Bisphosphonates which are used in patients with osteogenesis imperfecta to decrease the incidence of fractures can cause delay in healing and healing without exuberant callus in non-unions and osteotomies done for deformity corrections.
Dr. M L V Sai Krishna, Consultant, Department of Orthopaedics, KIMS-Sikhara Hospital, Guntur, Andhra Pradesh, India. E-mail: krishna.mlv.sai@gmail.com
Introduction: Bisphosphonates have become the standard drugs for the medical management of patients with moderate-to-severe forms of osteogenesis imperfecta (OI). This study was undertaken to study the effect of parenteral pamidronate or oral alendronate therapy, on bone healing after osteotomies in patients with moderately severe forms (Sillence type 4) of OI. .
Materials and Methods: We retrospectively evaluated the effects of bisphosphonate therapy on the healing of seven osteotomies in five patients of OI (Sillence type 4) who underwent Sofield Millar procedure for deformity correction and non-union of long bone fractures.
Results: The patients were evaluated clinically and radiologically for the time taken for osteotomy healing and the radiological pattern of osteotomy healing. The minimum clinico-radiological follow-up period was 2 years and the mean follow-up period was 3.9 years (range 2–7 years). The mean time taken for the osteotomy to heal in the patients receiving bisphosphonates was 10.4 months (range 8–12 months) and the union was achieved without the typical exuberant callus formation. Periosteal new bone formation was uniquely absent.
Conclusion: We infer from our findings that bisphosphonate therapy in OI patients is associated with a different pattern of osteotomy healing and delay in healing of osteotomy.
Keywords: Osteogenesis imperfecta, osteotomy, bisphosphonates, callus
Osteogenesis imperfecta (OI) is a heritable disorder caused by mutations in type 1 collagen, the principal form of collagen in bone, tendon, skin, dentin, and sclera. It is clinically characterized by abnormally weak bones, fragility fractures, and bowing of long bones due to a combination of stress on the weak bones and malunion of the fractures. Extraskeletal manifestations include bluish sclera due to thinning of the sclera, dental abnormalities, hearing loss, and lax skin. The management of patients with OI aims at reducing the frequency of fractures by increasing the bone mineral density, and improving the alignment of the long bones, thereby improving mobility and quality of life. Bisphosphonates particularly pamidronate and alendronate have been proven to be efficacious in improving bone density, relieving chronic bone pain, reducing fracture frequency, and improving the overall growth rate [1-5]. Bone healing following fracture or osteotomy is brought about by the combination of osteoclastic and osteoblastic activity. Theoretically, bisphosphonates by inhibiting the osteoclastic activity can disrupt this well-orchestrated bone remodeling mechanism and thereby lead to a delay in union at the fracture/osteotomy site. However, most reports regarding the use of bisphosphonate in metabolic bone disorders report normal fracture healing and do not indicate or prove impaired fracture healing in normal bones [6-8]. Recently few studies have reported a prolonged bone healing time following fractures in patients receiving bisphosphonate therapy [9]. Recent reports advocate the use of bisphosphonates in OI to decrease the incidence of fractures in these children [1-4]. However, there is no fixed protocol for their use in terms of specific bisphosphonate, its dosage, and duration [10]. Although these reports favor the use of bisphosphonates in OI to decrease the rate of fractures, they do not evaluate their effect on fracture healing or osteotomy healing in OI. We could find only three reports that evaluated the effects of bisphosphonates on fracture and osteotomy healing in OI and these reports are quite contradictory [11-13]. This retrospective study was undertaken to study the effect of parenteral pamidronate or oral alendronate therapy, on bone healing after osteotomies in patients with moderately severe forms (Sillence type 4) of OI [14].
