Comparative outcomes of anterior cruciate ligament reconstruction: Peroneus versus Hamstring graft.
Dr. Nilkumar Patel, Dhiraj Hospital, Smt BK Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India. E-mail:neelpatel0803@gmail.com
Introduction: Anterior cruciate ligament (ACL) injury is the most common for athletes. ACL injury reconstruction is a pivotal surgical intervention aimed at restoring knee stability and function following ligamentous trauma.
Surgical Techniques Advances in surgical techniques and rehabilitation protocols have significantly improved outcomes and patient recovery rates. This paper reviews current trends, outcomes, and future directions in ACL reconstruction using peroneus longus and hamstring grafts and emphasizing innovations in surgical approaches and rehabilitation strategies.
Conclusion: Peroneus longus grafts offer superior outcomes compared to hamstring grafts for ACL reconstruction. They provide enhanced graft strength and stability, potentially reducing the risk of re-injury. In addition, their use can lead to quicker recovery times and improved functional results for patients.
Keywords: Anterior cruciate ligament reconstruction, hamstring tendon autograft, peroneus longus tendon autograft.
Graft selection in anterior cruciate ligament (ACL) reconstruction is critical, as it remains one of the most easily adjustable factors affecting graft rupture and reoperation rates. Commonly used autografts, including hamstring tendon, quadriceps tendon. The primary goal of ACL-R is restoring anteroposterior and rotatory knee stability and function as closely as possible to the native joint. Despite advances in surgical techniques and rehabilitation, post-operative complications including graft rupture remain significant, yielding severe socioeconomic consequences and detrimental patient experience. The primary aim of ACL reconstruction is to restore the function of the ACL and native kinematics of the knee [1]. ACL reconstruction restores the stability of the knee joint and protects the menisci and joint surfaces from further damage and prevents progression of existing chondral lesions as well as occurrence of newer lesions. Reconstruction of the ACL may also alter the incidence of osteoarthritis in the longer term [2]. Recent literatures have focused on the concept of “anatomic” ACL reconstruction [3, 4] and popularized independent ACL femoral tunnel creation techniques like anteromedial portal (AMP), outside in, retrograde drilling, which results in more anatomically accurate ACL femoral tunnel placement[5, 6]. ACL reconstruction can be single bundle (SB)-anteromedial (AM) or double-bundle (DB) both AM and posterolateral reconstruction. DP ACL reconstruction is required only in patients with high athletic demands.[7] The purpose of this study is to evaluate clinical and functional outcomes of arthroscopic ACL reconstruction using hamstring and peroneus longus graft.
After getting clearance from the Institutional Ethics Committee, the study was carried out in patients who had ACL injury and underwent arthroscopic reconstruction of ACL after getting a prior informed consent. Patients who were diagnosed and admitted in the Department of Orthopedics, with ACL injury and underwent arthroscopic reconstruction of ACL were included in the study. The study duration was 30 ± 4.5 months. Ninety patients satisfying the inclusion criteria, operated from January 2019 to January 2023 were enrolled in this study. Patients were informed about the study in their vernacular language. All the patients were followed up for a minimum 12 months postoperatively.
Inclusion criteria
All patients between 18 and 60 years of age who had ACL tear and have undergone arthroscopic ACL reconstruction during the study period.
Exclusion criteria
Included those patients who had associated intra-articular/avulsion fractures of the tibial spine, open injuries of the knee, and patients not willing for surgery or not willing to participate in the study.
Patient’s injured knees were assessed under spinal anesthesia with standard Lachmann, anterior drawer, and pivot shift tests. High above knee pneumatic tourniquet was applied. Diagnostic arthroscopy was performed using the standard AM and anterolateral portals and the findings were noted. Meniscal injuries were assessed and treated accordingly. Semitendinosus gracilis peroneus longus grafts were harvested, prepared, doubled quadrupled, and sized.[8] (Fig. 1)
Hamstring tendon harvesting
In the hamstring group, a 3 cm oblique skin incision was made over the AM aspect of the proximal tibia over the pes anserinus. Both the semitendinosus and gracilis tendons were harvested using an open tendon stripper. The tendons were then folded to form a 4-strand hamstring graft, and both ends were secured with whip-stitch suture using a No. 5 polyester suture (Ethibond)[9]
Peroneus longus tendon harvesting
Peroneus tendon harvesting was done in the ipsilateral leg or contralateral leg. The peroneus longus tendon was harvested with a 2 cm longitudinal skin incision at the posterolateral side of the fibula just over the peroneus tendon, 2–3 cm proximal to the posterior border of the lateral malleolus. After exposing the distal peroneus longus, a stripper was used to harvest the tendon to about 4–5 cm below the fibular head to avoid peroneal nerve injury. Then both peroneus tendons were sutured distally. The superficial fascia and fat of the harvested tendon were removed, and the rough edge was trimmed carefully. The tendon was doubled and triple up longitudinally through the middle to obtain a 2-strand autograft, and its ends were whip-stitched with a No. 5 polyester suture (Ethibond) and pre-tensioning was done[10]
Femoral tunnel preparation
AMP technique: The medial side of the lateral femoral condyle was also cleared, and the posteromedial edge of the lateral condyle was identified. Femoral footprint was identified, and midpoint of the footprint was marked, and the guide wire was passed with knee in maximum flexion[11].
