This article highlights the versatility of dual mobility cups in managing extreme situations of failure of Primary Hip Arthroplasty.
Dr. Urvil Shah, Department of Orthopaedics, Seth GS Medical College and KEM Hospital, Mumbai, Maharashtra, India. E-mail: urvil97@gmail.com
Introduction: Dual mobility (DM) total hip replacement (THR) features an acetabular component with an unconstrained tripolar build which ensures a greater range of motion without provoking any dislocation. We report three cases with extremes of surgical misadventure where we carried out a revision arthroplasty with a DM cup. The causes of the failure of the primary arthroplasty were multifactorial, even individually, and ranged from instability due to component malposition, trochanteric fracture, intrapelvic prosthesis protrusion, etc.
Case Report: (1) Case 1 is a 40-year-old male, who following a failed fixation of a right proximal femur shaft fracture had undergone a proximal femur replacement outside with a proximal femur bipolar prosthesis and presented with a dislocated prosthesis due to excessive anteversion of 40 degree of the stem. Revision was done by inserting a DM cup without revising the stem to preserve the valuable femoral bone stock. (2) Case 2 is an 84-year-old comorbid female, who had come with right protrusio acetabuli with bipolar prosthesis in situ. The patient was managed with bone grafting and insertion of a DM cup with a peripheral fit. Greater trochanter wiring was done for the greater trochanter fracture (GTF) along with prophylactic posterior column plating. (3) Case 3 is a 60-year-old male, who had left sided chronic THR instability. He has had three previous episodes of dislocation which started after 7 years, when the patient fell and had a GTF. Here, the causes of instability were multifactorial- GTF, malposition, and liner wear. Instead of using a constrained liner and predisposing the patient to impingement, we did an isolated revision with a DM cup only.
Conclusion: The presented cases highlight the versatility and efficacy of utilizing a DM cup in revision arthroplasty for addressing diverse causes of primary hip arthroplasty failure. The adaptability is demonstrated in preserving the bone stock, managing bone loss, and addressing multifactorial instability, thereby emphasizing its widespread potential.
Keywords: Dual mobility, revision total hip replacement, instability, protrusio, component malposition.
Dual mobility (DM) total hip replacement (THR) features an acetabular component with an unconstrained tripolar design. This design consists of two articulating surfaces: The traditional ball-and-socket design and an additional smaller, mobile bearing within the cup. A greater range of hip motion without provoking any dislocation is possible with the DM cup [1-3]. Due to its inherently stable design, DM is used in patients in whom a higher risk of prosthesis dislocation is anticipated by hip surgeons during Primary THR (P-THR), such as patients aged 75 years or older; American Society of Anesthesiologists (ASA) grade >3; pre-operative diagnosis of neuromuscular disease; and body mass index (BMI) of 30 kg/m2 or greater [4]. Surgical-related risk factors for an increased risk of dislocation include the posterior surgical approach, inadequate capsular repair, component malposition, smaller femoral head size, smaller head/neck ratio, and a less experienced surgeon [4]. Instability is reported as the second (14%) most common cause for failure of P-THR needing revision THR [5]. Even in these cases, DM has demonstrated its efficacy while managing failed P-THRs with a 3% mean dislocation rate observed with the revision DM THR group[5]. We report three cases with extremes of surgical error where we carried out a revision arthroplasty with a third-generation DM cup. The causes of the failure of the primary arthroplasty were multifactorial, even individually, and ranged from instability due to component malposition and/or trochanteric fracture, advanced intrapelvic protrusio acetabuli. We were able to get away by retaining the primary stem in 2/3 cases and in the third case due to the complete absence of acetabulum floor, the peripheral hold of DM design was put to test. To attain acceptable outcomes while revising extremes of these surgical mishaps with DM acetabular cups without any stem exchange, we will not only test the limits of DM design but also preserve the femoral bone stock. All the surgeries were performed by a senior arthroplasty and pelvi-acetabular surgeon with more than 20 years of exp. In all cases, infection was ruled out by yielding negative microbial growth on cultures obtained from pre-operative hip aspirate and intraoperative samples. We were able to achieve adequate functional and radiological outcomes in all cases with full weight-bearing mobilization being possible immediately postoperatively and in subsequent follow-up of >6 months.
