Patients who have sustained a cat bite with a suspected infection should present as early as possible for an evaluation by a medical professional and should have early appropriate administration of empiric antibiotics, and early surgical debridement when warranted to help prevent complications.
Dr. Brett Lewellyn, 60 W Columbia ST, Orlando, FL 32806. E-mail: Brett.lewellyn@orlandohealth.com
Introduction: Cat bites are a remarkably common injury seen in the emergency department )setting . Due to the morphology of feline teeth and anatomy of the human hand, seemingly innocuous surface bites can seed infections in deeper structures of the hand that can result in adverse outcomes. We report on a case of a rare complication of a flexor tendon rupture that occurred well after the initial treatment of a superficial infection.
Case Report: A healthy 61 year old male presented to the emergency department with concerns for possible infection after sustaining a cat bite to the proximal phalanx of his left long finger 48 hoursh earlier. The patient was treated for suspected cellulitis and underwent irrigation and debridement within 36 hoursh. Five months after presentation, it was determined that the patient had suffered a spontaneous rupture of the flexor digitorum profundus tendon of the left long finger. The patient underwent surgical debridement, flexor tendon tenolysis, and tendon reconstruction. Postoperatively, the patient returned to normal activities with good function of his left hand after a course of occupational therapy.
Conclusion: The purpose of this case report is to describe the clinical course of a patient with the rare complication of a flexor tendon rupture after being bitten by a cat, as well as to review the current literature and treatment for feline bite-related hand injuries. We recommend patients who have sustained a cat bite with a suspected infection to present as early as possible for an evaluation by a medical professional, early appropriate empiric antibiotic administration, and early surgical debridement when warranted to help prevent complications.
Keywords: Cat bite, flexor tendon rupture, infection.
There are approximately 400,000 feline bites in the United States each year and of these, roughly 1–2% will present to the emergency department (ED) for medical treatment [1fig. Common sequelae after a cat bite or cat scratch are usually infectious in nature and can be resolved with antibiotics and surgical irrigation and debridement when indicated with minimal complications [1]. We present an uncommon complication of a spontaneous flexor tendon rupture after being bitten by a cat. This novel case demonstrates an uncommon sequela that occurred despite appropriate medical intervention that has yet to be reported on.
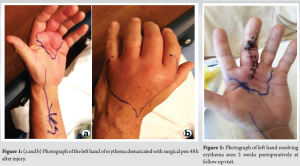
A 61-year-old right-hand dominant male presented to our institution’s ED within 48 h hours of being bitten on the left long finger proximal phalanx by his pet cat. He had complaints of worsening pain, redness, and swelling of his middle finger and left hand, with subjective fever and chills but no drainage from the wound. He had an uncomplicated medical history and had no previous injuries or surgery with regard to his left hand. Twenty-four hours earlier, he was treated at an outside hospital with vancomycin, rocephin, and a tetanus booster, and was told to follow-up with his primary care doctor. Due to worsening symptoms overnight, he presented to our institution’s ED, and the hand team was consulted. On examination, all digits had full range of motion (ROM) and there was no purulence or discreet fluctuations on palpation. There was localized erythema and swelling over the dorsal and palmar hand surfaces which were outlined with a surgical site marking pen to follow the progression of the erythema margins (Fig. 1a and b). Laboratory values on admission revealed leukocytosis and an elevated C-reactive protein. The patient was placed on an intravenous (IV) broad-spectrum antibiotic regimen of clindamycin and ancef. There was minimal resolution 24 h hours later and the patient underwent surgical irrigation and debridement through a standard Bruner’s incision during which culture swabs and tissue samples were taken and the wound was loosely closed over a Penrose drain. The patient’s tendon pulleys, the flexor digitorum superficialis (FDS), and the flexor digitorum profundus (FDP) tendons were intact. IV vancomycin, ceftriaxone, and azithromycin were started postoperatively, and tissue cultures eventually grew Pasteurella multocida. The patient was discharged on the 5th day of admission on a 10-day course of Augmentin. During the first post-operative visit 2 weeks later, the erythema margins had receded and the incision was healing well without drainage (Fig. 2). The patient was neurovascularly intact and had a normal examination of all digits, including tendons, and was instructed to start occupational therapy (OT) and was given a prescription for it.