This retrospective study analyzed nine osteotomies for non-union and deformity correction in six patients of moderately severe (Sillence type 4) form of OI who were available for clinical and radiological follow-up for a minimum of 2 years post-surgical management. All the children who have been operated on in the past 15 years were recruited and consent has been obtained from the patients and their families regarding publishing their case history details and pictures. Five patients received bisphosphonate therapy in the form of parenteral pamidronate or oral alendronate in the department of pediatrics to decrease the incidence of new fractures. One patient did not receive any bisphosphonate. Most of the new fractures occurring in these patients were managed conservatively at home by the family members who had become proficient in applying the splints themselves. Hence, data regarding exact time taken for fracture union could not be accurately documented in fractures managed at home. The patients were referred to the orthopedic department only for the management of deformities or non-union of long bone fractures. The patients were diagnosed to have non-union when the fracture failed to unite even after 9 months of sustaining the fracture. The medical records were reviewed for information regarding the specific bisphosphonate used, duration of bisphosphonate therapy, duration of non-union, and the time taken for osteotomy healing. All available radiographs were reviewed to document pre-operative deformity or non-union, radiological healing of non-union or osteotomy, and time taken for union. Non-union in patients with OI was associated with angular deformities. Both the non-union and deformities of long bones were treated by Sofield- Millar procedure which consists of fragmentation of the deformed bone after subperiosteal exposure, excision of the non-union segment, realignment over an intramedullary rod to achieve a near normal limb alignment [15]. The operated limbs were supported in the cast for 2-week post-surgery and then removable splints were advised till complete union was achieved. Postoperatively the bisphosphonates were discontinued and the patients were put on calcium and vitamin D supplementation. Clinical and radiological follow-up was done regularly for a minimum period of 2 years. The clinical follow-up included monitoring for any pain at the non-union site, and also to look for any recurrence of deformity at the same site. The radiological follow-up was done with the help of radiographs and the union was diagnosed when there was a bridging callus on three sides or disappearance of fracture line with trabeculae crossing the fracture site in two planes.
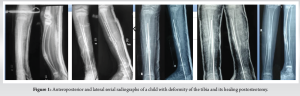
All the patients (four girls and two boys) in our series belonged to Sillence type 4 OI (moderately severe form). The patients were in the age group of 6–13 years with a mean age of 9.6 years. In the bisphosphonate group, four patients were on cyclic parenteral pamidronate therapy while one patient was on oral alendronate therapy. The demographic details of the patients, the type of bisphosphonate therapy, and the time taken for osteotomy healing are presented in Table 1. Out of the seven osteotomies analyzed, two were performed in the femur and five in the tibia. All the patients were available for follow-up for a minimum of 2 years (mean 3.9 years, range 2–7 years). The mean time taken for the osteotomy to heal in the patients receiving bisphosphonates was 10.4 months (range 8–12 months). The healing was confirmed radiologically when there was a bridging callus on three sides or the disappearance of the fracture line with trabeculae crossing the fracture site in two planes [16]. A detailed radiographic series of one child with tibial deformity and corrective osteotomy and healing stages were provided (Fig. 1). Out of the seven osteotomies in patients receiving bisphosphonate therapy, six (86%) showed no or minimal callus around the osteotomy site. One of the patients with OI who was not on any bisphosphonate therapy showed adequate callus around the osteotomy site. The five cases in the bisphosphonate therapy group showed partial healing and a radiolucent line was visible in a small segment of osteotomy for a prolonged time.

Osteogenesis imperfecta is characterized by abnormally weak bones leading to deformities and increased risk of fractures. Histologically, there is an increase in the number of morphologically normal osteoclasts and the number of resorption sites in addition to large-sized osteoblasts. There is an overall increase in bone turnover in patients with OI. Although the bone is weak, fracture healing is normal and the natural history shows that in a significant number of cases, there is exuberant callus formation that may mimic a malignancy [17,18]. Bisphosphonates, both parenteral pamidronate and oral alendronate, have been widely accepted as standard treatment options for patients with this disorder [1-3]. They improve the bone density and reduce the incidence of fractures [2-4]. With the increasing experience in the use of bisphosphonates in OI, some recent reports have raised the concern that bisphosphonates could lead to delay in the bone healing process, possibly, due to interference with the normal osteoclast-osteoblast rhythm of bone healing [11,12]. This was the significant finding in our study where there was a delay in the healing of osteotomy. In our study, we have found that the radiological pattern of osteotomy healing seen in the bisphosphonate group was different from the natural pattern. In the bisphosphonate group, the union was achieved without the typical exuberant callus formation despite bone grafting at the osteotomy. The bone graft gradually disappeared with time and there was no indication of bone grafting after a few months (Fig. 2). The bone healing resembled primary bone healing which occurs after rigid fixation of fracture giving it absolute stability. This was in contrast to the pattern of osteotomy healing seen in patients not receiving bisphosphonates, who demonstrate an abundant amount of bridging callus. Similar was the healing pattern in our case who did not receive any bisphosphonate. They demonstrate a good amount of periosteal bone formation at all the sites where the periosteum is elevated. This is not affected by the presence or absence of bone graft. Our non-bisphosphonate patient demonstrated that the periosteal new bone formed an envelope around the rotated bone fragment which was the middle segment of the osteotomy construct (Fig. 3). This feature of periosteal new bone formation was uniquely absent in the patients who received bisphosphonates. Even the presence of bone graft did not elicit new bone formation from the elevated periosteum in the bisphosphonate group.
