The acknowledgment of the unusual Jeffery type 2 radial neck fracture, associated with ipsilateral elbow dislocation, is important for its early recognition and open reduction to achieve the optimal outcome
Dr. Ganesh Singh Dharmshaktu, Department of Orthopaedics, Government Medical College, Haldwani, Uttarakhand, India. E-mail: drganeshortho@gmail.com
Introduction: The radial neck fractures in children are uncommon injures and more so in the settings of an associated elbow dislocation. Radial neck fracture, with 90° posterior rotation of the articular surface with respect to its normal axis, is a characteristic feature of rare Jeffery type 2 injury. This injury pattern is reported as sporadic reports or small series in the literature. Most of the reported cases have been managed by operative intervention with either open or percutaneous reduction and K-wire fixation. Despite the fact that isolated radial neck fractures have been managed frequently by the retrograde intra-medullary wire fixation technique as described by Métaizeau, its modified utilization as standalone treatment has rarely been described for Jeffery type 2 injury, to the best knowledge of the authors.
Case Report: We, hereby report our experience of a displaced Jeffery type 2 radial neck fracture, associated with the posterior elbow subluxation in a 13-year-old male. The injury was finally treated with open relocation of the displaced radial head to the radius neck followed by retrograde fixation of the radial head with one retrograde intramedullary K-wire as a modified Métaizeau technique. Gradual healing of the fracture, stable elbow, and painless activities of daily living were noted along with normal regain of pre-injury elbow function. No complication or instability was noted and excellent Mayo Elbow performance score in the follow-up of 13 months.
Conclusion: The peculiar injury pattern of Jeffery type 2 radial neck fracture warrants early recognition and appropriate management for the optimal functional outcome and also to avoid complication. Open reduction of the displaced radial head and fixation with Métaizeau technique is viable option for the management of this rare injury.
Keywords: Elbow injury, pediatric elbow, pediatric fracture, radial neck fracture, elbow dislocation.
Pediatric radial neck fractures are uncommon injuries and reported to occur in approximately 5–8.5% of pediatric elbow fractures [1]. Jeffrey type 2 fractures, a rare variant, that often result from relocation attempts of posterior elbow subluxation or dislocation, were described by Jeffery in 1950. There is rotation of the epiphysis, 90° posteriorly and is supposed to result while trying to reduce the elbow subluxation/dislocation. The capitellum, striking the anterior radial head edge, may result in this characteristic rotational deformity. The mechanism, as rightly described by Jeffrey, mimics that of a bottle opener [2]. These are reported as sporadic cases or small series in the literature and mainly are managed by operative fixation [3]. Closed manipulation attempts to reduce radial neck are reported to even complicate things by producing an “upside-down” radial head deformity [4]. There are reports of complete inversion with 180° rotation following closed reduction attempts, necessitating an open reduction later [5]. Successful closed reduction, however, has been reported but risk of epiphysiolysis and subsequent elbow valgus deformity persists [6]. Open reduction, however, achieves reduction under direct vision, which can then be stabilized usually with implants like K-wires. After the reduction of the radial head, the fixation can be done in standard manner with one of many described methods of fixation of radial neck fracture (Table 1).
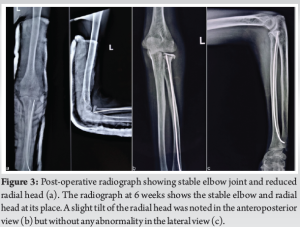
A 13-year-old male child presented to us with a history of the injury to his left elbow, following an inadvertent fall from tree, leading to acute painful restriction of the elbow movement. There was resultant acute pain and swelling and he could only carry the extremity while supported by the contralateral upper extremity. On clinical examination, there was swelling with active and passive painful restriction of the elbow movement. There was, however, no other injury or any distal neuromuscular deficit. The radiograph revealed posterior elbow subluxation along with the fracture of the radial neck. The radial neck fracture was displaced and appeared to be lodged near the elbow joint (Fig. 1a). The radial head epiphysis was found to be posteriorly displaced and perpendicular to the normal radial axis. An attempt of close reduction in the emergency room was done but elbow could not be properly reduced. Radiographs revealed non-concentric elbow joint and displaced radial neck fracture (Fig. 1b). Following the failed closed reduction attempt, reduction under anesthesia was planned (Fig. 2a). The elbow was comfortably reduced under anesthesia and the reduction was confirmed on fluoroscopy for concentricity and stability. The radial neck was lying and palpable at the lateral aspect of the elbow and direct incision over the palpable mass led to the isolation of the radial head (Fig. 2b). The incision was extended and the radial head was placed well at its native position. To add to the stability of the radial head at its position, retrograde intra-medullary wire was introduced through the distal radial metaphysis like the technique described by Métaizeau (Fig. 2c). The technique of intra-medullary fixation as described by the Métaizeau is a well described method for fixing pediatric radial neck fracture and was modified here as we reduced the fracture by open means. The wire was targeted to pierce and engage into the radial head but only the tip of the wire could be engaged in the head (Fig. 2d). The annular ligament was repaired and the wound was closed in layers. A protection plaster slab in forearm supination was given for 3 weeks and active shoulder and finger movement were encouraged all through the treatment (Fig. 3a). No re-displacement of elbow and gradual healing of the radial neck fracture were noted in the follow-up and at the end of 8 weeks, the fracture was united (Fig. 3b and c). The active elbow movement was advised from 8th weeks onward, leading to the regain of full range of motion. The fracture was fully consolidated by 13 months (Fig. 4) and though there was, however, mild deformity of the radial head noted but without any corresponding clinical complaint or instability. The Mayo Elbow performance score, as noted in the final follow-up, was 92 (excellent 90–100). Painless activities of daily living were noted in the follow-up of 13 months.