Case 1
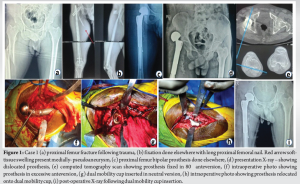
Having suffered a road traffic accident 3 months back, a 40-year-old male had undergone fixation with a long proximal femoral nail for proximal femur shaft fracture, elsewhere. Available notes were suggestive of the patient developing a pseudoaneurysm arising from the superficial femoral artery (SFA) postoperatively. The patient again underwent a cemented proximal femur bipolar hemiarthroplasty 2 weeks before presenting to us, probably for the surgical failure of previous fixation without any intervention being done for pseudoaneurysm. On examination, positive findings included an observable swelling with wound on the medial aspect of the thigh, with externally rotated limb. X-ray revealed a dislocated prosthesis. Initial management consisted of CVTS intervention where management of the pseudoaneurysm was done with excision and rent repair for SFA. Open relocation of dislocated prosthesis was not attempted in the same sitting. One month later, the patient underwent open relocation of dislocated bipolar prosthesis with absorbable antibiotic eluting calcium sulfate granules (STIMULAN) insertion and skin grafting for the well-granulated medial wound. Femoral stem though fixed in excessive anteversion was not found to be loose. After 3 months of antibiotic therapy, the patient underwent the removal of the existing bipolar head and insertion of a new head (PLUSFIT METAL HEAD 28mm) and DM acetabular cup with liner (SHARMA SURGICALS 48 mm) without revising the stem. Implant was found to be stable intraoperatively. Postoperatively, the patient was given a derotation cast for 2 weeks (Fig. 1).
Case 2
An 84-year-old female who had undergone a cemented bipolar hemiarthroplasty 12 years back for right-sided transcervical neck of femur fracture presented with inability to bear weight on the right hip for a month. X-ray imaging revealed protrusio acetabuli with the intrapelvic migration of hemiarthroplasty. A fracture involving greater trochanter with deficient cement mantle in Gruen Zone 6 and 7 was also noted [6]. Patient was managed with implant removal followed by Hybrid DM THR with bone graft substitutes, wiring for greater trochanter, and prophylactic posterior column plating of acetabulum. The greater trochanteric fracture acted like a flip osteotomy, and dislocation of bipolar head and stem was possible, followed by its removal. Paprosky Type IIc acetabular bone loss was present, consisting of a medial defect with bipolar head medial to Kohler’s Line (Protrusio) [7]. The acetabulum floor was deficient and was covered only by a membrane. Hence, peripheral fit of the cup was possible intraoperatively, which was achieved via the spikes on the DM cup. A prophylactic posterior column plating was also done (Fig. 2).
Case 3
A 60-year-old male who had undergone THR for left-sided avascular necrosis of femur head, 8 years back, presented with a history of three prosthesis dislocation episodes in the last 4 months. The first episode was managed with open relocation with trochanteric wiring (for associated greater trochanter fracture- GTF) and the second was managed with closed reduction. The radiograph at the time of presentation to us was suggestive of posterior dislocation of the prosthesis, which was multifactorial due to cup malposition, polywear (intraoperative finding), and GTF. CT scan revealed cup in 5° of retroversion and stem in 46° of anteversion with a combined anteversion of 41°. Revision of the acetabulum cup and liner with a DM cup and liner was performed with correction of the cup version (placed in 15° of anteversion), on the existing femur head and stem with additional trochanteric wiring. No further instability/dislocation episode has been documented since surgery (8 months post-operative) and the patient mobilizes comfortably (Fig. 3).
