this study was to examine the impact of individual characteristics and coccygeal dynamic patterns on the course of treatment for patients with chronic coccydynia treated with GIB through the Trans-sacrococcygeal technique who did not respond to conservative measures.
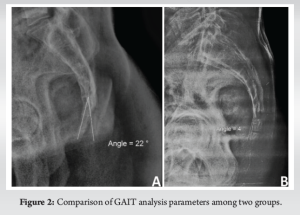
The prospective observational study was carried out in a tertiary care hospital in southern Indian state. Fourteen patients who fulfilled the inclusion and exclusion criteria were taken up for study. Patients aged more than 18 years of age with chronic refractory coccygeal pain which was non-responsive to conservative measures and oral medication for at least 3 months were taken up for study. Patients having coccydynia linked to metastasis or coccygeal fracture, a history of lumbar or coccygeal surgery, people who had undergone recurrent GIB, and missing follow-up appointments were excluded from the study. Lateral coccygeal X-ray was done for all the patients both in sitting and standing position and angle between the tips of the coccygeal segments were measured. Patients were divided based on the angle into two groups. Group 1 included patients having mobile coccyx and Group 2 had patients with immobile coccyx. They were classified using static and dynamic coccyx radiographs, based on coccygeal mobility.
Imaging technique :
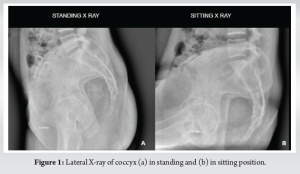
Firstly, for each patient, standard lateral coccygeal radiographs were taken after standing for 10 min, according to Maigne’s lateral dynamic X-ray protocol [1]. Then, the digital dynamic lateral coccygeal graphs were taken to evaluate the coccygeal mobility at the sitting position (painful position) with the vertebrae in extension and hips in flexion (Fig. 1). The angle between the tips of the coccygeal segments formed on radiographs by sagittal movement of the coccyx when the patient was sitting in the painful position (the angle of mobility) was noted (Fig. 2). The patients were categorized as normal (mobility between 5 and 25), immobile (with and without spicule, mobility between 0 and <5), or hypermobile (mobility of more than 25) based on the coccygeal mobility.
Procedure:
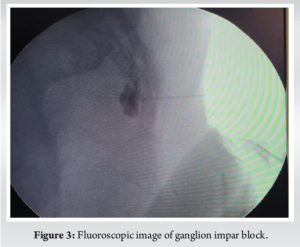
The procedure has been performed under fluoroscopic guidance. With the patient prone, the intergluteal area was sterilized and a small amount of local anesthetic (3 mL of 2% xylocaine) was given at achieving blockade of cutaneous and subcutaneous tissues. The sacrococcygeal joint was visualized through a fluoroscopy. A 22-gauge spinal needle was used to reach the ganglion impar by passing through the sacrococcygeal joint. After a 1 mL injection of non-ionic contrast and spreading of the dye gave a ‘‘reverse comma’’ appearance in the lateral view (Fig. 3), 3 mL of 0.5% bupivacaine, 2 mL of saline, and 1 mL (40 mg) of triamcinolone acetate were injected.
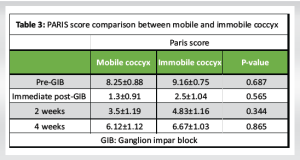
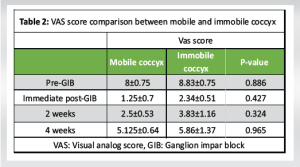
A total of 14 patients who underwent GIB were taken as the subjects for this study. According to Maigne’s lateral dynamic X-ray protocol, patients were classified into 2 groups (Group 1-Mobile coccyx and Group 2 – immobile coccyx). Group 1 included 8 patients (3 male and 5 female) and Group 2 included 6 patients (two males and four females). Mean age of the population in Groups 1 and 2 was 53.7 ± 10.21 and 49.67 ± 6.24, respectively. The visual analog score (VAS) and PARIS scores at 1 h following the procedure demonstrated a significant reduction in pain caused by the intervention (Table 1). Every evolution time point saw a significant drop in scores in both groups when compared to the pre-procedure PARIS and VAS (Fig. 4).
