This article underscores the diagnostic and management challenges of metallosis in hip replacements, stressing its importance as a differential diagnosis for post-arthroplasty symptoms, even in metal-on-polyethylene implants
Dr. Sanjay Singh Rawat, Department of Orthopaedics, AIIMS Raebareli, Munshiganj, Raebareli, Uttar Pradesh, India. E-mail: sanjaymamc07@gmail.com
Introduction: Metallosis, characterized by the collection of metallic debris in periarticular tissues, is primarily associated with metal-on-metal bearings in hip arthroplasty. This report presents a rare case of metallosis after metal-on-polyethylene (MoP) total hip arthroplasty (THA), highlighting diagnostic challenges and management strategies. Metallosis following MoP arthroplasty is extremely rare, with only a limited number of documented cases in the literature.
Case Report: A 70-year-old man presented with post-traumatic hip pain and instability 6 years after an uncemented MoP THA. Radiographs revealed a fractured acetabular cup with metal fragments and displacement of the femoral head. A computed tomography scan confirmed liner failure, cup breakage, and radiodense opacities around the joint. Given the post-traumatic presentation and the risk of heterotopic ossification, the patient underwent revision surgery. Revision surgery involved acetabular component exchange, and clinical follow-up indicated satisfactory outcomes.
Conclusion: This case highlights the atypical presentation of metallosis following MoP THA, emphasizing the significance of early diagnosis and awareness for optimal patient outcomes.
Keywords: Metallosis, total hip arthroplasty, revision surgery, bearing surfaces.
Total hip arthroplasty (THA) is a well-accepted surgical intervention for managing end-stage hip disease. While post-operative pain is a known consequence, pinpointing its exact source can be challenging. Post-operative pain in THA can result from infection, implant loosening, dislocation, fractures, heterotopic ossification, nerve injury, or metallosis, necessitating precise diagnosis and management. Periprosthetic fractures are potential post-traumatic complications, with femoral fractures being more prevalent than acetabular fractures [1]. The pursuit to optimize implant longevity and minimize complications has driven the evolution of various bearing surfaces in THA. Specifically, metal-on-metal (MoM) bearings have been linked to complications such as metallosis, resulting in failure and higher revision rates. Due to concerns about MoM bearings, metal-on-polyethylene (MoP) remains the predominant choice for bearing combinations. Adverse reaction to metal debris (ARMD), also known as metallosis, occurs when metal particles (wear debris) from a hip implant cause the surrounding tissues to become fibrotic, necrotic or result in the loosening of the implant [2, 3]. This incident is usually observed in MoM-bearing surfaces. However, in rare instances, MoP bearings could develop metallosis if polyethylene liner wear and tear progress to a point where MoM articulation occurs, leading to the symptoms and characteristic complications associated with ARMD [4]. The present case report describes a patient who experienced post-traumatic damage to the polyethylene liner, resulting in the head (Metal) coming in contact with the acetabular cup and subsequent metallosis.
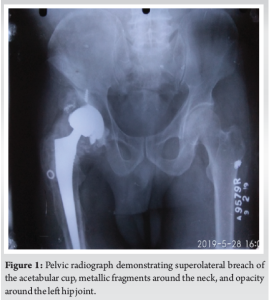
A 70-year-old man with a history of avascular necrosis left hip secondary to a post-traumatic femoral neck fracture, treated with failed cancellous screw fixation, presented 6 years after uncemented MoP THA. He reported progressive worsening of pain over the past 6 months in his left hip, leading to increasing difficulty in ambulation and eventual wheelchair dependence. The pain reportedly worsened following a fall at home 6 months before the presentation. His medical history included hypertension, which was well-managed with medication. Notably, he did not develop any symptoms suggestive of systemic metal poisoning. The patient’s prior THA, performed through a posterior approach, achieved a satisfactory outcome with pain-free ambulation until August 2018 (6 months pre-presentation). Following the fall, he developed progressive discomfort and instability in the hip. On clinical examination, the left hip was unstable with intermittent subluxation, readily reducible with traction, and had a constrained and painful range of motion. The surgical scar appeared well-healed without any erythema, sinus formation, or other concerning skin changes with no local rise in temperature. Standard laboratory tests, including erythrocyte sedimentation rate and C-reactive protein, returned results within normal limits. Pelvic radiographs demonstrated upper and outer migration of the head of the femur and downward displacement of the acetabular cup with metallic fragments (Fig. 1). No evidence of femoral stem loosening was observed. A computed tomography (CT) scan was performed but deemed inconclusive, suggesting liner failure, acetabular cup fracture, and radiodense opacities surrounding the hip joint. Magnetic resonance imaging (MRI) was not obtained due to the non-availability of metal artifact suppression techniques at the institute. The patient was posted for revision surgery based on clinical and radiographic findings. The revision surgery was performed using the posterior approach, just as in the primary surgery.