Jeffery type 2 fracture often results following the closed reduction of posterior elbow dislocation as the capitellum hinges on the anterior radial head leading to 90° of backward tilt [7]. Other than that, the Jeffery classification describes a total of 3 types based on the displacement of the radial head epiphysis and type 1 is not displaced with minimal soft tissue interposition and type 3 is anterior displacement of radial head produced during the posterior elbow dislocation. Another classification by Métaizeau is also described and is based on angle of translation of radial head epiphysis. Grade 1 has translation of <3 mm and epiphyseal tilt is <20°, type 2 has tilt between 20 and 45°, type 3 has tilt 45–80°, and type 4 has more than 80° tilt [8]. The acknowledgment of this potential complication is advocated for better decision-making as we may miss these injuries on casual radiological assessment, especially on bad-quality images [9]. Emergent open reaction has been advised for successful fixation and to avoid complications. Radial neck fracture in the setting of elbow dislocation is rare injury [1, 4, 7, 9]. In our case, there was elbow subluxation. The management in Jeffery type 2 fractures with rotated articular surface usually requires open reduction and fixation by various methods. Métaizeau popularized the technique of retrograde intra-medullary wire fixation technique for conventional radial neck fractures [9]. There are other methods such as percutaneous pinning or elastic stable intra-medullary nailing (ESIN) and both have found comparably good outcomes. Elbow range of motion may, however, be better in ESIN group [10, 11]. Modification of wire fixation techniques has been described like a two K-wire technique in which, one K-wire works as fulcrum while inserted at fracture site and the other wire pushes the radial head to its anatomical position [12]. Another percutaneous reduction technique used successfully in two cases was described as push-back procedure, to suppress the capitellum interposition between the head fragment and the metaphysis by reproducing the reversed trajectory to the trauma [13]. Recently, arthroscopic assisted reduction and fixation have also been reported as an alternative option [14]. Finally, in few cases, radial head excision can be last resort, especially in complex cases [15]. As many of these techniques are described for closed reduction, but as we had to open the site for radial head extraction none of these were attempted. We could find only one case similar to ours, with Jeffery type 2 injury as a result of elbow subluxation that was spontaneously reduced [16]. The radial neck was openly reduced and fixed with pinning with Métaizeau technique followed by a plaster slab. The management was similar to us but the delayed union of the radial neck fracture was noted in that case at the end of 4 months. Repeat surgery with cleaning of fibrous adhesions and fixation with mini-screws was done leading to the final union and good functional outcome. Stable fixation with mini-screw, avoiding the distraction, and minimal damage to osteochondral and ligamentous soft tissues were proposed factors favoring good outcome. Fortunately, in our case, despite poor fixation, good union was noted. The guarded prognosis was explained by us to parents but good repair of soft tissues and annular ligament may have contributed to the good results in our case. As there is potential for missing these injuries in casual observation, attempt should be made to carefully evaluate for proximal radius anatomy in all cases with elbow subluxation or dislocation. Besides it, the closed reduction should be attempted in the light of potential complication of further displacement of radial neck fracture. Prior information to the patient and relatives may help avoid unnecessary conflicts. Open reduction may be warranted for anatomical reduction and to avoid late complications.
