The use of home 3D printers and open-source software, as well as the creation of a multidisciplinary 3D unit with orthopedic surgeons and bioengineers, makes it possible to obtain customized guides or implants with satisfactory clinical results at minimal cost.
Dr. Miguel Márquez-Gómez, Resident, Department of Orthopaedic and Trauma Surgery, Hospital General Universitario Gregorio Marañon, C. Dr. Esquerdo 46, 28007, Madrid, Spain. E-mail: marquez.gomez.miguel@gmail.com
Introduction: Extra-articular deformity is that located proximal to the femoral epicondyles or distal to the neck of the fibula. In patients with gonarthrosis associated with extra-articular deformity, a different evaluation and approach will be necessary at the time of planning the arthroplasty. 3D planning and printing techniques have had a major impact on pre-operative planning, allowing the production of custom guides at low cost and in an accessible way. To our knowledge, this is the first report of combined 3D-guided extra-articular femoral osteotomy and total knee arthroplasty (TKA) for the treatment of extra-articular deformity and knee osteoarthritis.
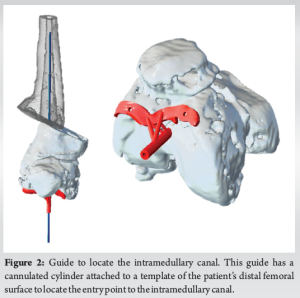
Case Report: We present the case of a 48-year-old caucasian male with gonarthrosis and a history of supracondylar femoral fracture with vicious consolidation. The pre-operative scan images were used for planning in collaboration with the engineers of the 3D planning and printing unit of our hospital. Two guides were designed and printed using biocompatible resin. The first one has a cannulated cylinder attached to a template of the patient’s distal femoral surface to locate the entry point to the intramedullary canal. The second one fits the anterior cortex of the femur, over the fracture callus, and has six cannulated cylinders attached; four of them guided K-wires through the plane of the osteotomy and the other two guided position K-wires that would ensure canal alignment in the next step. A fixation and control plate was designed to maintain the corrected alignment until the definitive fixation with a retrograde femoral nail. After corrective osteotomy and fixation, TKA was performed. Six months after surgery, the patient is independent, pain-free, and does not use mechanical aids for walking. X-ray shows consolidation of the osteotomy and restoration of the mechanical axis of the limb.
Conclusion: The use of home 3D printers and open-source software, as well as the creation of a multidisciplinary 3D unit with orthopedic surgeons and bioengineers, makes it possible to obtain customized guides or implants with satisfactory clinical results at minimal cost.
Keywords: 3D, extra-articular deformity, total knee arthroplasty, custom-made guides.
Extra-articular deformity is that located proximal to the femoral epicondyles or distal to the neck of the fibula. In patients with gonarthrosis associated with extra-articular deformity, a different evaluation and approach will be necessary at the time of planning the total knee arthroplasty (TKA) [1]. In large deformities, normally over ten degrees in the coronal plane, it is recommended to perform a corrective extra-articular osteotomy followed by arthroplasty, either simultaneously or staged. Alternatively, the deformity correction and the TKA can be done at the same time taking the deformity into account by intra-articular bone resections [2]. This is possible for deformities under 20° in the coronal plane and it is recommended to have a pre-operative computed tomography (CT) scan to assess the deformity in all planes. 3D planning and printing techniques have had a major impact on pre-operative planning, allowing producing three-dimensional printed anatomical models, custom implants, plates, or guides at low cost and in an accessible way [3].
We present the case of a 48-year-old Caucasian male with gonarthrosis requiring arthroplasty, with a history of supracondylar femoral fracture with a vicious consolidation (Fig. 1).
On physical examination, the patient was obese and the knee was stable with a range of motion of 15–70°. The pre-operative CT scan described the deformity as a pure horizontal translation of 4 cm and 3 cm of shortening. The surgical plan was a one-stage surgery: hardware removal, oblique osteotomy at 23° calculated by trigonometry using 3D-printed patient-specific guides, fixation of the correction with an intramedullary retrograde femoral nail, and TKA.
Pre-operative planning
Lower limb X-ray and CT scan of the right femur and knee were requested for pre-operative planning. The CT scan DICOM images were imported into a radiological postprocessing software (3D Slicer). The 3D model obtained was used for planning in collaboration with the engineers of the 3D planning and printing unit of our hospital.
Two guides were designed with Meshmixer. The first one has a cannulated cylinder attached to a template of the patient’s distal femoral surface to locate the entry point to the intramedullary canal (Fig. 2). The second one fits the anterior cortex of the femur, over the fracture callus, and has six cannulated cylinders attached; four of them guided K-wires through the plane of the osteotomy and the other two guided position K-wires that would ensure canal alignment in the next step (Fig. 3).
A fixation and control plate was designed to maintain the corrected alignment until the definitive fixation with a retrograde femoral nail, using the two position K-wires put before the osteotomy (Fig. 4).
The guides and plate were printed using biocompatible resin and sterilized for surgical use (Fig. 5).
Surgical technique
The patient was placed in the supine position and we used an anteromedial approach with a proximal extension to expose the distal femur. The osteotomy guide was applied on the anterior femoral surface and guided six K-wires, four following the osteotomy plane and two position K-wires. Then, the osteotomy guide was removed, keeping the K-wires in place, and we performed the osteotomy with an oscillating saw, sliding it just proximal to the K-wires. A lateral displacement of 40 mm and a lengthening of 17 mm was achieved as planned, using the two position K-wires as a guide. We maintained the correction and canal alignment with the designed plate, which was fixed with four screws (Fig. 6).
