An orthopedic surgeon must maintain a strong suspicion for etiologies such as metabolic bone diseases such as ochronosis and be well-prepared for challenging exposures and surgical procedures.
Dr. Dhrushith Ettakkepraven Puthanveetil, Department of Orthopaedics, Government Medical College Trivandrum, Kerala, India. E-mail: epdhrushith@gmail.com
Introduction: Alkaptonuria is a rare metabolic disorder that follows an autosomal recessive genetic inheritance pattern. It is distinguished by the buildup of homogentisic acid in tissues due to deficient homogentisic acid oxidase enzyme activity. The excess homogentisic acid is expelled through urine, darkening it on oxidation. Moreover, it deposits in connective tissues, imparting a characteristic blue-black pigmentation. This condition is known as Ochronosis or black bone disease. This accumulation over time renders cartilage brittle, potentially leading to ochronotic arthropathy.
Case Report: A 46-year-old lady presented with long-standing bilateral knee pain for 8 years with a predominant focus on the right side. Recurrent swelling and pain episodes in the right knee were noted, occurring without significant traumatic events. Despite various conservative treatments attempted to alleviate her knee pain, the patient experienced minimal relief. On examination, the patient demonstrated difficulty in ambulating, with severe tenderness along the joint line and a restricted range of motion. Standing knee X-rays revealed severe tricompartmental osteoarthritis and a correctable valgus deformity of 5. She underwent total knee replacement. A provisional diagnosis of ochronosis was made intraoperatively, later confirmed on histopathological examination of the tissue, and the patient was evaluated retrospectively.
Conclusion: Ochronotic arthropathies are rare conditions- characterized by articular cartilage damage. They are typically diagnosed post-surgery, often when surgeons observe the dark coloration of cartilage. However, joint replacement surgery can safely and effectively manage these conditions, leading to favorable outcomes, including improved functionality, pain alleviation, and heightened patient satisfaction.
Keywords: Ochronosis, alkaptonuria, ochronotic arthropathy, total knee arthroplasty.
Mild discoloration of the articular cartilage typically develops gradually with age. However, in certain circumstances, pathological tissue pigmentation can occur, including conditions such as alkaptonuria (ochronosis) [1], pigmented villonodular synovitis, chronic phenol poisoning, burns, hemosiderosis [2], medication use like Levodopa [3] and methyldopa for Parkinson’s disease, certain antibiotics such as minocycline [4], and exposure to substances like hydroquinone. Alkaptonuria, a rare metabolic disorder, follows an autosomal recessive genetic pattern resulting from a mutation in chromosome 3 (3q21-q23). It is distinguished by the buildup of homogentisic acid in tissues due to deficient homogentisic acid oxidase activity. This condition, known as ochronosis or black bone disease, manifests with dark urine and blackish discoloration, notably in connective tissues such as cartilage and bone [5]. The excess homogentisic acid is expelled through urine, darkening it on oxidation. Moreover, it deposits in connective tissues, imparting a characteristic blue-black pigmentation [6, 7]. This accumulation over time renders cartilage brittle, potentially leading to ochronotic arthropathy. Symptoms such as inflammatory arthritis and stiffness predominantly affect larger joints such as knees and hips, while spinal ankylosis and kyphosis may arise from disc calcification [5]. The reported case underwent total knee replacement, and blackish discoloration of cartilage and synovium was detected operatively. Histopathological examination of the specimen was suggestive of ochronosis, and the patient was assessed retrospectively. The patient expressed satisfaction with the outcome and could resume daily activities after the surgery.
The reported case is for a 46-year-old Indian lady; she initially sought medical attention at our tertiary center outpatient clinic, reporting long-standing bilateral knee pain for 8 years with a predominant focus on the right side. Recurrent swelling and pain episodes in the right knee were noted, occurring without significant traumatic events. Despite various conservative treatments attempted to alleviate her knee pain, including long-term physiotherapy and lifestyle adjustments, the patient experienced minimal relief. She is married, a non-smoker, with no prior surgical history, does not engage in sports, and has no relevant medication history. In addition, there is no family history of similar knee conditions. On examination, the patient demonstrated difficulty ambulating due to the primary complaint of knee pain. Severe tenderness along the joint line and restricted range of motion, limited from 10 to 100o, were observed during knee examination. Standing knee X-rays revealed severe tricompartmental osteoarthritis and a correctable valgus deformity of 5o (Fig. 1). The knee exhibited stability in both anteroposterior and varus-valgus translations. The patient scaled her knee pain on the Visual Analog Scale as 8/10, and her function scored severe difficulty (24) on the Knee Injury and Osteoarthritis Outcome Score (KOOS) [8].
