• To correlate radiological parameters with functional outcome following proximal humerus fracture fixed with PHILOS plating • To assess the outcome using radiological parameters and Constant-Murley score • To determine the significance of medial cortex fixation for better post-operative outcome
Dr. K V Arun Kumar, Department of Orthopaedics and Traumatology, Chettinad Hospital and Research Institute, Kelambakkam, Tamil Nadu, India. E-mail: arun5684@gmail.com
Introduction: Proximal humerus fractures are prevalent, especially among the elderly, and pose significant challenges in treatment, particularly for displaced fractures. Despite the availability of various surgical techniques, outcomes remain inconsistent, often due to poor anatomical reduction and fixation. This study examines the correlation between specific radiographic parameters and functional outcomes, aiming to identify key predictors of recovery. By focusing on these parameters, we aim to refine surgical approaches and improve follow-up strategies, ultimately enhancing patient outcomes.
Materials and Methods: A retrospective study involved 40 patients aged 18–75 with proximal humerus fractures, treated with open reduction and plate fixation at Chettinad Hospital between April 2022 and April 2024. All surgeries were performed through anterior deltopectoral approach. Radiographic parameters were evaluated postoperatively, with patients followed for a period of 1 year. Functional outcomes were correlated with radiological parameters using follow-up radiographs and Constant-Murley (C-M) scores.
Results: In this study of 40 patients with proximal humerus fractures, the mean age was 53.24 years, and the majority (60%) were male. The fractures predominantly affected the right side (62.5%), with road traffic accidents and falls being the leading causes. Neer’s classification identified 10 patients with two-part fractures, 21 with three-part fractures, and 9 with four-part fractures. The average neck-shaft angle (NSA) was 138.62° ± 11.09°. Four patients with an NSA of ≤120° had fair to good functional outcomes, while those with an NSA >130° and a well-positioned greater tuberosity (GT) generally had better outcomes. The average distance between the GT and the acromion surface (AS) was 6 mm ± 1.4 mm, influencing shoulder abduction and functional results. Patients with an alpha/beta ratio below 1.40 mm, indicating lower bone density, had a higher incidence of screw cut-out. The mean C-M score at 6 months was 80.72, with 87.5% of patients achieving abduction above 90°. Complications occurred in 8 patients (20%), including varus collapse (10%), abduction <90° (12.5%), infection (2.5%), and screw cut-out (5%). Larger head diameters and heights were associated with better functional scores.
Conclusion: Radiographic parameters such as the NSA, GT to AS distance, head diameter, head height, and alpha/beta ratio are crucial predictors of functional outcomes in proximal humerus fractures treated with PHILOS plates. Accurate reduction and medial column stabilization are a key to minimizing complications and improving patient recovery. Despite generally positive outcomes, challenges such as screw cut-out and varus collapse persist, highlighting the need for meticulous surgical technique and thorough post-operative management.
Keywords: Proximal humerus fractures, PHILOS plating, radiological parameters, plate osteosynthesis, shoulder rehabilitation.