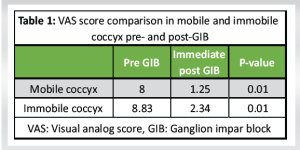
In contrast, there was no statistically significant difference between Group I and II at the immediate post-procedure, 2 weeks, and 4 weeks intervals (Tables 2 and 3). All patients only had one GIB procedure. After the procedure, none of the patients experienced any complications.
As coccydynia is a clinical condition with a variety of etiologies, there are currently no established diagnostic standards. Often, the source of the pain is not known. The frequency of coccydynia in females is 5 times higher than in males. Women may be more susceptible to this phenomenon due to their more posteriorly located sacrum and coccyx [3, 4]. Pain may also result from a sacrococcygeal ligament injury sustained during vaginal delivery. Because the coccyx is mobile and supported by the sacrococcygeal ligament, sprains rather than fractures are more common. Chronic sprain of the coccyx can also be brought on by microtraumas from improper body positioning during sitting [5]. However, since idiopathic pain is frequently the source of the problem, a careful differential diagnosis is required. According to other sources, abrupt weight loss causes a loss of natural tissue protection and is a risk factor for coccygodynia [6]. A retroperitoneal structure at the level of the ganglion impar the sacrococcygeal junction, where the paravertebral sympathetic chain comes to an end. When other conservative treatments for coccydynia are ineffective, GIB is typically used as a treatment. It is possible to (1) perform a diagnostic GIB ganglion impar block using a local anesthetic to verify the block’s effectiveness. Both sympathetic and nociceptive fibers are blocked to relieve pain. Based on our patients’ results, the GIB ganglion impar block may be a useful therapeutic option for providing long-term relief from coccydynia [7]. The trans-Sacro-coccygeal “needle inside needle” approach used in this study is a technically workable, simple to learn, and superior to the classical and paramedian approaches to the ganglion. When compared to surgical treatment, this technique carries a minimal risk. With careful attention, the risks associated with this procedure can be minimized, including neuritis and accidental injection of the neurolytic agent into the rectum. Wemm and Saberski [8] originally described the method, and Nebab and Flonehce later made modifications. In our review, the normal and dynamic radiographs of 14 patients with persistent coccygodynia who were impervious to moderate treatment and who went through GIB under fluoroscopy were assessed for mobile and immobile coccyx. In like manner, the patients were arranged into regularly portable and stationary coccyx, and their VAS scores were looked at. Conceivable impacting variables such as age, sex, body mass index, length of sickness, and presence of injury had no impact on results. According to Maigne et al.’s study of 248 coccygodynia patients, 69.2% of the cases could have the lesion identified using the lateral dynamic radiography protocol. Gitkind AI, Mahmood S et al proposed a link between the cause of pain in coccydynia patients and subluxation, hypermobility, and immobility. When coccygeal instability results in coccygeal hypermobility and subluxation, the patient experiences pain when seated and chronic inflammation. When a patient sits, the presence of a spicule causes irritation and inflammation in the coccygeal region. It is highlighted that there is only a weak correlation between coccygeal pain and other lesions, such as immobility without a spicule and normal mobility. [9,10] In our study, a reduction in pain beginning at 1 hour and sustained for up to 2 months was provided by the GIB in both groups. Postacchini & Massobrio, Usta et al and Ahadi et al contrasted the lateral radiographs of asymptomatic patients with those of patients who had a partial or total coccygectomy and outlined four different coccygeal configuration types. They demonstrated that Type I, which is slightly forward-curving, was more common in asymptomatic people whereas patients with coccydynia were more likely to have other forms, such as subluxation. Nonetheless, they discovered no connection between the treatment results in patients undergoing partial or complete coccygectomy and the pre-operative coccygeal morphology. Likewise, there does not seem to be any clear correlation between the results of GIB therapy and a normal or immobile coccyx pattern. [11-13]. There are certain limitations on our research. Two additional coccygeal lesions-subluxation and hypermobility-that were found in patients with coccydynia prevented us from assessing their impact on the course of treatment. Because there were so few participants in our study, it is likely that we were unable to detect these two types of lesions in any of the subjects. The absence of an evaluation for sacrococcygeal or trans sacrococcygeal disc degeneration is additional limitations. However, since our study investigates the impact of coccyx radiological features on GIB treatment outcomes, it offers crucial data.