Tibial tunnel preparation
After preserving the tibial stump remnants, free-floating fibers of ACL, if any, were shaved off. After visualizing the stump at the tibial ACL footprint, with the knee flexed at 90°, an external tibial tunnel drill guide/zig was placed at an angle of 55° in the sagittal plane and 20° in the frontal plane to allow the guide pin to enter intra-articularly in the center of the tibial ACL stump. The tibial tunnel was drilled over the guide wire with the appropriate size reamer as per the graft size. The graft was transfixed, while maintaining appropriate tension, in the femoral and tibial tunnel using endobutton with loop titanium screw polyethylene ether ketone (PEEK) bioabsorbable screw. Postoperatively, compression dressing and knee immobilizer were applied. Knee society score was evaluated preoperatively as well as immediate postoperatively; at 2 months follow-up until 1 year. Statistical data were collected based on knee society score using SPSS software (Ilinois, Chicago). P < 0.05 was statistically significant[12].
Autograft fixation
The intra-articular surgical technique was identical: The femoral tunnel and the tibial tunnel were drilled independently in anatomical position, and implantation of the tendon was performed. The prepared autograft tendon was implanted, and femoral fixation and tibia site fixation using both side rigid fixation, rigid and suspensory fixation, and both side suspensory fixation using PEEK interference screw, titanium interference screw, biodegradable screws, EcoButton knotless Rope Knotless PEEK suture Anchor, etc. With the advent of faster and more aggressive rehabilitation protocols, the primary aim of graft fixation is to provide stability of the graft within the bone tunnel until graft-to-bone incorporation is accomplished. Optimal graft fixation minimizes graft elongation, longitudinal (“bungee effect”), and transverse (“windshield wiper”) graft movement, as well as influx of synovial fluid into the bone tunnel by maximizing strength, stiffness, stability, and durability. Despite advancements in graft fixation methods, the fixation point remains the weakest link in the graft-to-bone interface and is therefore crucial to the success of ACL-R. Several direct and indirect methods of graft fixation have been described. Direct methods include absorbable and non-absorbable interference screws, cross pins, staples, washers, or hardware-free press-fit fixation, whereas indirect devices include fixed or adjustable suspensory cortical button fixation. At this point, there is no clear consensus regarding the “best” graft fixation method, as each option has advantages and disadvantages. Several recent meta-analyses and network meta-analyses have demonstrated no superiority in clinical or patient-reported outcomes of any particular fixation method. Advantages of suspensory fixation include the ease and simplicity of technique, the possibility of a thicker graft with higher graft-to-bone contact area resulting in superior graft incorporation, as well as excellent fixation strength and stiffness. When comparing fixed loop-to-adjustable loop suspension, superior biomechanical results have been observed for fixed-loop devices. Compared to interference screws, less tunnel widening is seen when using suspensory fixation or cross pins, which becomes relevant in revision cases. Graft elongation as well as longitudinal and transverse movements appears to be lower using interference screws, especially when screws are placed close to the joint surface. Hardware-free press-ft techniques have been reported, showing promising outcomes comparable to traditional techniques with low rates of tunnel enlargement[13,14] (Fig. 2)
Rehabilitation
Patients were discharged with the knee immobilizer the day after the surgery. Both groups were treated with the standard post-operative protocol for ACL-R. Full weight-bearing walking with brace and walker, static quadriceps, and ankle pump exercises began immediately after surgery. The first 2 weeks allowed a motion range of 0–60°. Full flexion was obtained after >3 weeks after the surgery. Running was permitted after 3–4 months, and returning to sports activity was recommended after completing functional outcome tests 6–9 months after the operation[15]
Observations and Results