A proximal humerus a fracture that occurs at or close to the humeral surgical neck is the most prevalent fracture involving the scapular girdle in adults. It stands third in frequency following fractures of hip and distal radius [1]. Recent statistics indicate that these fractures now represent close to 7% of all fractures and comprise 80% of all humeral fractures. In individuals over 65, the proximal humerus is the site of the second most frequent upper limb fractures and the third most common non-vertebral osteoporotic fractures, following fractures of the nearby femur and distal far radius [2]. Neer’s categorization is commonly used to classify upper humerus fractures based on fragment angulation >45° or displacement over 10 mm. This classification affects management and outcomes, with 4-part fractures having a poorer prognosis than 2- or 3-part fractures [3]. Proximal humerus fractures are a significant contributor to morbidity in elderly populations and should be a key consideration in healthcare planning. Roughly 80% of these fractures are not out of position and can be effectively handled with conservative methods such as Plaster of Paris. However, the supervision of disarranged fractures remains contentious and difficult. Some experts recommend non-surgical treatment for Neer’s two, three, and four-part proximal humeral fractures in older treatment seekers, though this approach often leads to complications such as pain, stiffness, and functional impairment [4]. According to the AO/ASIF guidelines, addressing these fractures needs adequate reduction, solid fixation, and early mobilization for better functional outcomes. Computed tomography (CT) scans can be advantageous in complex cases to assess fragments [5]. Proximal humerus fractures can be managed using non-invasive approaches when suitable, surgically through options such as percutaneous pinning, plate osteosynthesis (such as PHILOS plating), intramedullary nailing, external fixation, and arthroplasty. Among these, PHILOS plating is widely used and has shown excellent outcomes [5]. Despite satisfactory practical and tailored to patient needs, locking plate complications continue to be high, spanning between 16% and 48.8%, and encompass screw cut-out, intra-articular screw-penetration, subacromial-impingement, varus malalignment, non-union, implant-failure, and osteonecrosis [6]. These issues are generally caused by inadequate surgical technique, faulty implant position, inadequate intraoperative assessment of reduction, and screw length [7]. Radiographic parameters play a crucial role in predicting outcomes, though there is no consensus on the best parameters to use, especially relative to the cross-side uninjured side. Unsatisfactory anatomic diminution, particularly of the inner side column, is associated with higher failure rates following plate fixation. For elderly patients, organizing follow-up examinations is challenging, making it essential to identify radiographic parameters correlating with poor clinical outcomes. These parameters can help determine which patients need closer follow-up and guide surgeons in anatomically restoring these parameters during surgery. The primary goal of this study is to determine the link between resultant function and radiographic parameters of proximal near humeral fractures, such as neck-shaft orientation, distance from the head of the humeral to the greater tuberosity (GT), alpha/beta calculations, head diameter, head height, and calcar screw status.
We did a retrospective analysis encompassing 40 participants who had proximal humerus fractures resolved with an open cutback and plate fixation at Chettinad Hospital and Research Institute from April 2022 to April 2024, patients aged between 18 and 75 years with a lesser follow-up duration of 1 year. Three different surgeons conducted all the surgeries.
Inclusion criteria
- Age more than 18 years
- Based on Neer’s classification two parts, three parts, and four parts fractures of proximal humerus
- The injury duration is <4 weeks.
Exclusion criteria
- Less than 18 years.
- Open proximal humerus fractures
- Infection
- Head injury/vascular injury
- Pathological fracture and malignancy.
Pre-operative planning
The patient was initially stabilized in the emergency department, and local skin conditions were assessed. Pre-operative radiographs were taken to evaluate the fracture morphology, classify according to Neer’s classification and the patient was placed in U-slab immobilization. Pre-anesthetic work-up was completed, and each patient underwent plate osteosynthesis using the standard anterior deltopectoral approach [8,9, 10] (Fig. 1).
Post-operative care
Following surgery, all 40 patients were given a shoulder immobilizer to help stabilize their arms. Post-operative X-rays were obtained the entire day after the procedure to assess fracture positioning, reduction, and support. Physiotherapy for the shoulder was initiated based on fixation stability, bone quality, and patient adherence. Active range of motion (ROM) activities for the elbow, wrist, and hand began on the 1st post-operative day, while passive ROM exercises such as oscillator swings, passive ahead elevation, and outward rotation began in the 2nd week after surgery.
The rehabilitation process included early passive-assisted exercises to prevent adhesion formation. Active exercises were started around 6 weeks after surgery, with strengthening and resistance exercises commencing between 10 and 12 weeks, once bony consolidation was confirmed through X-rays. Subsequent X-rays were scheduled at 4 weeks, 3 months, 6 months, and 12 months to monitor fracture healing and identify potential complications, including screw permeation, screw removal, avascular necrosis, and device loosening. The Constant-Murley (C-M) scores were assessed at each follow-up [11].
