Infrapatellar fat pad has a undefined role, any many a times it’s pathologies may present with a calcified mass and their management is excision, as they are of benign nature mostly.
Dr. Kamparsh Thakur, Department of Orthopaedics, 166 Military Hospital, Jammu, Jammu and Kashmir, India. E-mail: drkamparsh@gmail.com
Introduction: Infrapatellar fat pad (IFP) calcification is a rarely reported entity in the literature. Only a few cases have been reported so far and that too as case reports. The authors in the present study present two cases of IFP calcification. We also did a thorough review of the literature on the clinical presentation, etiology, and management of the rarely reported entity and present it as a narrative review.
Materials and Methods: Cases: Three cases managed by the authors are presented as case reports. A narrative review of the PubMed and Cochrane database was carried out using MeSH headings and subheadings in various combinations (i.e., IFP calcification and IFP calcified mass and para-articular osteochondroma knee and Hoffa’s fat pad calcification). The data from the previous studies and case reports were extracted (Age, sex, symptoms, duration of symptoms, management, and pathological assessment).
Results: We in this study present 03 cases who had presented with large IFP mass with calcification on radiographs. They underwent excision of the mass and had an uneventful recovery. Narrative review of the literature was done which showed 36 such cases in 26 studies which were reported so far with a calcified mass in the IFP. The mean age of presentation was 49.64 years (16–78 years). The duration of symptoms varied from 02 to 360 months. The average volume of the mass excised was 99.91 cc. The management was excision of the mass in all except two cases, who underwent total knee arthroplasty and one which was managed conservatively. The lesions were benign in nature on clinical presentation and on histopathological assessment.
Conclusion: IFP has no clearly defined function and role; however, it is known to harbor various pathologies. These can present as a calcified mass on radiographs and are generally benign in nature. The management primarily is excision in majority of the cases.
Keywords: Infrapatellar fat pad, calcification, calcified mass.
Infrapatellar fat pad (IFP) is an intracapsular extra-synovial structure, with no clearly defined function and role. Many patients present with anterior knee pain or swelling due to disorders localized to IFP such as Inflammation and fibrosis, synovial disorders, synovitis, pigmented villonodular synovitis, symptomatic plica, mass-like abnormalities, Hoffa’s disease (HD), and cartilage abnormalities [1]. Calcified mass appreciable on radiographic imaging in the IFP region is due to synovial chondromatosis, osteochondroma, or end stage HD [1, 2]. Synovial chondromatosis has a thickened synovial lining and is intra-synovial in location, whereas osteochondromas are extra-synovial and have an isolated uninodular appearance [1, 3]. End-stage HD has a similar radiographic appearance as solitary osteochondroma, but on pathological examination has surrounding fibroadipose tissue and hemosiderin deposits [2]. The purpose of the present study is for two reasons, first, to present three cases who had similar presentation as mass in the IFP region and calcified appearance on radiographic imaging, but with different etiologies, and second, to perform a review of the literature for lesions with calcified mass in the IFP.
Case
Three cases who had presented with swelling in the IFP with calcified mass on radiographs, underwent excision, and had an uneventful recovery are being presented.
Narrative review
A review was conducted and PubMed and Cochrane database were searched in using MeSH headings and subheadings in various combinations (i.e., IFP calcification and IFP calcified mass and para-articular osteochondroma knee and Hoffa’s fat pad calcification) to increase sensitivity. Due to the paucity of literature related to IFP impingement, we included any study related to IFP calcification derived from the search regardless of study design or patient demographics. Results were limited to humans, English, and the publication dates 1950–2023. Studies or reports with infrapatellar calcified mass were included for the review. Studies presenting with locations other than IFP were excluded from the study. Reports with multiple cases and had a case with IFP calcified mass were included in the study. The studies where the full text could not be retrieved or were not in English were excluded of the study. Two independent reviewers screened the text and included the studies if they were eligible. The references of the selected studies and studies which cited them were also screened and studies which met our selection criteria were included in the review. Following data were extracted from the studies: Age, sex, symptoms, duration of symptoms, management, and pathological assessment.
