Tb is a great clinical masquerader. Atypical presentations are no longer uncommon. The varying presentations of osteoarticular Tb pose many diagnostic challenges in the clinician’s daily practice. Good clinical acumen and effective timely use of modern diagnostic adjuncts such as PCR and GeneXpert are critical in early diagnosis. Timely intervention significantly reduces patient morbidity and community spread.
Dr. Aizel Sherief Palasseril, Department of Orthopaedics, Sree Balaji Medical College Hospital, 7-CLC works Road, Shankar Nagar, Chromepet, Chennai- 600044, Tamil Nadu, India. E-mail: aizelsherief@gmail.com
Introduction: Elbow joint is the most common affliction in upper limb tuberculosis (TB). A review of literature shows varying clinical presentations of TB in the elbow, with and without detectable primary foci.
Case Report: We report a rare case of post-traumatic reactivation of latent TB of elbow which mimicked septic arthritis, in a healthy adult who suffered an elbow contusion injury following an road traffic accident. It was misdiagnosed as septic arthritis elsewhere and was going non-responsive to broad-spectrum antibiotics. At our center, we suspected TB and magnetic resonance imaging done showed joint destruction and fibrous ankylosis. He underwent joint debridement with removal of fibrous tissue and synovectomy. The synovial biopsy and polymerase chain reaction were consistent with TB. At 1-year follow-up on anti-tuberculosis treatment, he was relatively pain free and regained functional range of movement.
Conclusion: Post-traumatic reactivation of TB in joints, though a rare entity, should be kept in mind in patients who are non-responsive to routine antibiotics, especially in endemic areas. Early and accurate diagnosis prevents progression to articular destruction and fibrous ankylosis.
Keywords: Latent tuberculosis, trauma, elbow, reactivation, osteoarticular tuberculosis.
Tuberculosis (TB) is still a global health-care burden with an estimated 1.5 million deaths and 10.4 million new cases in 2020, of which 95% being reported from low-and middle-income countries [1]. Osteoarticular Tb accounts for 1–3% of total cases and 30–40% of extrapulmonary cases worldwide [2, 3]. The most common affliction of osteoarticular TB is dorsal spine followed by hip and knee. Elbow joint involvement, though rare, is the most common area affected in the upper limb and accounts for 1–5% of osteoarticular TB [4]. A review of literature has shown varying presentations of TB in elbow joint with hematogenous spread from a primary focus being the primary reason followed by lymphatic spread, inoculation from a contiguous site, or direct inoculation [5, 6, 7, 8, 9]. A recent study by McGuire et al. [10] suggested elbow as the second-largest site (19.4%) of extrapulmonary TB after knee joint (23.7%) in their large cohort of cases. This study has brought back our focus to elbow TB, which was thought to be less affected. To our knowledge, no cases of post-traumatic TB of elbow have been reported so far in a closed injury setting. This particular presentation is a diagnostic dilemma and treatment challenge, as much of the clinician thoughts are diverted in the direction of septic arthritis in a post-traumatic scenario. This case highlights the importance of keeping TB as a differential in post-traumatic infection settings, especially in non-responders to routine antibiotics. Early diagnosis and initiation of anti-tuberculosis treatment (ATT) can save the joint from irreversible articular damage and loss of function and reduce patient morbidity. Surgical debridement may be necessitated in terminal stages to contain infection, correct deformity, instability, and restoration of function.