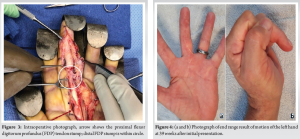
The patient did have a delay in starting therapy and he returned to the outpatient clinic 6 weeks later with complaints of stiffness in his left long finger and decreased ROM. The patient was firing both his FDS and FDP tendons and had 90 degrees of ROM through both the metacarpophalangeal (MP) and proximal interphalangeal (PIP) joints and was lacking 3 cm fingertip to palm. A prescription for additional OT was given with a follow-up appointment scheduled for 8 weeks. The patient returned to clinic 4 months later with a resolved infection and a stiff hand. Active FDS function was noted; however, the patient was unable to pull through his long finger FDP tendon. The patient denied any additional trauma or infection. The patient was scheduled for exploration with possible tendon tenolysis versus repair/transfer. The surgery was performed 22 weeks after his initial surgical debridement at our institution. During surgery, scarring and adhesions were seen extending from the long finger middle phalanx into the mid palm. A zone II rupture of the FDP tendon was seen proximal to the FDS decussation with retraction of the proximal FDP stump into the mid palm (Fig. 3). A complete tenolysis of the FDS and FDP tendons was performed. After debriding the tendons, the patient was left with a gap of approximately 2.5 cm between the FDP tendon ends, and a single staged primary FDP tendon reconstruction was performed by splitting the proximal FDP tendon longitudinally, reversing it, and using it as a tendon interposition graft with a Pulvertaft weave.
Postoperatively, the patient began immediate OT 3 days a week and performed daily exercises on his own. Formal OT continued for 16 weeks. At his final follow-up visit, the patient had normal function with regard to activities of daily living but subjective dysfunction with some maneuvers while at work in his office. His final physical examination revealed active pulling through the FDP and FDS, with 90° of active ROM through the MP and PIP joints of the affected finger (Fig. 4a and b).
Animal bites in the US are a common occurrence with anywhere from 1.5 to 2 million occurring annually [1]. While over 90% of these bites are canine-related, feline bites often have higher morbidity, with sequelae such as infection reaching rates as high as 50% [2-4]. There are several reasons for these increased infection rates. Felines have sharp, needle-shaped teeth that puncture and inject tissue with their oral bacterial flora. Due to the small diameter but large depth of the wound, the puncture wound often heals superficially which traps inoculated bacteria within the wound allowing abscess development. Similarly, due to the small size and benign appearance of the cat bite wound, medical attention is rarely pursued which can lead to a delay in antibiotic treatment. Previous studies have shown a direct correlation between delay in treatment and severity of infection for cat bite injuries [3, 4]. Another possible reason for the high infection rate is the location of injury. Cat bites occur to the hand and fingers 45–80% of the time compared to other areas of the body, and multiple studies have shown higher rates of infection when the hand is bitten [1, 3-6]. This could be explained by the fact that the hand, compared to the lower extremity, often has fewer layers of protective clothing which allows for deeper inoculation of oral flora. Finally, cat bites are also associated with the organism P. multocida. This bacterium is found in the oral flora in up to 90% of cats and exposure to this bacterium often leads to aggressive, recalcitrant infections due to the fast-replicating nature of the organism [7, 8]. If presentation to a medical facility and antibiotic initiation is delayed, often complicated infections can result. Once a cat bite-related infection occurs, appropriate medical attention is needed. A review of the literature shows that there is no widely accepted algorithm for the triage and treatment of cat bite injuries. At our institution, we advocate an initial evaluation by a licensed medical practitioner as soon as possible with the adherence to the following steps to expedite recovery and minimize complications. For acute presentation of a cat bite with possible infection, plain radiographs should be taken of the affected body part to identify any foreign bodies such as broken teeth. If these are embedded in the superficial tissue and are easily removable, then this can be done under local anesthetic in the clinic or ED suite along with irrigation with a diluted betadine/saline solution in a one-to-ten ratio. This ratio has been shown to cause the least amount of toxicity to native tissue while still displaying antibiotic properties [9]. Wounds should be left open without sutures to allow for drainage which can help prevent abscess formation [5]. Broad-spectrum antibiotics, including coverage for P. Multocida, should be initiated and tetanus status addressed. Wounds should be cleansed twice daily with soap and water and covered loosely or left open to air. Appropriate education and counseling is imperative for the patient and family members with regard to wound care, follow-up, as well as signs of potential complications including increasing swelling, fevers, or advancing erythema. At our institution, we prefer to see all patients for follow-up evaluation within 5 days of initial presentation. Cat bite injuries with delayed presentation that show no signs of infection do not need to be cultured, nor do they need prophylactic antibiotics. However, injuries with a cellulitic appearance, but no signs of a discreet fluid collection such as an abscess, should still be started on empiric antibiotics such as Augmentin [1, 10]. Penicillin and ampicillin are no longer recommended due to the prevalence of resistant Staphylococcus that can be found in cat bite wound cultures [8]. Azithromycin, although not solely effective against oral feline bacteria, should be added to an antibiotic regimen if there are cat scratches to treat potential Bartonella henselae infection. Antibiotics can be administered on an outpatient basis with close follow-up scheduled. Feline bites and scratches demonstrating abscesses on advanced imaging, Kanavel’s signs on examination, no resolution of symptoms with appropriate antibiotics, or obvious signs of a fulminant infection, such as a draining wound or palpable fluctuance, warrant urgent surgical debridement. We recommend using an incision large enough to evacuate the entire tendon sheath for flexor tenosynovitis, as well as irrigation with a 1: 10 betadine solution, followed with normal saline. Exsanguination should be accomplished with gravity only, rather than with an Esmarch bandage to prevent abscess propagation. Six liters of saline irrigation delivered by cystoscopy tubing rather than jet lavage has yielded good results at our institution. We choose to close the incision loosely over a quarter-inch Penrose drain that is pulled at the bedside 24–48 hoursh later. The patient is then discharged with close follow-up scheduled, typically within 5 days of surgery. Any bite with questionable fluid collection on examination should undergo advanced imaging with either ultrasound or magnetic resonance imaging to confirm if there is a drainable abscess. If no abscess is present, then the patient is admitted for a course of observation with IV antibiotics.