Gilles Bousquet and André Rambert initially brought the concept of a design characterized by two distinct articulations in THA (France, 1974) as an attempt to diminish the risk of dislocation [1-3]. The implant consists of a porous-coated metal shell with a polished interior that accepts a large polyethylene ball into which a smaller metal or ceramic head is inserted [1]. The two areas of articulation share the same motion center [1]. The design effectively increases the head size and the head-neck ratio of the construct [8]. Initial motion occurs between the femoral head and the inner concave surface of the PE bearing and a secondary motion between the PE bearing and the acetabular cup when a larger range of motion is required (when the femoral head impinges on the liner’s rim) [8,9]. Therefore, the second articulation between the liner and the cup increases the jump distance. All these factors increase the range of motion [9,10], reduce the implant impingement and improve the stability [1, 11, 12]. In Case 1, the patient had a failure of his proximal femur bipolar hemiarthroplasty – cause being instability due to malposition and he fell into the Type IV category of classification of failure of hip hemiarthroplasty [13] for which the surgical strategy entailed a comprehensive approach, involving the complete removal of both the implant (stem and head) and the extraction of cement, extending to the distal metaphysis [13]. The subsequent plan involved the insertion of a new proximal femur prosthesis and acetabular cup. Notably, the initial prosthetic fixation in the proximal femur demonstrated no indications of radiological or intraoperative loosening. However, opting for implant and cement removal would have mandated an extended trochanteric osteotomy, carrying inherent risks such as prolonged surgical duration, an elevated likelihood of prosthetic fracture, bone loss, infection, and an increased probability of future implant loosening, potentially requiring re-revision surgery. Considering the patient’s age in their fourth decade and the established stability of the existing implant, our decision was to replace solely the femur head and utilize a DM cup. This strategic choice aimed at preserving valuable bone stock, mitigating the challenges associated with an extensive and arduous surgery, and postponing the necessity for stem revision. While our thorough literature review uncovered instances of revision surgeries employing a DM cup in isolation, notably absent were articles detailing the isolated insertion of a DM cup without concurrent femur stem revision in cases of femoral component malposition [14]. In a retrospective study by Carulli et al. where in DM cups were used for the management of recurrent dislocations of hip hemiarthroplasty with a mean follow-up of 3.8 years, there were no dislocations and the mean Harris Hip Score improved from 62.2 to 76 [15]. In this same study, the one case where in the cause of dislocation was found to be wrong version of the cemented stem, it was managed by revising not only the cup but also the stem [15]. In Case 2, the cause of the failure of the bipolar prosthesis was the protrusio, and the GTF occurring due to the protrusio. This falls into Category IB of the classification of Failure of Hip Hemiarthroplasty [13]. In this case, the alternative surgery would have been to do an implant removal, followed by revision surgery using a jumbo cup/cage/augment/standard cup with screws and bone grafting on the acetabular side [7]. However, in this case, considering the high-risk factors- age of 84 years, the patient having hiatal hernia with lung compression, ASA Grade 3, we went ahead with an implant removal followed by doing the revision with a DM cup and new stem and using bone substitutes. We combined this with a prophylactic posterior column plating and greater trochanter wiring for the GTF. A peripheral fit of the DM cup was achieved due to the peripheral spikes present on the outer aspect of the cup. Stability was confirmed intraoperatively. Considering the high-risk nature of this patient (ASA grade 3), this surgical plan ensured a shorter surgical duration and achieved a good outcome postoperatively with the patient being able to mobilize postoperatively after being bedridden for a month. In Case 3, the patient had three episodes of dislocation in short intervals, 7 years after the index surgery. Hence, this patient was a case of a chronic total hip instability. The cause of the dislocation was multifactorial – Cup malposition (5° of retroversion- Type 1), stem malposition (46° anteversion- type 2) (combined anteversion of 41°), GTF (abductor weakness- type 3), liner wear (type 5) and loss of mobility at the lumbosacral spine (impingement- type 4) [16]. However, the primary cause most likely is abductor-trochanter insufficiency as the dislocations occurred following the GTF due to the fall [16]. Since the cause of the instability is multifactorial, all the causes have to be addressed and an alternate