Assessment
Antero-posterior views of shoulders were assessed under the supervision of an orthopedic specialist, ensuring the patient was in a standardized position. Measurements were performed using InstaRISPACS from Meddiff Technologies Pvt. Ltd. To minimize magnification errors, plate and screw sizes were employed as scales. An experienced trauma consultant reviewed the radiographs. X-rays were taken immediately after surgery and at 1 month, 3, and 6 and 1 year to assess the quality and the union of the fracture. This assessment considered the neck-shaft angle (NSA), the distance that’s falling within the GT and articular surface (AS), head height, head diameter, alpha distance, beta distance, and whether a calcar-specific screw was present (Fig. 2). Post-check in X-rays was also analyzed for the betterment of the bone, avascular necrosis, device-associated challenges, screw fixing within the joint, and signs of arthritic transformation.
The NSA was calculated by drawing a line parallel to the articular near the border and an erect line through the heads of the humerus center. A third line was drawn in line to the humeral shaft, and the NSA was measured at their intersection [12], the head diameter was calculated by measuring the gap in the middle of the lower and elevated cortices of the articular surface. Head height was the distance from the center of the head diameter and the articular cortex, measured erect to the head diameter [13].
The alpha position is the distance between the outer cortices just above the deltoid tuberosity, and beta distance is the position of the inner cortices at a similar equal level. Alpha/beta is an indirect indicator of bone marrow density and is useful in the prediction of screw cut out [14, 15]. The GT to AS distance was the distance that lies inside the most elevated point on the GT and the highest point on the humeral head [16]. The C-M score evaluates pain, shoulder function in routine activities, all movements, and shoulder toughness [17]. The scoring is made as excellent (100–86 points), good (85–71 points), satisfactory (70–56 points), and poor (below 56 points). Setbacks were recorded with hindsight at each visit [18].
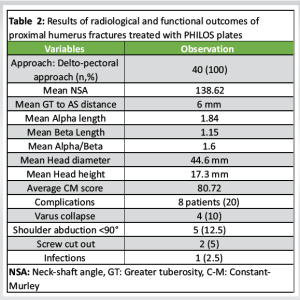
A total of 40 patients were studied, as summarized in Table 1 and table 2. The patients had an average age of 53.24 years, with an age range of 22–75 years. The group comprised 24 males and 16 females. Injuries occurred on the right side in 25 of them and 15 on the left side. The causes of injury included street accidents in 19 of them and falls in 21 patients. Based on Neer’s classification, 10 patients had two-part fractures, 21 had three-part fragmentation, and 9 had four-part fragmentation.
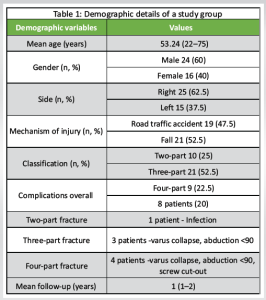
Every patient underwent surgery using the deltopectoral approach. The mean NSA was 138.62° ± 11.09°. The literature indicates that a normal NSA is 135°, with an acceptable varus deviation up to 120° [19]. In this, four had an NSA of ≤120°, with three achieving a fair functional outcome and one achieving a good functional outcome. Two of 29 of those who participated with an NSA >130° and a compressed GT lower the acromion surface (AS) had a fair functional prognosis, most likely based on concurrent rotator cuff and soft tissue injuries. The distance from the higher limit of the GT and the AS was assessed, as this area is critical for shoulder abduction and significantly impacts functional outcomes. In the study, the mean distance from GT to AS was 6 mm ± 1.4 mm. The mean alpha angle was 1.84 ± 0.17, the mean beta angle was 1.15 ± 0.18, and the mean alpha/beta ratio was 1.60 ± 0.19. Among the 40 patients, 5 had an alpha/beta ratio of <1.40 mm but still achieved a good C-M score. However, 2 out of these 5 patients experienced screw cut-outs. The study also measured head diameter and height, which revealed that individuals with outstanding grades had considerably greater head diameters and heights. The mean C-M marks at the half-yearly re-visit were 80.72. Five patients had a C-M score below 60, with 4 of these patients exhibiting varus head position and all 5 having a GT to AS distance of <6 mm. ROM was assessed at final follow-up, with 35 of them (87.5%) achieving abduction more than 90° and 5 patients (12.5%) below 90°. Complications were observed in 8 patients (20%): Varus collapse in 4 patients (10%), abduction <90° in 5 patients (12.5%), infection in 1 patient (2.5%), and screw cut-out in 2 patients (5%).