Study on clinical and functional outcome of Arthroscopic ACL reconstruction was carried out on 90 patients who were diagnosed and operated for Arthroscopic ACL reconstruction from January 2019 to January 2023. All patients were regularly assessed up to 12 months postoperatively. In our study, out of 90 patients, 42 patients were between 20 and 30 years, 35 patients were between 31 and 40 years, and only 13 patients among 41–50 years age group (mean age 33 years.) Male preponderance was found to be high; Male (n = 79 patients, 87.77%) compared to females (n = 11 patients, 12.23%). Side of injury was almost equal on both right (53.33%) and left (46.67%) which was statistically not significant. The most common mode of injury was vehicular accidents (53.33%), followed by twisting injury (30%) and sports-related injury (16.67%). All patients had Lachman tests and anterior drawer tests positive (96.67% and 91.11%) respectively. Among 90 patients, n = 19 patients (21.21%) had medial meniscus injury; n = 3 patients (3%) had lateral meniscus injury, n = 3 patients (3%) had posterior cruciate ligament (PCL) injury and 2 patients (2.47%) had medial collateral ligament (MCL) injury. In magnetic resonance imaging findings, 61 patients (68%) had isolated ACL tear with buckling of PCL; 3 patients (3%) had ACL + PCL mid-substance tear; 15 patients (17%) had ACL + medial meniscus tear; 8 patients (8%) had ACL + lateral meniscus tear; and 3 patients (2.94%) had terrible triad of ACL + MCL + medial meniscus injury. Fifty-three patients (59%) semitendinosus and gracilis graft were harvested. Whereas in 37 patients (41%) peroneus longus graft was used. In 61 patients (68%) endobutton switch loop, 10 patients (12%) titanium screw, and 19 patients (21%) PEEK screw, femoral fixation was done. At the final follow-up, 79 patients (87.78%) did not have any pain, 6 patients (6.67%) had mild/occasional pain, 3 patients (3.33%) had mild pain while climbing stairs, and 2 (2.22%) had occasional mild pain while walking and climbing stairs. Out of 90 patients, 85 patients (94.45%) had achieved full knee range of motion, and 5 patients (5.55%) had achieved a range of motion between 116 and 120 at final follow-up, while 16 patients (17.78%) had lag of <10° and 3 patients (3.33%) had lag of more than 10°. At the final follow-up, 3 patients (3.33%) had extension lag of <10°. It might be due to the reason that they presented to us after 9 months of initial trauma leading to significant disuse quadriceps wasting. All patients were checked for anterior-posterior stability at regular follow-up using Lachman test. Out of 90 patients, 85 patients (94.45%) did not have any anterior-posterior instability at final follow-up, while 5 patients (5.56%) had instability of < 5 mm. At the final follow-up, 85 patients (94.45%) were able to walk for long distances without any difficulty, and 5 patients (5.56%) were able to walk more than 10 blocks. At the final follow-up, all 90 patients were able to climb up and down stairs normally. At the final follow-up, considering both clinical and functional Knee Society Score, we can conclude that clinical findings match with functional outcomes. Moreover, 85 patients (94.45%) had excellent and remaining 5 patients (5.56%) had good outcome. Out of 90 patients 53 were operated with semitendinosus and gracilis graft and all 53 patients shows excellent outcome (SCORE) while 37 were operated with peroneus longus graft 32 patients shows excellent outcome (SCORE) and five patients shows good outcome (SCORE). The knee society score based on graft harvesting did not show a significant difference at the final follow-up. We have evaluated anterior laxity clinically using Lachman test at the final follow-up. Out of 90 patients, 87 patients (94.45%) did not have anterior laxity with Lachman test at the final follow-up. Lachman test was positive in the remaining 3 patients (5.56%). Even with a positive Lachman test, 2 patients among these three patients had excellent outcome and other one had good outcome according to Knee Society. Only 3 patients (3.33%) had complications. Two patients had superficial suture infection which subsided with suture removal and oral antibiotics (according to pus culture report) for 6 weeks. One patient had an allergy to PEEK screw and Ethibond™ from the tibial side which was then removed at 3 months which was followed by debridement. Subsequently, at the final follow-up, there was Lachman test positive and the patient refused for revision arthroscopic reconstruction[16].