Operation
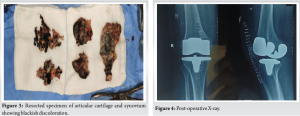
We performed a total knee arthroplasty (TKA) of the right knee under spinal anesthesia. The medial parapatellar approach exposed the right knee, revealing widespread blackish pigmentation of articular cartilage and synovial membrane. The patellar tendon was much stiffer than usual and was carefully mobilized to avoid injuring the knee extensor mechanism. Following the tibial and femoral cuts, we noticed the pigmentation localized to the cartilage layer (Figs. 2 and 3). We inserted a cemented mobile-bearing posterior stabilized prosthesis (Buechel-Pappas). The resected bone cuts and synovial membranes were sent for histopathological examination. Despite a thorough assessment after the release of the femur tourniquet, no significant bleeding lesions were identified. The post-operative period was uneventful, and the patient was retrospectively assessed for alkaptonuria after obtaining a histopathology report (Fig. 4). The patient was rehabilitated postoperatively as per standard rehabilitation protocols. The patient was followed up regularly for 2 years. The patient expressed satisfaction with the functional outcome of a score of 84.6(KOOS-JR) at the end of 2 years (Fig. 5).
Histological examination
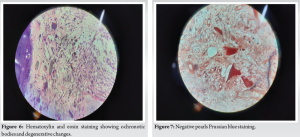
Microscopic examination with hematoxylin and eosin staining of the cartilage revealed a noticeable decrease in the number of chondrocytes and chondrocyte fragments suggestive of degenerative changes. Numerous yellow-brown, banana/sickle-shaped, and round ochronotic bodies were identified along with hemosiderin-loaded macrophages [9] (Fig. 6). Pearl’s Prussian blue staining was negative, indicating no iron deposition (i.e., hemosiderosis) in the joint surface cartilage (Fig. 7).
Severe pigmentary abnormalities in the joint occasionally occur after several specific conditions, such as ochronotic arthropathy due to alkaptonuria [1], hemosiderosis [2], and the use of drugs for Parkinson’s disease [3] or antibiotics [4]. In this case, the severe black coloration of the articular cartilage appears to have occurred due to ochronosis. Even though this condition can be diagnosed through a urine test, diagnosis is generally confirmed after joint surgery [10, 11]. Ochronosis metabolic arthropathy presents as a rare degenerative joint disease characterized by the accumulation of homogentisic acid on the articular cartilages of large joints and the spine [5]. Typically, symptomatic ochronosis in joints emerges after age forty and clinically resembles osteoarthritis [6, 7]. This condition does not display a sex predilection. As per previously published literature, most diagnoses of knee ochronotic arthritis are confirmed intraoperatively [10, 11], mirroring our case and retrograde evaluation was done. Intraoperative analysis of synovial and articular cartilage biopsy revealed numerous yellow-brown, banana/sickle-shaped, and round ochronotic bodies, indicative of ochronosis [9]. Lee et al. conducted a Systematic literature review encompassing 19 case reports from 2000 to 2016 involving 19 patients and 26 TKAs. Their findings revealed favorable outcomes across all cases, with no significant complications. The authors also examined the various types of prostheses used. In line with previous research, they advocated for cemented TKA with a posterior-stabilized prosthesis as the preferred treatment for ochronosis and its recommendation for patients with rheumatoid arthritis [12, 13]. The accumulation of homogentisic acid in the patellar articular cartilage and tendon induces chemical irritation and weakens the tendon [14]. We opted for patella resurfacing due to the dark pigment deposits in the patellar articular cartilage. To prevent ligamentum patellae avulsion during patella resurfacing, we exercised meticulous care in gently everting the patella. It is important to note that these patients may exhibit significant synovitis, potentially leading to bleeding after synovectomy. This could prolong the surgery and complicate the cementing of the prosthesis. To mitigate this, we employed a hemostatic tourniquet and administered tranexamic acid before the tourniquet release, aiming to minimize bleeding and ensure optimal cementing quality [14]. Diagnosis typically happens post-surgery when surgeons notice the dark coloration of the cartilage. Despite limited information, TKA is the preferred treatment for advanced disease, as it alleviates pain and improves function [15]. In the existing literature, no specific post-operative rehabilitation guidelines have been outlined for ochronotic knee arthritis. Therefore, we adopted a similar rehabilitation protocol for standard total knee replacement patients. Total knee replacement has demonstrated favorable outcomes for patients unresponsive to conservative management of ochronotic knee arthritis [15]. Spencer et al. detailed the outcomes of three patients who underwent 11 arthroplasties, involving both upper and lower extremities, for degenerative ochronotic arthropathy. These patients showed positive results during a 12-year follow-up [16]. Our patient expressed satisfaction with a pain-free knee joint after 2 years.