The primary intention was to examine the relationship between radiographic parameters with functional outcomes. Proximal humeral fractures, known for their complex fracture pathoanatomy, are prevalent and of significant interest in orthopedic practice due to the methods employed to ensure early functional recovery. The reduction and fixation technique, alongside the surgeon’s skill and experience, is crucial. In this investigation, 22 of 40 were below 60 age, with an average age of 53.24 years. In addition, 24 patients were men, who generally have better bone quality. This contrasts with Dheenadhayalan et al.’s [20] study, which had a higher proportion of male patients, whereas other studies often report a larger number of female patients. The NSA, representing the aspect from the diaphyseal to the humeral neck level, has a normal value of about 135°. NSA of 120° or lower increases the probability of varus collapse [19]. In our study, 4 out of 40 patients had an NSA of <120°. Of these, 3 had shoulder abduction lower to 90° and a C-M scoring of 60, representing that deviations from the NSA can impair active outcomes. These findings align with literature describing restricted shoulder mobility, particularly abduction, because of varus deformities of the humerus. In Dheenadhayalan et al.’s [20] study, 14 out of 127 patients had an NSA of <120°, and all of these patients exhibited similar impairments in shoulder abduction and C-M scores. GT to AS was also evaluated, as this distance is crucial for shoulder abduction and functional outcomes. In our study, the mean GT to AS distance was 6 mm ± 1.4 mm. Head diameter, measured within the lower and superior cortices of the articular plane, averaged 44.6 mm, while head height, represented as the space from the head midpoint to the articular cortex, averaged 17.3 mm. Patients with larger head diameters and heights had better C-M scores. Dheenadhayalan et al. [20,21] reported an average GT to AS length of 7.2 mm, noting that higher displacement of GT above AS was linked with shoulder abduction of <90° in patients with such displacements. Robertson et al.’s [22] study of cadaveric humeri found comparable values for head height and gap from the tuberculum and head apex. In our study, the alpha gap was noted within the outer cortices above the deltoid tuberosity, and the beta distance was measured between the inner cortices at the same level. The alpha/beta ratio, an indirect indicator of bone marrow density, was used to predict screw cut-out. The mean alpha distance was 1.84 ± 0.17, the beta distance was 1.15 ± 0.18, and the alpha/beta ratio was 1.60 ± 0.19. Five patients had an alpha/beta ratio of <1.40 but still achieved good C-M scores; however, 2 of these 5 patients experienced screw cut-out. Da Silva et al. [15] found that a deltoid tuberosity index (similar to our alpha/beta ratio) of ≤1.44 was associated with an 8% rate of screw cut-out. In our study, 5 patients had an alpha/beta ratio <1.44, with 2 (40%) experiencing screw cut-out. Recent studies highlight the necessity of supporting the medial column in holding stable fixation of nearby humerus fractures and avoiding varus malunion, plate failure, screw cut-out, and impingement. Proper anatomic reduction and medial calcar restoration provide essential support, increasing load to failure, axial stiffness, and overall stability of the fixation. Gardner et al. [21] first emphasized that mechanical support of the inferomedial area considerably minimizes post-operative fracture subsidence. Medial column support can be achieved through calcar screws or endosteal fibular allograft augmentation. In our study, calcar screws were not applied in 6 patients, of whom 4 experienced varus collapse postoperatively. Dheenadhayalan et al. [20] also observed post-operative varus collapse in 14 patients, all of whom did not receive a calcar screw (Fig. 3).