Cases
Case 1
A 16-year-old healthy adolescent male presented to our outpatient department (OPD) with a gradually progressive swelling in the anterolateral aspect of the right knee in the IFP. On examination, the knee was essentially normal with no ligamentous laxity and preserved range of motion. The overlying skin was normal in consistency and texture. Radiograph revealed a calcified mass in IFP region. Subsequent magnetic resonance imaging (MRI) showed a well marginated and circumscribed mass, with few hemorrhagic areas in the swelling. The patient underwent excision biopsy after a diagnostic arthroscopy. The lining synovium was normal with no evidence of any synovial pathology. The swelling was not attached to any surrounding structure, measured 7 × 6.5 × 3 cm in size and was excised en mass. Histopathological assessment revealed it to be osteochondroma. As the swelling was localized to IFP, with hemorrhagic foci inside and osteochondral picture, it was suggestive of end-stage HD (Fig. 1).
A 77-year-old male presented to the OPD with swelling of the left knee of 5-year duration. It was gradually increasing in size and had not started with occasional episodes of locking of knee. On examination, the knee had stiffness with terminally restricted flexion of the knee. Radiographic evaluation showed a calcified mass in IFP region. The patient underwent excision biopsy of the swelling. The synovium was normal with evidence of inflammation. The swelling was intracapsular and extra-synovial in location and measured 06 × 5 × 03 cm. The inferior aspect abutted the tibial plateau, and the overlying cartilage layer was absent. It was a separate mass with no attachments to nearby structures. Histopathological examination (HPE) revealed the swelling to be osteochondroma. With the typical location and extra-skeletal origin and no evidence of hemorrhagic foci, it was suggestive of para-articular extra-synovial osteochondroma (Fig. 2).
Case 3
A 35-year-old male presented with complaints of pain on the anterior aspect of the knee for 4 months duration with antecedent history of trauma. The pain was occasional and not related to any other factor. On examination, there was minimal tenderness in the infrapatellar region anteriorly. The knee movements and ligaments were preserved. Radiographic evaluation showed a small, calcified mass in the infra-patellar region. MRI confirmed the nature of the swelling to be osteo-cartilaginous in the IFP. The patient underwent arthroscopic excision of the mass. The mass measured 02 × 02 × 02 cm. The mass was located in the IFP and was not adherent to nearby structures. Histopathological evaluation revealed the mass to be osteochondroma. Based on the location and the HPE, the swelling was diagnosed to be para-articular extra-synovial osteochondroma (Fig. 3).
Narrative Review
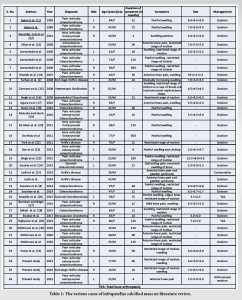
The reports and studies searched and identified on the PubMed and Cochrane database were further assessed for the eligibility and data collection. For increasing the scope of the review, the studies and reports included were further screened for their references and citations, and reports meeting our inclusion criteria were included in the review. Thirty-six cases in 26 studies (including the present study) were analyzed for their descriptions and outcomes (Table 1). There were multiple etiologies which led to IFP calcification as shown in Table 2. Twenty-six cases (Right-16; Left-10) were identified where side was mentioned. Of the 36 cases, 20 were male and 16 were female. The mean age at presentation was 49.64 years (range 16–78 years). The symptoms were mostly swelling, with pain (25 cases) and restricted range of motion (mostly flexion). The duration of symptoms was mentioned in 29 studies and ranged from 2 to 360 months with mean duration being 70.2 months. The average size was reported in 23 studies and the average volume of the calcified mass was 99.91 cc. The management in most of the cases was excision of the swelling, two patients underwent total knee arthroplasty (TKA) in the same seating, whereas one was managed conservatively (Table 2).