Intraoperative findings
The surgical field revealed dark metal debris within the soft-tissues, surrounded by a dark blackish fluid collection (Fig. 2, 3, 4). Blackening of surrounding tissues with metallic debris was also noted. The polyethylene liner was fixed within the acetabular cup and showed wear on both the liner and the cup itself. The femoral head was noted to have migrated superior and laterally through a defect in the acetabular cup, coming into contact with the acetabular wall, meanwhile, the acetabular cup component remained secured within the acetabulum. Following thorough debridement and lavage, the pseudo capsule, broken liner, and remaining acetabular cup were removed. The femoral stem demonstrated no signs of loosening or trunnionosis and was retained. Revision surgery involved the placement of a 58 mm titanium alloy Pinnacle revision cup secured with multiple screws (4 peripheral + 3 inner). A ceramic liner (52 mm) and ceramic femoral head (34 mm) were implanted (Fig. 5). Tissue samples were procured and dispatched for histopathological analysis. The surgical wound was meticulously irrigated and closed in layers.


Post-operative course
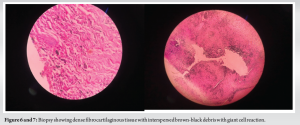
The patient tolerated the surgery well and received post-operative management in the hospital for the next 6 days, including pain control, antibiotics, and physical therapy. Initial serum levels of chromium (3.91 μg/L, within the normal range of 0.70–28 μg/L) and cobalt (<2.5 μg/L, within the normal range of 0.50–3.90 μg/L) measured on post-operative day 1 were within the normal range, effectively excluding systemic cobalt or chromium poisoning. Patient was discharged on post-operative day 6, followed by outpatient suture removal on day 15. Home health therapy for rehabilitation was then initiated. The patient was followed up at 4 and 12 weeks postoperatively for regular examinations. At the 12-week visit, he demonstrated a stable and pain-free gait. The final histopathological examination revealed dense fibrocartilaginous tissue with interspersed brown-black debris and a giant cell reaction consistent with metallosis (Fig. 6 and 7), with no evidence of acute inflammation.
Conventionally, complications of metallosis, corrosion, and pseudotumor formation were primarily observed in MoM bearing surfaces in THA. However, recent evidence suggests that these complications can occur less frequently in MoP bearings [4]. The generation of debris (wear) from the bearing surfaces remains a critical factor limiting long-term implant survival in THA [5]. While wear significantly contributes to MoM THA failure and revision surgery, particularly at the head-neck junction (trunnions), erosion through the polyethylene component and metal acetabular cup in MoP bearings is a much rarer occurrence [6, 7]. This case report and a limited number of others documented in the literature (e.g., Birkett et al. and Delimar et al.) highlight the potential for metallosis to develop even in MoP THA due to extreme wear [8, 9]. Several factors can contribute to polyethylene wear in hip arthroplasty, with patient activity level being a primary determinant. Smaller metal particles released due to wear can disrupt smooth articulation, exacerbate wear rates, and induce an inflammatory cascade within the joint [10]. Metallosis can manifest as implant failure or a foreign body reaction. Plain radiographs often lack sensitivity in detecting metallosis, with characteristic signs such as eccentric femoral head alignment and joint radiolucency (“bubble sign”) being absent in most cases [11, 12]. CT scans can be helpful, revealing dense material surrounding the joint capsule or bursa [12]. However, the gold standard for diagnosing metallosis and assessing its extent is the combination of ultrasound and metal artifact reduction sequence MRI (MARS-MRI), which together has nearly 100% sensitivity [13]. In addition, blood metal ion levels can serve as an indicator for early detection of metallosis following arthroplasty. Literature suggests a threshold of >4.5 ppb (One ppb is equivalent to µg/L) for chromium/cobalt, which should prompt further investigation with MARS-MRI [14]. Regular clinical and radiological monitoring is crucial for detecting potential complications like metallosis. If intraoperative assessment reveals minimal damage to the metal shell, liner replacement might be a viable option. However, extensive metallic wear necessitates a more comprehensive revision surgery. The present case exemplifies the value of regular radiographic follow-up, as the patient showed no symptoms until significant wear developed. If there is suspicion of metallosis, monitoring blood metal ion levels and considering a MARS-MRI scan is recommended [14]. Definitive diagnosis necessitates immediate revision surgery, ideally before severe complications or metal poisoning develop. Although metal-related pathology is a frequent cause for revision after MoM THA, it is crucial to exclude other potential reasons, such as acute dislocation, component loosening, infection, and periprosthetic fracture [2]. In addition, referred pain from the pelvis or spine should be considered as a differential diagnosis. Metal debris is not biologically inactive, and its buildup in synovial tissue can cause chronic inflammation. These particles can also migrate to nearby or distant lymph nodes, often triggering fibrotic and necrotic changes [15]. Phagocytized particles may travel to organs such as the liver, spleen, and lungs; however, the link between metal debris and disease development in these organs is still debated [15].