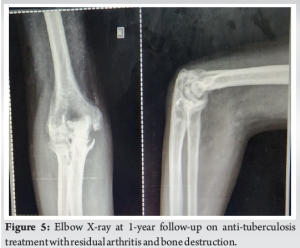
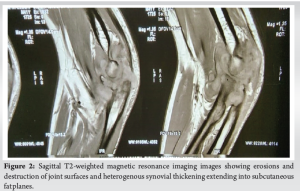
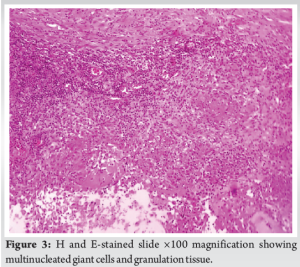
A 41-year-old well-nourished non-smoker from a low socioeconomic status working as a taxi driver with no significant comorbidities or TB history presented to our center in July 2021 with a 2-year-old history of pain, swelling, and restriction of movement of his right elbow which he believes began after a contusion injury to his elbow following an road traffic accident. He initially underwent treatment at a local bone setter where he had few sessions of massage and herbal packings which gave him no relief. He was treated at multiple hospitals where the clinicians suspected subacute septic arthritis and put him on long durations of broad-spectrum antibiotics which proved futile for his symptoms. In fact, he never had any contributory history to suspect TB and his clinical signs and symptoms were vague. By the time, he presented to our hospital his pain, swelling, and restriction of movements increased to such an extent that he was unable to carry out his activities of daily living. On examination, his elbow was swollen, warm, and had a fixed flexion deformity of 90° with further flexion up to 110°. The X-ray done (Fig. 1) revealed severe joint destruction and magnetic resonance imaging (MRI) done (Fig. 2) revealed the same along with joint effusion, extensive heterogenous synovial thickening with extension posteriorly into the overlying subcutaneous fat plane, and edema in the adjacent muscle group. His blood counts were normal, but erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were raised to 25 mm and 2.4 mg/dL, respectively. RA factor was negative. His sputum AFB was negative and a chest X-ray done was unremarkable. However, his Mantoux test came positive. Our provisional diagnosis was TB and the patient underwent joint debridement for removal of fibrous tissue and synovectomy. Multiple intraoperative specimens sent for AFB, gram staining, aerobic and anaerobic cultures, and fungal KOH mount, turned negative. As expected, the TB GeneXpert result came positive. Histopathological examination of the synovial biopsy was also consistent with TB and showed necrotizing granulomatous inflammation (Fig. 3 and 4). The patient was put on ATT regimen for osteoarticular TB for 1 year. This included isoniazid, rifampicin, pyrazinamide, ethambutol for 2 months of intensive phase followed by 10 months of continuation phase with isoniazid and rifampicin. At 1-year follow-up, the patient is relieved of his initial pain and swelling and has also regained a functional range of elbow movement even though his radiological picture shows severe articular destruction (Fig. 5). His blood ESR and CRP has also returned to normal. However, his functional recovery is not complete owing to the irreversible joint destruction; he already had before initiation of the treatment. This highlights the importance of early diagnosis and timely initiation of ATT to prevent fibrous ankylosis and arthritis. The patient has been advised to undergo a total elbow arthroplasty to regain his full range of movements.


Even though TB elbow is an uncommon presentation in the developed world, in endemic areas, the clinicians should have a high index of clinical suspicion, especially when patients present with atypical features of infection and are non-responsive to routine antibiotics. Even in the developed world, there is an increased interest in atypical osteoarticular infections such as TB and fungi due to the growing number of immunodeficient patients with lifestyle diseases such as diabetes, HIV, and autoimmune disorders [11]. Tb is unique in infecting only 3 out of 10 people who are exposed and among the infected, 95% can contain the infection with their T cell immune response, rendering the disease latent with some viable bacteria remaining [12]. However, it has been reported that more likely in the first 5 years, up to 5% of these cases can get reactivated, especially in immunocompromised and malnourished [13]. Our case was unique in that the reactivation happened even though he was a healthy well-nourished adult with no detectable immunocompromise. A literature review of reported cases of elbow TB shows variable presentations either as a chronic infection depicting chronic osteomyelitis or septic arthritis [14-17]. The most challenging part in osteoarticular TB is confirmation of diagnosis. There is no single test for diagnosing osteoarticular TB with high sensitivity and specificity [18]. A combined approach using clinico-radiological findings and their microbiological and histopathological correlation would be ideal. Non-invasive techniques include roentgenographic modalities such as X-rays, computed tomography (CT), positron emission tomography CT, ultrasound, and MRI. Invasive modalities include analyzing hemograms, immunological testing using Mantoux, Interferon-gamma release assays, Ziehl–Neelsen staining, fluorescence microscopy, and bactec cultures of specimens, histopathological correlation, and modern molecular PCR techniques like GeneXpert [19]. In this case, the exact pathophysiology of probable reactivation of latent TB is poorly understood. A literature review to identify the same yielded no results. The authors would like to postulate a probable mechanism of seeding from a reactivated latent focus in the body, triggered by the systemic inflammatory response of trauma and increased local vascularity and hyperemia. However, this needs to be validated with future studies.
In areas of high TB prevalence like India, where 40% of the population are latently infected, clinicians should have high index of clinical suspicion for osteoarticular TB and a low threshold for biopsy in patients presenting with chronic vague articular symptoms and signs of infection. Delay in timely diagnosis of osteoarticular TB can result in residual arthritis and significant patient morbidity as demonstrated in our case. Apart from olden times when diagnostic modalities for TB where limited, today, we have modern adjuncts like Interferon gamma release assays, PCR’s, and BACTEC cultures for quick and accurate diagnosis of TB. Appropriate usage of these modalities is warranted in suspicious cases and early treatment considerably reduces patient morbidity, community spread, and health-care burden. Our case report warrants more research and interest into the possible reasons for reactivation of latent TB in a closed post-traumatic clinical scenario.