IFP or Hoffa’s fat pad is an intra-articular extrasynovial structure, has role as a space filling organ, and has vital functions in the joint as synovial fluid secretion, lubrication of joint, and shock absorption [4]. In addition, due to the anatomy, pattern of neurovascular structure, and the adipose contents which secrete plenty of proinflammatory cytokines and adipokines, it is presumed to be contributory to osteoarthritis of the knee [4, 5]. The multipotent stem cells derived from IFP are known to possess chondrogenic, osteogenic, and adipogenic stimuli [6]. Thus, for calcification to result in the IFP, it contains the necessary potion, but the initiating circumstances vary for the pathological process to set in.
In the present review, we analyzed the reports of lesions with IFP calcified mass, and the underlying reported pathology varied to an extent. These pathologies were para-articular osteochondroma, synovial chondromata, HD, and heterotopic ossification. None of swelling had any evidence of malignant changes. Extraskeletal osteochondromas have been divided into three types: Synovial chondromatosis, para-articular chondroma/osteochondroma, and soft-tissue chondroma [7]. These have been given different nomenclature in the literature by various authors despite having a similar HPE picture. Our review shows that these are the most common cause of IFP calcification (29 cases out of 36). The radiographic picture shows an isolated calcified mass. The management of these is primarily excision with no evidence of any recurrence [8]. One patient underwent a simultaneous TKA as they had evidence of advanced osteoarthritis. On the other hand, synovial chondromatosis is known to affect joints such as knee, hip, shoulder, and elbow. The pathology involves the complete synovium and forms multiple free cartilaginous bodies, which undergo calcification by a process of metaplasia [9]. The radiographic picture of these shows multiple calcified mass with round or oval appearance. We came across two cases of synovial chondromatosis with IFP calcification. One was managed with excision and the other underwent TKA. HD is thought to be a result of repetitive microtrauma or acute injury and further leading to hemorrhage, inflammation, hypertrophy, and further edema of IFP [10]. Culminating as an ossified mass is an extremely rare occurrence and has been defined as an end-stage HD. One interesting finding was presence or evidence of hemosiderin, which likely suggests hemorrhage in the IFP [2]. Thus, the presence of hemosiderin favors the diagnosis of HD and should be looked for during the MRI and HPE of the swelling. The spectrum of the patients varied from adolescents to as late as 8th decade, the youngest patient was 16 year old (our case) and the eldest was 78 year old. This clearly confirms that no age group is at risk. The symptoms varied from benign asymptomatic presentation with no evidence of arthritis to a painful swelling with restricted range of motion with advanced osteoarthritis of the knee. However, for the patient to seek medical attention, it took a long time (02 months to 360 months), as it rarely was a cause of discomfort or any other symptoms when the size was evolving. The management generally involved excision of the swelling when there was no associated pathology and TKA in patients who had advance osteoarthritis of the knee. Only one patient was managed conservatively. The IFP is known to play a role in various pathologies of the knee, as has been confirmed by the presence of proinflammatory cytokines and adipokines. These can be predicted to play a role in isolated IFP calcification, which can be found in para-articular extra-synovial osteochondroma, synovial chondromatosis, and HD. These lesions are mostly benign in nature and can be safely managed with excision or TKA in select cases.
IFP calcification is a clinical result in pathologies such as para-articular osteochondroma, synovial chondromata, HD, and heterotopic ossification. The fat pad is known to consist of the various chondrogenic stimuli for the pathological process to initiate and end with a calcified mass. The resultant mass is of benign origin and management involves excision or knee arthroplasty in case if associated with arthritis of knee.
Infrapatellar calcified mass is mostly benign with different possible etiology, and the management is by excision; however, this should not prevent the surgeon to negate the importance of a histopathological evaluation.