At the 6-month revisit, the average C-M rating in our study was 80.72. Thirty-two patients (80%) achieved a good to excellent outcome. Five of the participants had a C-M score below 60, with 4 exhibiting varus head position and all having a GT to AS distance of within 6 mm. ROM assessment revealed that 87.5% of patients had shoulder abduction above 90°, while 12.5% had abduction below 90°. Dheenadhayalan et al. [20] reported that 94% had a good to excellent based on the C-M rating. Ahrend et al. have mentioned a mean C-M scoring of 80.2 ± 17. Our findings are consistent with previous studies, including Ockert et al. [23], who found an average C-M score of 75.3 points after a median follow-up of 10 years. This study’s limitations include its retrospective methodology, limited sample size, low follow-up rate, and reliance on X-ray rather than CT imaging, which would provide more comprehensive three-dimensional information on radiographic parameters and prognostic factors for previously mentioned fractures.
This study evaluates the relationship between radiographic parameters and functional outcomes in proximal humeral fractures treated with open reduction and plate fixation. The findings highlight the importance of precise anatomical reduction, particularly the NSA and the distance between the GT and the articular surface (AS), in predicting functional recovery. A normal NSA and an adequate GT to AS distance are associated with improved shoulder abduction and higher C-M scores. Even though 9 patients had Neer’s four part fracture, only 4 patients had fair functional outcome and remaining had good functional recovery. In addition, the alpha/beta ratio, which reflects bone marrow density, was found to influence outcomes, with lower ratios correlating with a higher incidence of screw cut-out. Stabilization of the medial column, achieved through techniques such as calcar screws, was shown to reduce the risk of varus collapse, underscoring its importance in ensuring stable fixation. Although the outcomes were generally positive, complications such as screw cutout and varus collapse remain significant, emphasizing the need for careful surgical technique and diligent post-operative care.
Restoring radiological parameters in proximal humerus fractures with plate fixation is vital for optimal functional outcomes. Accurate anatomical reduction preserves shoulder biomechanics, improving mobility and strength while reducing complications such as malunion, non-union, or stiffness, ensuring better post-operative recovery.
References
- 1.Pencle F, Varacallo M. Proximal humerus fracture. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. [Google Scholar]
- 2.Iglesias-Rodríguez S, Domínguez-Prado DM, García-Reza A, FernándezFernández D, Pérez-Alfonso E, García-Piñeiro J, et al. Epidemiology of proximal humerus fractures. J Orthop Surg Res 2021;16:402. [Google Scholar]
- 3.Carofino BC, Leopold SS. Classifications in brief: The Neer classification for proximal humerus fractures. Clin Orthop Relat Res 2013;471:39-43. [Google Scholar]
- 4.Schumaier A, Grawe B. Proximal Humerus Fractures: Evaluation and Management in the Elderly Patient. Geriatr Orthop Surg Rehabil. 2018 Jan 25;9:2151458517750516. doi: 10.1177/2151458517750516. PMID: 29399372; PMCID: PMC5788098. [Google Scholar]
- 5.Misra S, Vaishya R, Trikha V, Maheshwari J. Practice guidelines for proximal humeral fractures. J Clin Orthop Trauma 2019;10:631-3. Erratum in: J Clin Orthop Trauma 2020;11:1176. Erratum in: J Clin Orthop Trauma 2021;21:101570. [Google Scholar]