Post-traumatic reactivation of latent TB should be an important differential in TB endemic regions such as India and Asia, even in a closed injury. Timely diagnosis and intervention are critical in significantly reducing patient morbidity and community spread.
References
- 1.WHO. Global Health Observatory (GHO) Data: Tuberculosis. Available from: https://www.who.int/gho/tb/en [Last accessed on 10 Sep 2024]. [Google Scholar]
- 2.Jain AK. Tuberculosis of Bones Joints and Spine. Evidence Based Management Guide. 1st ed. New Delhi: CBS Publication; 2017. p. 1. [Google Scholar]
- 3.Tuli SM. Tuberculosis of the Skeletal System (Bones, Joints, Spine, and Bursal Sheaths). 4th ed. New Delhi: Jaypee Brothers’ Publishers Private Ltd.; 2010. [Google Scholar]
- 4.Liao Q, Shepherd JG, Hasnie S. Mycobacterium tuberculosis of the elbow joint. BMJ Case Rep 2017;2017:bcr2017222735. [Google Scholar]
- 5.Holder SF, Hopson C, Vonkuster L. Tuberculous arthritis of the elbow presenting as chronic bursitis of the olecranon: A case report. J Bone Joint Surg (Am) 1985;67:1127-9. [Google Scholar]
- 6.Magnussen A, Amirthanayagam T, Sofat R. Osteoarticular tuberculosis: The great mimicker still catches us out--a case report. Acta Orthop 2016;87:83-4. [Google Scholar]
- 7.Heycock JB, Noble TC. Four cases of syringe transmitted tuberculosis. Tubercle 1961;42:25-7. [Google Scholar]
- 8.Wright T, Sundaram M, McDonald D. Radiologic case study: Tuberculous osteomyelitis and arthritis. Orthopedics 1996;19:699-702. [Google Scholar]
- 9.Abdelwahab IF, Kenan S, Hermann G, Klein MJ. Tuberculous gluteal abscess without bone involvement. Skeletal Radiol 1998;27:36-9. [Google Scholar]
- 10.McGuire E, Rajagopal S, Vaikunthanathan T, Krutikov M, Burman M, Rahman A, et al. Extraspinal articular tuberculosis: An 11-year retrospective study of demographic features and clinical outcomes in East London. J Infect 2020;81:383-9. [Google Scholar]
- 11.Palasseril AS, Gopinath SV, Thanikachalam R, Prabhu SA, Rajamanoharan V, Shahul MR. “Debaryomyces subglobosus” - Management of a rare case of fungal septic arthritis post arthroscopic rotator cuff repair - a case report. SICOT J 2021;7:60. [Google Scholar]
- 12.Sharma N, Basu S, Chopra KK. Achieving TB elimination in India: The role of latent TB management. Indian J Tuberc 2019;66:30-3. [Google Scholar]
- 13.WHO. Latent Tuberculosis Infection: Updated and Consolidated Guidelines for Programmatic Management. Geneva: World Health Organization; 2018. Available from: https://www.who.int/publications/i/item/9789241550239 [Last accessed 10 Sep 2024]. [Google Scholar]
- 14.Chen WS, Wang CJ, Eng HL. Tuberculous arthritis of the elbow. Int Orthop 1977;21:367-70. [Google Scholar]
- 15.Parkinson RW, Hodgson SP, Noble J. Tuberculosis of the elbow: A report of five cases. J Bone Joint Surg Br 1990;72:523-4. [Google Scholar]
- 16.Vohra R, Kang HS. Tuberculosis of the elbow. A report of 10 cases. Acta Orthop Scand 1995;66:57-8. [Google Scholar]
- 17.Wilson JN. Tuberculosis of the elbow; a study of thirty-one cases. J Bone Joint Surg Br 1953;35-B:551-60. [Google Scholar]
- 18.Agashe VM, Johari AN, Shah M, Anjum R, Romano C, Drago L, et al. Diagnosis of osteoarticular tuberculosis: Perceptions, protocols, practices, and priorities in the endemic and non-endemic areas of the world-A WAIOT view. Microorganisms 2020;8:1312. [Google Scholar]
- 19.Dhammi IK, Kumar S. Current concepts in diagnosis and management of osteoarticular tuberculosis. Ortho J MPC 2020;26:3-13. [Google Scholar]