The Jeffery type 2 radial neck fracture is uncommon injury that may lead to complications such as restriction of movement and deformities. Its occurrence with elbow dislocation requires appropriate management following the joint reduction. The injury often requires open reduction and fixation and the popular method like Métaizeau technique may be a good treatment option.
The Jeffery type 2 radial neck fracture is unusual associated injury in the settings of pediatric elbow dislocation. The early diagnosis by careful evaluation of the radiographs and open reduction to ensure the anatomical replacement of the radial head ensures favorable results. The use of retrograde intramedullary wiring by the Métaizeau technique can be useful technique. Despite flimsy fixation, results may be good when good set tissue and annular ligament repair is coupled with complaint treatment.
References
- 1.Jeffery CC. Fractures of the head of the radius in children. J Bone Joint Surg Br 1950;32-B:314-24. [Google Scholar]
- 2.Tupe R, Desai S, Tomer D, Patil N. Management and outcome of Jeffery type 2 fractures in paediatric patients: A case series and review of literature. J Orthop Case Rep 2023;13:34-8. [Google Scholar]
- 3.Chotel F, Vallese P, Parot R, Laville JM, Hodgkinson I, Muller C, et al. Complete dislocation of the radial head following fracture of the radial neck in children: The Jeffery type II lesion. J Pediatr Orthop B 2004;13940:268-74. [Google Scholar]
- 4.São Simão R, Monteiro M, Dopico C, Pinto R, Cabral AT. Upside-down radial head: A rare complication after an unrecognised Jeffery Type 2 lesion. J Orthop Trauma 2010;24:e17-20. [Google Scholar]
- 5.Sirois ZJ, Kreul SM, Shank CF. Inadvertent radial head inversion during closed reduction of a pediatric radial neck fracture. J Am Acad Orthop Surg 2019;27:e414-7. [Google Scholar]
- 6.Papaioannou I, Tagaris G, Baikousis A, Christodoulou G, Korovessis P. Successful closed reduction of a Jeffery type 2 radial head epiphysiolysis- A case report with literature review. J Orthop Case Rep 2019;9:22-5. [Google Scholar]
- 7.Kraft DB, Sheppard ED. Radial head incarceration after closed reduction of a pediatric elbow dislocation with a radial neck fracture: A case report. J Am Acad Orthop Surg Glob Res Rev 2022;6:e21.00319. [Google Scholar]
- 8.Métaizeau JP, Lascombe P, Lemelle JL, Finlayson D, Prevot J. Reduction and fixation of displaced radial neck factures by closed intramedullary pinning. J Pediatr Orthop 1993;13:355-60. [Google Scholar]
- 9.Kherbeck T, Gillani S, Ali AM. Reversed reduction of radial neck fractures; a predictable complication of closed manipulation. Injury Extra 2006;37:116-9. [Google Scholar]
- 10.Métaizeau JP. Reduction and osteosynthesis of radial neck fractures in children by centromedullary pinning. Injury 2005;36:A75-7. [Google Scholar]
- 11.Tarallo L, Mugnai R, Fiacchi F, Capra F, Catani F. Management of displaced radial neck fractures in children: Percutaneous pinning vs. elastic stable intramedullary nailing. J Orthop Trauma 2013;14:291-7. [Google Scholar]
- 12.de Oliveira RK, Aita M, Brunelli JF, Ribak S, Serrano PD. Jeffery Type II fracture of the radial neck of a child: Description of the lesion and novel method of closed reduction. Tech Should Elbow Surg 2020;21:124-31. [Google Scholar]
- 13.Chotel F, Sailhan F, Martin JN, Filipe G, Pem R, Garnier E, et al. A specific closed percutaneous technique for reduction of Jeffery type II lesion. J Pediatr Orthop B 2006;15:376-8. [Google Scholar]
- 14.Colozza A, Padovani S, Caruso G, Cavaciocchi M, Massari L. Arthroscopically-assisted reduction and pinning of a radial neck fracture in a child: A case report and review of the literature. J Med Case Rep 2020;14:78. [Google Scholar]
- 15.Tay D, Mahadev A. An unexpected outcome following radial head excision for Jeffrey type II fracture-dislocation of the proximal radius in a child. Ann Acad Med Singapore 2010;39:742-3. [Google Scholar]
- 16.Corominas-Frances L, Fernandez-Lavilla J, Sanpera-Trigueros I. Fracture of the radial neck following elbow subluxation in children. Jeffery type II lesion. A new concept of fixation. Ann Mediterr Surg 2019;2:10-4. [Google Scholar]