- 6.Jung WB, Moon ES, Kim SK, Kovacevic D, Kim MS. Does medial support decrease major complications of unstable proximal humerus fractures treated with locking plate? BMC Musculoskelet Disord 2013;14:102. [Google Scholar]
- 7.Egol KA, Ong CC, Walsh M, Jazrawi LM, Tejwani NC, Zuckerman JD. Early complications in proximal humerus fractures (OTA Types 11) treated with locked plates. J Orthop Trauma 2008;22:159-64. [Google Scholar]
- 8.Neer CS 2nd. Displaced proximal humeral fractures: Part I. Classification and evaluation. By Charles S. Neer, I, 1970. Clin Orthop Relat Res 1987;223:3-10. [Google Scholar]
- 9.Hoppenfeld S, deBoer P, Buckley R. Surgical Exposures in Orthopaedics: The Anatomic Approach. 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2009. [Google Scholar]
- 10.Robinson CM, Murray IR. The extended deltoid-splitting approach to the proximal humerus: Variations and extensions. J Bone Joint Surg Br 2011;93:387-92. [Google Scholar]
- 11.Ziegler P, Kühle L, Stöckle U, Wintermeyer E, Stollhof LE, Ihle C, et al. Evaluation of the constant score: Which is the method to assess the objective strength? BMC Musculoskelet Disord 2019;20:403. [Google Scholar]
- 12.Wang Q, Sheng N, Rui B, Chen Y. The neck-shaft angle is the key factor for the positioning of Calcar screw when treating proximal humeral fractures with a locking plate. Bone Joint J 2020;102:1629-35. [Google Scholar]
- 13.Ahrend MD, Kühle L, Riedmann S, Bahrs SD, Bahrs C, Ziegler P. Radiographic parameter(s) influencing functional outcomes following angular stable plate fixation of proximal humeral fractures. Int Orthop 2021;45:1845-52. [Google Scholar]
- 14.Spross C, Kaestle N, Benninger E, Fornaro J, Erhardt J, Zdravkovic V, et al. Deltoid tuberosity index: A simple radiographic tool to assess local bone quality in proximal humerus fractures. Clin Orthop Relat Res 2015;473:3038-45. [Google Scholar]
- 15.Da Silva T, Ehrhard D, Chuchuy TM, Knop C, Merkle T. Predictive value of the deltoid tuberosity index for assessing the risk of screw cut-out. Obere Extremität 2023;18:106-12. [Google Scholar]
- 16.Sheng N, Shi T, Wang Q, Wang L, Chen Y. Nonanatomic healing of the greater tuberosity after plating in proximal humeral fractures: A case control study. J Orthop Surg Res 2023;18:374. [Google Scholar]
- 17.Yian EH, Ramappa AJ, Arneberg O, Gerber C. The constant score in normal shoulders. J Shoulder Elbow Surg 2005;14:128-33. [Google Scholar]
- 18.Bahrs C, Badke A, Rolauffs B, Weise K, Zipplies S, Dietz K, et al. Long-term results after non-plate head-preserving fixation of proximal humeral fractures. Int Orthop 2010;34:883-9. [Google Scholar]
- 19.Lupescu O, Popescu GI, Nagea M, Ciurea NM, Dimitriu AL, Lupescu D, et al. Morphological landmarks of proximal humerus with impact in post-traumatic outcome. Rom J Morphol Embryol 2016;57:1273-8. [Google Scholar]
- 20.Dheenadhayalan J, Prasad VD, Devendra A, Rajasekaran S. Correlation of radiological parameters to functional outcome in complex proximal humerus fracture fixation: A study of 127 cases. J Orthop Surg (Hong Kong). 2019 May-Aug;27(2):2309499019848166. doi: 10.1177/2309499019848166. PMID: 31104562. [Google Scholar]
- 21.Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma 2007;21:185-91. [Google Scholar]
- 22.Robertson DD, Yuan J, Bigliani LU, Flatow EL, Yamaguchi K. Three-dimensional analysis of the proximal part of the humerus: Relevance to arthroplasty. J Bone Joint Surg Am 2000;82:1594-602. [Google Scholar]
- 23.Ockert B, Siebenburger G, Kettler M, Braunstein V, Mutschler W. Long-term functional outcomes (median 10 years) after locked plating for displaced fractures of the proximal humerus. J Shoulder Elb Surg 2014;23:1223-31 [Google Scholar]