surgical plan would be to revise the acetabular cup, head, and stem, use a constraint liner (for the abductor weakness), and to do greater trochanter wiring [16,17]. However, since the stem was well fixed, revision surgery was done with a DM acetabular cup inserted in a neutral version with its liner and using the same head and stem. Followed by this, greater trochanter wiring was done. By correcting the version and inserting a new DM cup, stability was increased multifold, and the patient now had a painless hip. We were able to preserve the femoral bone stock, reduce the chance of prosthetic fractures, and reduce the duration of surgery. Normally, abductor insufficiency constraint liner is indicated [16,17]. Abductor trochanteric insufficiency is the most difficult to treat and has a failure rate of as high as 22% [16]. When the abductor-trochanteric complex is deficient, large femoral heads may not be effective, and the use of a constrained liner is generally recommended; however, even when a constrained liner was used, a high rate of failure was observed particularly if a locking ring-type constrained liner was implemented [16]. In the systematic review by Jones, they found a failure rate of >10% observed to occur at <5 years on using constrained acetabular liners [18]. In the prospective study by Ozden et al., where in revision was done with DM cups for patients having abductor-trochanter insufficiency – the mean duration of follow-up was 38.1 months (range 24–98 months), and there were no dislocations [19]. At the last follow-up, the mean Harris Hip Score increased from 42 points preoperatively to 86 points. The cumulative survival rate of the dual-mobility cup system was 93% (95% confidence interval 88–98.7%) at 5 years [19]. Paderni et al. reported a cup survival rate of 99.2% at 5 years [20]. Prudhon et al. report a DM cup survival of 95% at 10 years [21]. Schmidt et al. found a lower rate of dislocation with the use of a DM cup in revision THA compared to a standard metal cup (3.8% vs. 13.5%) [1]. Their study also demonstrated no significant re-revision risk between DMC and SMC for any reason [1]. In the meta-analysis and systemic review by Giacomo et al., the use of a DM cup for revision total hip arthroplasty (independently of indications) seems to be able to decrease the risk of implant failure at mid-term follow-up, reducing at the same time early post-operative dislocation rates and THA re-revision rates when comparing to results obtained with standard fixed bearing cups [3]. There is no significant level of evidence that the use of DM increases the risk of infection compared with FB [3]. FB implants have a higher risk rate of aseptic loosening at mid-term follow-up [3]. The retrospective cohort study by Van Heumen et al. with a median follow-up of 29 months, found that none of the 50 hips included in their study had dislocated at 1–5 years and had favorable implant survival at 59 months [14]. In the retrospective review by Jones et al. where in DM THA was done in patients who are at a higher risk of dislocation, it was found that only one hip had a traumatic dislocation, while no dislocation was seen in the other hips [4]. Categorization of patients as high risk for dislocation was made according to the presence of one or more of the following patient-related risk factors: an age of 75 years or older, female aged 70 years or older, prior surgery, ASA grade >3, pre-operative diagnosis, neuromuscular disease, and BMI of 30 kg/m2 or greater [4]. In the recent past, several authors described the most significant disadvantages of DM. These were thought to be: Intraprosthetic dislocation and aseptic loosening caused by poly-ethylene (PE) wear increment [4]. However, more recent designs utilizing highly cross-linked polyethylene, sub-hemispherical shells, and optimized head/neck ratios appear to have largely eliminated this issue [4,22]. The mean rate of intraprosthetic dislocation was 0.7% in primary and 1.3% in revision THAs [23].
The use of DM cups in revision arthroplasty emerges as a versatile and effective strategy for addressing diverse causes of primary hip arthroplasty failure. The presented cases demonstrate successful outcomes, showcasing the adaptability of this approach in preserving bone stock, managing bone loss, and addressing multifactorial instability. The consistent improvements in functional and radiological parameters highlight the reliability and promise of pushing DM technology to its limits, emphasizing its potential to optimize patient outcomes in complex scenarios of hip arthroplasty failure.
DM cups offer a robust solution for complex hip arthroplasty failures by providing stability, preserving bone stock, shorter surgical durations in revision scenarios, and facilitating full weight-bearing mobilization. This approach should especially be considered for patients with multifactorial instability, protrusio, component malposition, and other challenging conditions following primary hip arthroplasty failure.