A safe and effective alternative therapeutic strategy to lower pain ratings with low complication rates is GIB given using the trans sacrococcygeal procedure to patients with chronic coccygodynia refractory to conservative therapy. Normal and immobile coccyges detected by standard and dynamic radiographs of patients with chronic coccydynia appear to be two different coccygeal dynamic patterns do not affect the treatment outcome in GIB Ganglion Impar Block.
Mobility of the coccyx is often overlooked in the treatment of chronic coccydynia. Its role has not been studied extensively. Although it has a very less role in pain management, it is evident that the mobility of coccyx does not affect the outcome in GIB. Hence, our study proves that GIB ganglion impar block is efficient but mobility does not play a significant role in pain reduction.
References
- 1.Sencan S, Cuce I, Karabiyik O, Demir FU, Ercalik T, Gunduz OH. The influence of coccygeal dynamic patterns on ganglion impar block treatment results in chronic coccygodynia. Interv Neuroradiol 2018;24:580-5. [Google Scholar]
- 2.Oh CS, Chung IH, Ji HJ, Yoon DM. Clinical implications of topographic anatomy on the ganglion impar. Anesthesiology 2004;101:249-50. [Google Scholar]
- 3.Toshniwal GR, Dureja GP, Prashanth SM. Transsacrococcygeal approach to ganglion impar block for management of chronic perineal pain: A prospective observational study. Pain Physician 2007;10:661-6. [Google Scholar]
- 4.Fogel GR, Cunningham PY 3rd, Esses SI. Coccygodynia: Evaluation and management. J Am Acad Orthop Surg 2004;12:49-54. [Google Scholar]
- 5.Ho KY. Ganglion impar injection techniques for coccydynia (coccyx pain) and pelvic pain. Anesthesiology 2007;106:1063. [Google Scholar]
- 6.Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner J 2014;14:84-7. [Google Scholar]
- 7.Gonnade N, Mehta N, Khera PS, Kumar D, Rajagopal R, Sharma PK. Ganglion impar block in patients with chronic coccydynia. Indian J Radiol Imaging 2017;27:324-8. [Google Scholar]
- 8.Wemm K Jr., Saberski L. Modified approach to block the ganglion impar (ganglion of walther). Reg Anesth 1995;20:544-5. [Google Scholar]
- 9.Gitkind AI, Olson TR, Downie SA. Vertebral artery anatomical variations as they relate to cervical transforaminal epidural steroid injections. Pain Med 2013;15:1109-14. [Google Scholar]
- 10.Mahmood S, Ebraheim N, Stirton J, Varatharajan A. Coccydynia: A literature review of its anatomy, etiology, presentation, diagnosis, and treatment. Int J Musculoskelet Disord 2018;1:1-5. [Google Scholar]
- 11.Usta B, Gozdemir M, Sert H, Muslu B, Demircioglu RI. Fluoroscopically guided ganglion impar block by pulsed radiofrequency for relieving coccydynia. J Pain Symptom Manage 2010;39:e1-2. [Google Scholar]
- 12.Sencan S, Edipoglu IS, Ulku Demir FG, Yolcu G, Gunduz OH. Are steroids required in the treatment of ganglion impar blockade in chronic coccydynia? A prospective double-blinded clinical trial. Korean J Pain 2019;32:301-6. [Google Scholar]
- 13.Ahadi T, Asilian M, Raissi GR, Soltani SK, Soleymanzadeh H, Sajadi S. Ultrasound-guided vs. Blind coccygeal corticosteroid injections for chronic coccydynia: A randomized, clinical trial. Arch Bone Jt Surg 2022;10:877-84. [Google Scholar]
- 14.Sencan S, Kenis-Coskun O, Demir FG, Cuce I, Ercalık T, Gunduz OH. Ganglion impar block improves neuropathic pain in coccygodynia: A preliminary report. Neurol Neurochir Pol 2018;52:612-7. [Google Scholar]