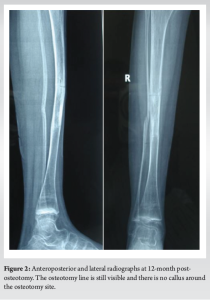
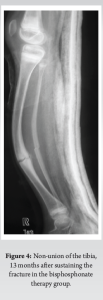
The eventual mechanical strength of the callus is dependent on the physical properties of the callus and the size of the callus. We cannot comment on the physical strength or properties of the callus. But logically, a large amount of callus bridging the bone ends would be stronger than a smaller callus. The union at the osteotomy site without significant callus presents a dilemma for the surgeon concerning weight bearing on the operated limb. Most patients were advised to brace/external support for an extended duration and the weight bearing was delayed. Even after waiting for periods as long as 12 months, the osteotomy site healing appeared “inadequate” to allow unprotected weight bearing (Fig. 2) while in most of the studies using modifications of the Sofield Miller procedure in OI patients not receiving bisphosphonates, the usual time taken for healing of osteotomy is in the range of 7–12 weeks [19, 20]. Non-union of fractures in OI is not unknown but very rare [21,22]. The risk factors for non-union in OI are inadequate mobilization, multiple fractures at the same site, and progressive skeletal angulation [22]. In our series, there were three non-unions and all of these patients were on bisphosphonate therapy (Fig. 3 and 4). Although the importance of the etiological factors mentioned by other authors cannot be underestimated, the significance of the bisphosphonates as an etiological factor for non-union needs to be emphasized here. We feel that it is a significant association even if it may not be a cause. A similar concern for a non-union was expressed by Alharbi et al. who reported delayed union (unhealed even after 6 months) in 30% of patients with OI on parenteral pamidronate therapy [12].
Munns et al. in a retrospective study on a large cohort of patients reported a delay in osteotomy healing in OI patients on intravenous pamidronate therapy. They were not able to identify the exact cause for this differential healing and postulated that this could be due to the presence of an intramedullary rod, the use of an oscillating saw that cauterized the bone ends and early healing of fibula. In our study, we found a delay in healing of osteotomy which ranged from 8 to 13 months. This was similar to the finding of Munns et al. The normal time for healing of osteotomy in the absence of bisphosphonates is 7–12 weeks [19,20]. Our findings that bisphosphonate causes a delay in osteotomy healing is in contrast to several other reports in which osteotomy healing in OI patients was undisturbed by pamidronate therapy [13,23]. El Sobkya et al. reported that bisphosphonate therapy did not affect healing on osteotomies in OI patients and surgery combined with bisphosphonate therapy provided better clinical outcomes than surgery alone in terms of pain relief and overall patient mobility [23]. Pizones et al. based on their findings in seven children with OI on bisphosphonates reported one incidence of the non-union of the femoral osteotomy (14%) but inferred that bone healing is unaffected by bisphosphonate therapy [13]. The limitation of our study is its low sample size. We have provided a single patient as a control group which was a limitation of our study as well.
We infer from our findings that bisphosphonate therapy in OI patients is associated with a different pattern of osteotomy healing and delay in healing of osteotomy.
The radiological pattern of osteotomy healing seen in the bisphosphonate group was different from the natural pattern. In the bisphosphonate group, the union was achieved without the typical exuberant callus formation despite bone grafting at the osteotomy.