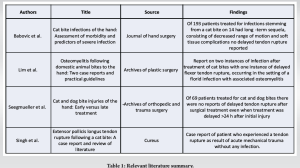
The case presented is unique in that despite appropriate treatment upon presentation for their cat bite injury, this patient suffered an uncommon complication of a delayed flexor tendon rupture, which, as far as we know, has not been reported in the scientific literature(Table 1). One possible reason for the tendon rupture in our patient is the delay in surgical treatment. Studies have shown an increase in complication rates when surgical debridement occurs more than 48 hours h after a cat bite [6]. Our patient had a 72 hour h surgical delay from their initial injury due to an original presentation to an outside hospital. Although they were administered appropriate antibiotics both at the outside hospital and at our institution, the delay in surgical debridement may have allowed time for inoculated bacteria to weaken the FDP tendon. This slow deterioration of the tendon could have caused its rupture many weeks after surgical treatment. Another possibility is that the FDP tendon was partially lacerated during the initial injury, causing scarring and adhesions which could have led to an iatrogenic injury during formal physical therapy or during the patient’s normal activity. However, this is unlikely as the tendons were directly visualized during surgery and no discreet injury was seen with regard to the tendon or pulley system.
This case demonstrates an uncommon sequela after a common injury, a cat bite to the hand. While there are a variety of complications that commonly occur following feline bites such as infections, delayed wound healing, and scarring with contractures, tendon rupture is a rare complication that is uncommonly reported in the literature. Due to the fact that there is no widely accepted treatment algorithm for cat bite injuries, we have provided our institution’s treatment strategy to help minimize potential complications. At our institution, we advocate for patients who have sustained a cat bite with a suspected infection to present as early as possible for an evaluation by a medical professional, early appropriate empiric antibiotic administration, and early surgical debridement when warranted to help prevent complications.
Patients who sustained a cat bite to the hand can have concealed sequestered infections, early appropriate empiric antibiotic administration, and early surgical debridement, when warranted, can prevent adverse events from what may otherwise disregarded as a minor injury.
References
- 1.Goldstein EJ. Bite wounds and infection. Clin Infect Dis 1992;14:633-40. [Google Scholar]
- 2.Griego RD, Rosen T, Orengo IF, Wolf JE. Dog, cat, and human bites: A review. J Am Acad Dermatol 1995;33:1019-29. [Google Scholar]
- 3.Dire DJ. Cat bite wounds: Risk factors for infection. Ann Emerg Med 1991;20:973-9. [Google Scholar]
- 4.Mitnovetski S, Kimble F. Cat bites of the hand. ANZ J Surg 2004;74:859-62. [Google Scholar]
- 5.Babovic N, Cayci C, Carlsen BT. Cat bite infections of the hand: Assessment of morbidity and predictors of severe infection. J Hand Surg 2014;39:286-90. [Google Scholar]
- 6.Seegmueller J, Arsalan-Werner A, Koehler S, Sauerbier M, Mehling I. Cat and dog bite injuries of the hand: Early versus late treatment. Arch Orthop Trauma Surg 2020;140:981-5. [Google Scholar]
- 7.Freshwater A. Why your housecat’s trite little bite could cause you quite a fright: A study of domestic felines on the occurrence and antibiotic susceptibility of Pasteurella multocida. Zoonoses Public Health 2008;55:507-13. [Google Scholar]
- 8.Talan DA, Citron DM, Abrahamian FM, Moran GJ, Goldstein EJ. Bacteriologic analysis of infected dog and cat bites. Emergency medicine animal bite infection study group. N Engl J Med 1999;340:85-92. [Google Scholar]
- 9.Hollander JE, Singer AJ. Laceration management. Ann Emerg Med 1999;34:356-67. [Google Scholar]
- 10.Esposito S, Picciolli I, Semino M, Principi N. Dog and cat bite-associated infections in children. Eur J Clin Microbiol Infect Dis 2013;32:971-6. [Google Scholar]
- 11.Lim JS, Byun JH, Min KH, Lee HK, Choi YS. Osteomyelitis following domestic animal bites to the hand: Two case reports and practical guidelines. Arch Plast Surg 2016;43:590-4. [Google Scholar]
- 12.Singh S, Adamji S, Badge R. Extensor pollicis longus tendon rupture following a cat bite: A case report and review of literature. Cureus 2023;15:e43940. [Google Scholar]