Ochronotic arthropathies are rare conditions characterized by articular cartilage damage. They are typically diagnosed post-surgery, often when surgeons observe the dark coloration of cartilage. However, joint replacement surgery can safely and effectively manage these conditions, leading to favorable outcomes, including improved functionality, pain alleviation, and heightened patient satisfaction.
Given its rarity and frequent lack of detection, the functional outcome of knee arthroplasty in patients with ochronotic arthropathy mirrors that of primary osteoarthritis. The crux lies in accurately diagnosing the condition and anticipating any intraoperative challenges. Long-term follow-up is needed to establish the outcome of TKA in ochronotic arthropathy.
References
- 1.Delialioglu OM, Daglar B, Bayrakci K, Ceyhan E, Tezel K, Erekul S, et al. Ochronosis: Complicated tear of the black meniscus. Knee Surg Sports Traumatol Arthrosc 2009;18:540-2. [Google Scholar]
- 2.Roosendaal G, Mauser-Bunschoten EP, De Kleijn P, Heijnen L, van den Berg HM, Van Rinsum AC, et al. Synovium in haemophilic arthropathy. Haemophilia 1998;4:502-5. [Google Scholar]
- 3.Connolly CE, O’Reilly U, Donlon J. Black cartilage associated with levodopa. Lancet 1986;327:690. [Google Scholar]
- 4.Yang S, Takakubo Y, Kobayashi S, Asano T, Sasaki A, Sasaki K, et al. Minocycline-induced periarticular black bones in inflamed joints which underwent arthroplastic reconstruction. Clin Orthop Surg 2012;4:181-7. [Google Scholar]
- 5.Zatkova A. An update on molecular genetics of Alkaptonuria (AKU). J Inherit Metab Dis 2011;34:1127-36. [Google Scholar]
- 6.Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, et al. Natural history of alkaptonuria. N Engl J Med 2002;347:2111-21. [Google Scholar]
- 7.Harun M, Hayrettin Y, Serhat M, Cuneyt M, Fırat F, Ufuk O. A rare cause of arthropathy: An ochronotic patient with black joints. Int J Surg Case Rep 2014;5:554-7. [Google Scholar]
- 8.Gandek B, Ware JE Jr. Validity and responsiveness of the knee injury and osteoarthritis outcome score: A comparative study among total knee replacement patients. Arthritis Care Res (Hoboken) 2017;69:817-25. [Google Scholar]
- 9.Doganavsargil B, Pehlivanoglu B, Bicer EK, Argin M, Bingul KB, Sezak M, et al. Black joint and synovia: Histopathological evaluation of degenerative joint disease due to Ochronosis. Pathol Res Pract 2015;211:470-7. [Google Scholar]
- 10.Gil JA, Wawrzynski J, Waryasz GR. Orthopedic manifestations of ochronosis: Pathophysiology, presentation, diagnosis, and management. Am J Med 2016;129:536.e1-6. [Google Scholar]
- 11.Drakoulakis E, Varvitsiotis D, Psarea G, Feroussis J. Ochronotic arthropathy: Diagnosis and management: A critical review. Am J Orthop (Belle Mead NJ) 2012;41:80-3. [Google Scholar]
- 12.Lee WC, Tan TL, Chan YH. Total knee arthroplasty in ochronosis arthropathy: A case report and systematic review. Case Rep Orthop 2019;2019:1871856. [Google Scholar]
- 13.Rodriguez JA, Saddler S, Edelman S, Ranawat CS. Long-term results of total knee arthroplasty in class 3 and 4 rheumatoid arthritis. J Arthroplasty 1996;11:141-5. [Google Scholar]
- 14.Ulucay C, Ozler T, Altintas F, Inan M, Onur A, Kocadal AO. Arthroplasty in ochronosis “tips and pearls in surgery”: Case series. J Arthritis 2013;3:116. [Google Scholar]
- 15.Pesciallo C, Garabano G, Rodriguez J, Viale G, Tillet F, Del Sel H. Total knee replacement in alkaptonuric ochronosis. Acta Biomed 2022;93:e2022108. [Google Scholar]
- 16.Spencer JM, Gibbons CL, Sharp RJ, Carr AJ, Athanasou NA. Arthroplasty for ochronotic arthritis: No failure of 11 replacements in 3 patients followed 6-12 years. Acta Orthop Scand 2004;75:355-8. [Google Scholar]