The other femoral guide was applied on distal femur, guiding the intramedullary rod in the canal. The distal femur cut was made before definitive fixation of the osteotomy with a retrograde femoral nail. Finally, TKA was performed.
Clinical outcomes
There were not any early post-operative complications and the post-operative X-ray showed that planned length correction and femoral translation were achieved (Fig. 7). The patient was discharged one week after surgery weight-bearing with crutches.
One month after discharge the patient still needed one crutch to walk. The wound had completely healed at this point and the X-ray showed no signs of loosening or complication of the osteotomy. Six months after surgery, the patient is independent, pain-free, and does not require mechanical aids for walking. He has a range of motion from 0 to 100 degrees. Lower-limb X-ray shows consolidation of the osteotomy and restoration of the mechanical axis of the limb (Fig. 8).
Deformity correction by intra-articular bone resections allows single-stage TKA in patients with knee osteoarthritis associated with extra-articular femoral deformity, reducing costs as well as the potential complications of an extra-articular osteotomy [2, 4]. Vedoya et al. followed 28 patients with knee osteoarthritis associated with extra-articular deformity over ten degrees who underwent one-stage TKA, corrected by intra-articular bone resections and soft tissue release. They report excellent results with an average follow-up of 10.3 years, with improved range of motion and restoration of the mechanical axis [5]. Our patient had a pure horizontal translation of 4 cm and 3 cm of shortening. Intra-articular bone resections would allow correction of alignment in the coronal plane but would not restore the length of the leg. Femoral extra-articular osteotomy allows multiplanar correction but is a challenging procedure that depends on the complexity of the deformity [6]. Many authors have reported the use of 3D planning and printing technology, especially for traumatology, reconstructive, orthopedic, and oncology surgery. Some examples are the design of 3D-printed osteotomy guide plates for fractures and osteotomies [7] and custom-made implants [8, 9]. To our knowledge, this is the first report of combined 3D-guided extra-articular femoral osteotomy and TKA for the treatment of extra-articular deformity and knee osteoarthritis. Kappel et al. reported in 2021 a case of one-stage TKA and correction of extra-articular tibial deformity using custom-made 3D cutting guides with satisfactory clinical results [10]. Assisted by 3D printing technology, the osteotomy can be performed with high precision, using custom-made guides that control position and angulation of the osteotomy plane for deformity correction, even multi-planar if necessary. Following the “do-it-yourself” philosophy, the design, production, and printing of the guides were carried out in an in-hospital circuit without the collaboration of external companies.
This technique helps the orthopedic surgeon to reduce human error as well as surgical time. 3D planning lets us carry the surgical steps in a virtual environment and even with tangible printed models, and is reproducible in the operating room.
The use of home 3D printers and open-source software, along with the establishment of a multidisciplinary 3D unit with orthopedic surgeons and bioengineers, enables the production of customized guides or implants with satisfactory clinical results at minimal cost.
References
- 1.Sculco PK, Kahlenberg CA, Fragomen AT, Rozbruch SR. Management of extra-articular deformity in the setting of total knee arthroplasty. J Am Acad Orthop Surg 2019;27:e819-30. [Google Scholar]
- 2.Wang JW, Wang CJ. Total knee arthroplasty for arthritis of the knee with extra-articular deformity. J Bone Joint Surg Am 2002;84:1769-74. [Google Scholar]
- 3.Meng M, Wang J, Sun T, Zhang W, Zhang J, Shu L, et al. Clinical applications and prospects of 3D printing guide templates in orthopaedics. J Orthop Translat 2022;34:22-41. [Google Scholar]
- 4.Xiao-Gang Z, Shahzad K, Li C. One-stage total knee arthroplasty for patients with osteoarthritis of the knee and extra-articular deformity. Int Orthop 2012;36:2457-63. [Google Scholar]
- 5.Vedoya SP, Sel HD. Total knee arthroplasty and extra-articular deformity: Deformity correction with intra-articular bone resections. 10 years follow up. J Orthop 2021;23:219-24. [Google Scholar]
- 6.Lonner JH, Siliski JM, Lotke PA. Simultaneous femoral osteotomy and total knee arthroplasty for treatment of osteoarthritis associated with severe extra-articular deformity. J Bone Joint Surg Am 2000;82:342-8. [Google Scholar]
- 7.Aman ZS, DePhillipo NN, Peebles LA, Familiari F, LaPrade RF, Dekker TJ. Improved accuracy of coronal alignment can be attained using 3D-printed patient-specific instrumentation for knee osteotomies: A systematic review of level III and IV studies. Arthroscopy 2022;38:2741-58. [Google Scholar]
- 8.Costanzo R, Ferini G, Brunasso L, Bonosi L, Porzio M, Benigno UE, et al. The role of 3D-printed custom-made vertebral body implants in the treatment of spinal tumors: A systematic review. Life (Basel) 2022;12:489. [Google Scholar]
- 9.Haglin JM, Eltorai AE, Gil JA, Marcaccio SE, Botero-Hincapie J, Daniels AH. Patient-specific orthopaedic implants. Orthop Surg 2016;8:417-24. [Google Scholar]
- 10.Kappel A, Nielsen PT, Kold S. 1-stage total knee arthroplasty and proximal tibial non-union correction using 3-D planning and custom-made cutting guide. Acta Orthop 2021;92:452-4. [Google Scholar]