Heightened awareness is crucial when evaluating patients with persistent pain after THA surgery. Early diagnosis of metallosis can be advantageous, even in atypical presentations and before frank failure or extreme wear patterns develop. MARS-MRI can be a valuable screening method in such cases.
Metallosis is a recognized complication of THA, typically associated with MoM bearing surfaces. This case underscores the significance of considering metallosis as a differential diagnosis for pain and loosening after THA, regardless of the bearing surface used. Local complications can occur even without symptoms and with normal serum levels of heavy metals. Both MARS-MRI and CT scans play a significant role in diagnosing metallosis.
References
- 1.Wood MJ, Al-Jabri T, Zaghloul A, Lanting B, Giannoudis PV, Hart AJ. Periprosthetic acetabular fractures as a complication of total hip arthroplasty. Injury 2023;54:111058. [Google Scholar]
- 2.Drummond J, Tran P, Fary C. Metal-on-metal hip arthroplasty: A review of adverse reactions and patient management. J Funct Biomater 2015;6:486-99. [Google Scholar]
- 3.Langton DJ, Joyce TJ, Jameson SS, Lord J, Van Orsouw M, Holland JP, et al. Adverse reaction to metal debris following hip resurfacing: The influence of component type, orientation and volumetric wear. J Bone Joint Surg Br 2011;93:164-71. [Google Scholar]
- 4.Matharu GS, Pandit HG, Murray DW, Judge A. Adverse reactions to metal debris occur with all types of hip replacement not just metal-on-metal hips: A retrospective observational study of 3340 revisions for adverse reactions to metal debris from the National Joint Registry for England, Wales, Northern Ireland and the isle of man. BMC Musculoskelet Disord 2016;17:495. [Google Scholar]
- 5.Karachalios T, Komnos G, Koutalos A. Total hip arthroplasty: Survival and modes of failure. EFORT Open Rev 2018;3:232-9. [Google Scholar]
- 6.Pastides PS, Dodd MS, Sarraf KM, Willis-Owen C. Trunnionosis: A pain in the neck. World J Orthop 2013;4:161-6. [Google Scholar]
- 7.Shulman RM, Zywiel MG, Gandhi R, Davey JR, Salonen DC. Trunnionosis: The latest culprit in adverse reactions to metal debris following hip arthroplasty. Skeletal Radiol 2014;44:433-40. [Google Scholar]
- 8.Birkett N, El-Daly I, Ibraheim H, Mbubaegbu C. Metallosis following full thickness wear in total hip arthroplasty. J Surg Case Rep 2015;2015:rjv122. [Google Scholar]
- 9.Delimar D, Bohaček I, Dimnjaković D, Viderščak D, Schauperl Z. Femoral head wear and metallosis caused by damaged titanium porous coating after primary metal-on-polyethylene total hip arthroplasty: A case report. Croat Med J 2018;59:253-7. [Google Scholar]
- 10.Schmalzried TP, Shepherd EF, Dorey FJ, Jackson WO, Dela Rosa M, Fa’vae F, et al. The John Charnley Award. Wear is a function of use, not time. Clin Orthop Relat Res 2000;381:36-46. [Google Scholar]
- 11.Su EP, Callander PW, Salvati EA. The bubble sign: A new radiographic sign in total hip arthroplasty. J Arthroplasty 2003;18:110-2. [Google Scholar]
- 12.Oliveira CA, Candelária IS, Oliveira PB, Figueiredo A, Caseiro-Alves F. Metallosis: A diagnosis not only in patients with metal-on-metal prostheses. Eur J Radiol Open 2014;2:3-6. [Google Scholar]
- 13.Matharu GS, Mansour R, Dada O, Ostlere S, Pandit HG, Murray DW. Which imaging modality is most effective for identifying pseudotumours in metal-on-metal hip resurfacings requiring revision: Ultrasound or MARS-MRI or both? Bone Joint J 2016;98-B:40-8. [Google Scholar]
- 14.Sidaginamale RP, Joyce TJ, Lord JK, Jefferson RD, Blain PG, Skinner JA, et al. Blood metal ion testing is an effective screening tool to identify poorly performing metal-on-metal bearing surfaces. Bone Joint Res 2013;2:84-95. [Google Scholar]
- 15.Urban RM, Jacobs JJ, Tomlinson MJ, Gavrilovic J, Black J, Peoc’HM. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am 2000;82:457-76. [Google Scholar]