References
- 1.Akcay T, Turan S, Guran T, Bereket A. Alendronate treatment in children with osteogenesis imperfecta. Indian Pediatr 2008;45:105-9. [Google Scholar]
- 2.Andiran N, Alikasifoglu A, Gonc N, Ozon A, Kandemir N, Yordam N. Cyclic pamidronate therapy in children with osteogenesis imperfecta: Results of treatment and follow-up after discontinuation. J Pediatr Endocrinol Metab 2008;21:63-72. [Google Scholar]
- 3.Seikaly MG, Kopanati S, Salhab N, Waber P, Patterson D, Browne R, et al. Impact of alendronate on quality of life in children with osteogenesis imperfecta. J Pediatr Orthop 2005;25:786-91. [Google Scholar]
- 4.Land C, Rauch F, Travers R, Glorieux FH. Osteogenesis imperfecta type VI in childhood and adolescence: Effects of cyclical intravenous pamidronate treatment. Bone 2007;40:638-44. [Google Scholar]
- 5.Burnei G, Vlad C, Georgescu I, Gavriliu TS, Dan D. Osteogenesis imperfecta: Diagnosis and treatment. J Am Acad Orthop Surg 2008;16:356-66. [Google Scholar]
- 6.Li C, Mori S, Li J, Kaji Y, Akiyama T, Kawanishi J, Norimatsu H. Long-term effect of incadronate disodium (YM-175) on fracture healing of femoral shaft in growing rats. J Bone Miner Res 2001;16:429-36. [Google Scholar]
- 7.Matos MA, Tannuri U, Guarniero R. The effect of zoledronate during bone healing. J Orthop Traumatol 2010;11:7-12. [Google Scholar]
- 8.Peter CP, Cook WO, Nunamaker DM, Provost MT, Seedor JG, Rodan GA. Effect of alendronate on fracture healing and bone remodeling in dogs. J Orthop Res 1996;14:74-9. [Google Scholar]
- 9.Rozental TD, Vazquez MA, Chacko AT, Ayogu N, Bouxsein ML. Comparison of radiographic fracture healing in the distal radius for patients on and off bisphosphonate therapy. J Hand Surg Am 2009;34:595-602. [Google Scholar]
- 10.Phillipi CA, Remmington T, Steiner RD. Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst Rev 2008;4:CD005088. [Google Scholar]
- 11.Munns CF, Rauch F, Zeitlin L, Fassier F, Glorieux FH. Delayed osteotomy but not fracture healing in pediatric osteogenesis imperfecta patients receiving pamidronate. J Bone Miner Res 2004;19:1779-86. [Google Scholar]
- 12.Alharbi M, Pinto G, Finidori G, Souberbielle JC, Guillou F, Gaubicher S, et al. Pamidronate treatment of children with moderate-to-severe osteogenesis imperfecta: A note of caution. Horm Res 2009;71:38-44. [Google Scholar]
- 13.Pizones J, Plotkin H, Parra-Garcia JI, Alvarez P, Gutierrez P, Bueno A, et al. Bone healing in children with osteogenesis imperfecta treated with bisphosphonates. J Pediatr Orthop 2005;25:332-5. [Google Scholar]
- 14.Sillence D. Osteogenesis imperfecta: An expanding panorama of variants. Clin Orthop Relat Res 1981;159:11-25. [Google Scholar]
- 15.Sofield HA, Millar EA. Fragmentation, realignment, and intramedullary rod fixation of deformities of the long bones in children: A ten-year appraisal. J Bone Joint Surg Am 1959;41:1371-91. [Google Scholar]
- 16.Islam O, Soboleski D, Symons S, Davidson LK, Ashworth MA, Babyn P. Development and duration of radiographic signs of bone healing in children. AJR Am J Roentgenol 2000;175:75-8. [Google Scholar]
- 17.Kutsumi K, Nojima T, Yamashiro K, Hatae Y, Isu K, Ubayama Y, et al. Hyperplastic callus formation in both femurs in osteogenesis imperfecta. Skeletal Radiol 1996;25:384-7. [Google Scholar]
- 18.Rieker O, Kreitner KF, Karbowski A. Hyperplastic callus formation in osteogenesis imperfecta: CT and MRI findings. Eur Radiol 1998;8:1137-9. [Google Scholar]
- 19.Abulsaad M, Abdelrahman A. Modified sofield-millar operation: Less invasive surgery of lower limbs in osteogenesis imperfecta. Int Orthop 2009;33:527-32. [Google Scholar]
- 20.Li YH, Chow W, Leong JC. The Sofield-Millar operation in osteogenesis imperfecta. A modified technique. J Bone Joint Surg Br 2000;82:11-6. [Google Scholar]
- 21.Agarwal V, Joseph B. Non-union in osteogenesis imperfecta. J Pediatr Orthop B 2005;14:451-5. [Google Scholar]
- 22.Gamble JG, Rinsky LA, Strudwick J, Bleck EE. Non-union of fractures in children who have osteogenesis imperfecta. J Bone Joint Surg Am 1988;70:439-43. [Google Scholar]
- 23.El-Sobky MA, Hanna AA, Basha NE, Tarraf YN, Said MH. Surgery versus surgery plus pamidronate in the management of osteogenesis imperfecta patients: A comparative study. J Pediatr Orthop B 2006;15:222-8. [Google Scholar]