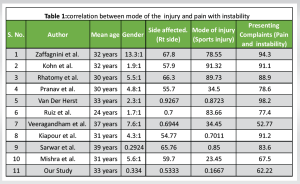
Knee stability is affected by both passive (ligamentous) and active (neuromuscular) joint restraints. Among the contributors to knee joint stability, the ACL has long been considered the primary passive restraint to anterior translation of the tibia with respect to the femur. Moreover, the ACL contributes to knee rotational stability in both frontal and transverse planes due to its specific orientation. In our study, mean age of patients is 33 years with a male preponderance ratio of 8:1. In our study, 79 patients were males (87.78%) and 11 were females (12.22). Forty-eight patients had the right ACL tear, while remaining 42 patients had the left ACL tear. Thus, right side involvement is marginally higher than left which was not statistically significant. The most common mode of injury in our study is road traffic accident (53.33%) followed by twisting injury (30%) and sports injury (16.67%). Fifty-six patients (62.22%) out of 90 patients had mainly complains of instability/giving away and pain during normal work or walking. In our study, Lachman test was positive in 96.67% of patients while anterior drawer test was positive in 91.11% of patient
[table 1]
Associated injuries
Out of 90 patients, 3 patients (2.94%) had MCL, 3 patients (2.94%) had PCL injury, and 23 patients (24%) had meniscus injury (medial meniscus tear [n = 15, 65.21%] > lateral meniscus tear [n = 8, 35.79%]). Other studies with associated meniscus injury along with ACL injury e.g., Kelly et al. Bellabarba C et al. Lee JJ et al. Sudevan et al. all studies tell medial meniscus injury is more common as compared with lateral meniscus injury.
Semitendinosus-gracilis versus peroneus longus graft
In our study, out of 90 patients in 53 patients ACL reconstruction was done using Semitendinosus and gracilis graft while 37 patients were operated with peroneus longus graft. At the final follow-up, all 53 patients (100%) operated with semitendinosus and gracilis grafting have achieved excellent result according to the Knee Society Score while out of 37 patients who were operated with peroneus longus graft, 32 patients have achieved excellent result while five patients have achieved good result according to Knee Society Score. This was not statistically significant. None of the patients had quadriceps or bone-patellar tendon graft harvest. No augmentation with tape or sutures was used in any of ACL reconstruction. In other studies, for example, Rhatomy et al. suggested that patients operated with peroneus longus graft, showing the excellent result is slightly higher (92.5%) compared to semitendinosus and gracilis graft (88.8%); Ertogrul et al. studied semitendinosus and gracilis had better result (94%) when compared with peroneus longus graft harvest (92%).
Knee range of motion at final follow–up: In our study, out of 90 patients, 85 patients (94.45%) have achieved full knee range of motion at final follow-up. In Other studies, for example, Veeragandham et al. 77.77%; Anderson et al 83.33% and Chen et al. 91% of patients have achieved full knee range of motion.
In our studies, 94.45% showed excellent result compared to other studies, for example, Chen et al. (91%); Colombet et al. (94%); Rai et al. (95%); Rhatomy et al. (92%). This study includes 90 patients who were diagnosed to have ACL injury and underwent arthroscopic reconstruction of ACL. The mean age in our study is 33 years with male predominance. Road traffic accident is the common mode of injury in our study. In our study, 56 (62.22%) out of 90 patients presented to us with complaints of both instability and pain during walking/stair climbing (especially downstairs). Preoperatively, 87/90 patients (96.67%) showed Lachman test positive while 82/90 patients (91.11%) had a positive anterior drawer test. Patients with MCL, PCL, and menisci injuries were treated accordingly along with arthroscopic ACL reconstruction. All patients in our study had SB ACL reconstruction. Semitendinosus and gracilis grafts were used for ACL reconstruction in 52 (57.78%) out of 34 patients while peroneus longus graft was used for remaining 48 patients (42.22%). In 61 patients (68%) endobutton with loop, 10 patients (12%) titanium screw 19 patients (21%) PEEK screw femoral fixation done. Only 3 patients (3.33%) in our study had developed complication in the form of superficial wound infection which was treated by regular dressing and antibiotics. Preoperatively 85 patients had poor result and five patients had fair result according to Knee Society Score. At the final follow-up, 85 patients had excellent result and remaining five patients had good result using Knee Society Score. Five patients who had good result were operated with peroneus longus grafting. Among these three patients, one had femoral fixation using suspensory method while another had aperture femoral fixation. Out of these two patients, one patient presented to us at 9th month of injury with significant quadriceps wasting and both these patients were not compliant to physiotherapy. Out of 90 patients, 53 were operated with semitendinosus and gracilis graft, and all 53 patients showed excellent outcome, while 37 were operated with peroneus longus graft 32 patients showed excellent outcome and five patients showed good outcome. Out of 90 patients, 87 patients (94.45%) did not have anterior laxity with Lachman test at the final follow-up. Lachman test was positive in remaining 3 patients (5.56%). Even with a positive Lachman test, two patients among these three patients had excellent outcome and other one patient had good outcome according to Knee Society. Limitation of our study is a small sample size and shorter duration of follow-up. Further future studies are required to validate our results at various institutes.