References
- 1.Schmidt A, Batailler C, Fary C, Servien E, Lustig S. Dual mobility cups in revision total hip arthroplasty: Efficient strategy to decrease dislocation risk. J Arthroplasty 2020;35:500-7. [Google Scholar]
- 2.Noyer D, Caton JH. Once upon a time.... Dual mobility: History. Int Orthop 2017;41:611-8. [Google Scholar]
- 3.Giacomo P, Giulia B, Valerio P, Vincenzo S, Pierluigi A. Dual mobility for total hip arthroplasty revision surgery: A systematic review and metanalysis. SICOT J 2021;7:18. [Google Scholar]
- 4.Jones CW, De Martino I, D’Apolito R, Nocon AA, Sculco PK, Sculco TP. The use of dual-mobility bearings in patients at high risk of dislocation. Bone Jt J 2019;101-B(1_Supple_A):41-5. [Google Scholar]
- 5.Oltean-Dan D, Apostu D, Tomoaia G, Kerekes K, Păiuşan MG, Bardas CA, et al. Causes of revision after total hip arthroplasty in an orthopedics and traumatology regional center. Med Pharm Rep 2022;95:179-84. [Google Scholar]
- 6.Schuroff AA, Deeke M, Pedroni MA, Lupselo FS, Kunz RE, Lima AM. Radiographic evaluation of cementation technique using polished, conical, triple-tapered femoral stem in hip arthroplasty. Rev Bras Ortop 2017;52(Suppl 1):40-5. [Google Scholar]
- 7.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty 1994;9:33-44. [Google Scholar]
- 8.De Martino I, Triantafyllopoulos GK, Sculco PK, Sculco TP. Dual mobility cups in total hip arthroplasty. World J Orthop 2014;5:180-7. [Google Scholar]
- 9.Takahashi D, Shimizu T, Miyazaki T, Ogawa T, Iwasaki N. Instability in total hip arthroplasty: A literature review. J Jt Surg Res 2023;1:92-6. [Google Scholar]
- 10.Guyen O, Chen QS, Bejui-Hugues J, Berry DJ, An KN. Unconstrained tripolar hip implants: Effect on hip stability. Clin Orthop 2007;455:202-8. [Google Scholar]
- 11.Romagnoli M, Grassi A, Costa GG, Lazaro LE, Lo Presti M, Zaffagnini S. The efficacy of dual-mobility cup in preventing dislocation after total hip arthroplasty: A systematic review and meta-analysis of comparative studies. Int Orthop 2019;43:1071-82. [Google Scholar]
- 12.Batailler C, Fary C, Verdier R, Aslanian T, Caton J, Lustig S. The evolution of outcomes and indications for the dual-mobility cup: A systematic review. Int Orthop 2017;41:645-59. [Google Scholar]
- 13.Morsi E, Habib ME, Elseedy A, Eid T. Revision of failed hip hemiarthroplasty. Classification, management, and follow-up. J Orthop 2016;13:63-8. [Google Scholar]
- 14.Van Heumen M, Heesterbeek PJ, Swierstra BA, Van Hellemondt GG, Goosen JH. Dual mobility acetabular component in revision total hip arthroplasty for persistent dislocation: No dislocations in 50 hips after 1-5 years. J Orthop Traumatol 2015;16:15-20. [Google Scholar]
- 15.Carulli C, Macera A, Matassi F, Civinini R, Innocenti M. The use of a dual mobility cup in the management of recurrent dislocations of hip hemiarthroplasty. J Orthop Traumatol 2016;17:131-6. [Google Scholar]
- 16.Wera GD, Ting NT, Moric M, Paprosky WG, Sporer SM, Della Valle GJ. Classification and management of the unstable total hip arthroplasty. J Arthroplasty 2012;27:710-5. [Google Scholar]
- 17.Sheth NP, Melnic CM, Paprosky WG. Evaluation and management of chronic total hip instability. Bone Jt J 2016;98-B(1 Suppl A):44-9. [Google Scholar]
- 18.Jones SA. Constrained acetabular liners. J Arthroplasty 2018;33:1331-6. [Google Scholar]
- 19.Ozden VE, Dikmen G, Beksac B, Tozun R. Dual-mobility bearings for patients with abductor-trochanteric complex insufficiency. Hip Int 2018;28:491-7. [Google Scholar]
- 20.Paderni S, Pari C, Raggini F, Busatto C, Delmastro E, Belluati A. Third generation Dual Mobility Cups: Could be the future in total hip arthroplasty? A five-year experience with dualis. Acta Biomed 2021;92(Suppl 3):e2021553. [Google Scholar]
- 21.Prudhon JL, Ferreira A, Verdier R. Dual mobility cup: Dislocation rate and survivorship at ten years of follow-up. Int Orthop 2013;37:2345-50. [Google Scholar]
- 22.Abdel MP. Dual-mobility constructs in revision total hip arthroplasties. J Arthroplasty 2018;33:1328-30. [Google Scholar]
- 23.De Martino I, D’Apolito R, Soranoglou VG, Poultsides LA, Sculco PK, Sculco TP. Dislocation following total hip arthroplasty using dual mobility acetabular components: A systematic review. Bone Jt J 2017;99-B(A Suppl 1):18-24. [Google Scholar]