Graft choice has a considerable influence on post-operative outcomes and remains an easily adjustable surgical factor affecting graft rupture and reoperation rates. When comparing anatomical, histological, and morphological features of commonly used grafts to the native ACL, none can perfectly replicate the complex characteristics of the native ACL. Results achieved with hamstrings as well as peroneus longus graft are excellent. Peroneus longus graft harvesting technique is relatively simple and less time-consuming and has advantage of producing a larger graft diameter. The most crucial finding of this study was that the peroneus longus tendon seemed to be an appropriate autograft option for ACL-R, provided good functional results, prevented potential complications of the autograft harvested from the knee region, and did not significantly affect the ankle joint. The clinical relevance of the current study is that the peroneus longus as an alternative graft in ACL-R can be recommended because it shows good functional results compared to the hamstring tendon with less donor site morbidity.
Clinical massage can aid in the recovery of the peroneus longus graft used for ACL reconstruction by improving blood flow, reducing muscle tension, and promoting healing. Compared to hamstring grafts, peroneus longus grafts may offer benefits such as reduced donor site morbidity and potentially quicker recovery of strength and function. The specific advantages can depend on individual patient factors and the surgeon’s expertise.
References
- 1.Van Eck CF, Schreiber VM, Liu TT, Fu FH. The anatomic approach to primary, revision and augmentation anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2010;18:1154-63. [Google Scholar]
- 2.Louboutin H, Debarge R, Richou J, Selmi TA, Donell ST, Neyret P, et al. Osteoarthritis in patients with anterior cruciate ligament rupture: A review of risk factors. Knee 2009;16:239-44. [Google Scholar]
- 3.Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, et al. Incidence of anterior cruciate ligament tears and reconstruction. On: A 21-year population-based study. Am J Sports Med 2016;44:1502-7. [Google Scholar]
- 4.Salzler MJ, Harner CD. Tunnel placement for the ACL during reconstructive surgery of the knee. A critical analysis review. JBJS Rev 2014;2:e3. [Google Scholar]
- 5.Ferretti M, Edkahl M, Shen W, Fu FH. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: An anatomic study. Arthroscopy 2007;23:1218-25. [Google Scholar]
- 6.Kopf S, Musahl V, Tashman S, Szczodry M, Shen W, Fu FH. A systematic review of the femoral origin and tibial insertion morphology of the ACL. Knee Surg Sports Traumatol Arthrosc 2009;17:213-19. [Google Scholar]
- 7.Klapour AM, Murray MM. Basic science of anterior cruciate ligament injury and repair. Bone Joint Res 2014;3:20-31. [Google Scholar]
- 8.Jackson DW, Gasser SI. Tibial tunnel placement in ACL reconstruction. Arthroscopy 1994;10:124-31. [Google Scholar]
- 9.Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of anterior cruciate ligament. Am J Sports Med 1999;27:444-54. [Google Scholar]
- 10.Ruiz AL, Kelly M, Nutton RW. Arthroscopic ACL reconstruction: A 5-9 year follow-up. Knee 2002;9:197-200. [Google Scholar]
- 11.Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR Jr. Arthroscopic anterior cruciate ligament reconstruction: A metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med 2003;31:2-11. [Google Scholar]
- 12.Colombet P, Robinson J, Christel P, Franceschi JP, Djian P. Using navigation to measure rotation kinematics during ACL reconstruction. Clin Orthop Relat Res 2006;454:1-7. [Google Scholar]
- 13.Zaffagnini S, Bignozzi S, Martelli S, Lopomo N, Marcacci M. Does ACL reconstruction restore knee stability in combined lesions? An in vivo study. Clin Orthop Relat Res 2007;454:95-9. [Google Scholar]
- 14.Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: Meta-analysis of functional scores. Clin Orthop Relat Res 2007;458:180-7. [Google Scholar]
- 15.Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions, and ACL tears: A systematic review. Br Med Bull 2007;84:5-23. [Google Scholar]
- 16.Cirstoiu C, Circota G, Panaitescu C, Niculaita R. The advantage of arthroscopic anterior cruciate ligament reconstruction with autograft from the tendons of the semitendinosus-gracilis muscles for the recovery of the stability of the knee. J Clin Med 2011;6:109-13. [Google Scholar]