References
- 1.Dragoo JL, Johnson C, McConnell J. Evaluation and treatment of disorders of the infrapatellar fat pad. Sports Med 2012;42:51-67. [Google Scholar]
- 2.Turhan E, Doral MN, Atay AO, Demirel M. A giant extrasynovial osteochondroma in the infrapatellar fat pad: End stage Hoffa’s disease. Arch Orthop Trauma Surg 2008;128:515-9. [Google Scholar]
- 3.Saxena S, Patel DD, Shah A, Doctor M. Fat chance for hidden lesions: Pictorial review of Hoffa’s fat pad lesions. Indian J Radiol Imaging 2021;31:961-74. [Google Scholar]
- 4.Jiang LF, Fang JH, Wu LD. Role of infrapatellar fat pad in pathological process of knee osteoarthritis: Future applications in treatment. World J Clin Cases 2019;7:2134-42. [Google Scholar]
- 5.Zhou S, Maleitzke T, Geissler S, Hildebrandt A, Fleckenstein FN, Niemann M, et al. Source and hub of inflammation: The infrapatellar fat pad and its interactions with articular tissues during knee osteoarthritis. J Orthop Res 2022;40:1492-504. [Google Scholar]
- 6.Do Amaral RJ, Almeida HV, Kelly DJ, O’Brien FJ, Kearney CJ. Infrapatellar fat pad stem cells: From developmental biology to cell therapy. Stem Cells Int 2017;2017:6843727. [Google Scholar]
- 7.Reith JD, Bauer TW, Joyce MJ. Paraarticular osteochondroma of the knee: Report of 2 cases and review of the literature. Clin Orthop Relat Res 1997;334:225-32. [Google Scholar]
- 8.Evaniew N, Bayegan D, Popovic S, Parasu N, Ghert M. Infrapatellar fat pad osteochondroma: Three cases and a systematic review. J Knee Surg 2015;28:229-38. [Google Scholar]
- 9.Perry BE, McQueen DA, Lin JJ. Synovial chondromatosis with malignant degeneration to chondrosarcoma. Report of a case. J Bone Joint Surg Am 1988;70:1259-61. [Google Scholar]
- 10.Duri ZA, Aichroth PM, Dowd G. The fat pad. Clinical observations. Am J Knee Surg 1996;9:55-66. [Google Scholar]
- 11.Sakai H, Tamai K, Iwamoto A, Saotome K. Para-articular chondroma and osteochondroma of the infrapatellar fat pad: A report of three cases. Int Orthop 1999;23:114-7. [Google Scholar]
- 12.González-Lois C, García-de-la-Torre P, SantosBriz-Terrón A, Vilá J, Manrique-Chico J, Martínez-Tello J. Intracapsular and para-articular chondroma adjacent to large joints: Report of three cases and review of the literature. Skeletal Radiol 2001;30:672-6. [Google Scholar]
- 13.Oliva F, Marconi A, Fratoni S, Maffulli N. Extra-osseous osteochondroma-like soft tissue mass of the patello-femoral space. BMC Musculoskelet Disord 2006;7:57. [Google Scholar]
- 14.Rizzello G, Franceschi F, Meloni MC, Cristi E, Barnaba SA, Rabitti C, et al. Para-articular Osteochondroma of the Knee. Arthroscopy 2007;23:910.e1-4. [Google Scholar]
- 15.Carmont MR, Davies S, Gey van Pittius D, Rees R. Accelerated para-articular osteochondroma formation within the knee: A case report. Cases J 2008;1:6. [Google Scholar]
- 16.Singh VK, Shah G, Singh PK, Saran D. Extraskeletal ossifying chondroma in Hoffa’s fat pad: an unusual cause of anterior knee pain. Singapore Med J 2009;50:e189-92. [Google Scholar]
- 17.Ogura K, Goto T, Nemoto T, Imanishi J. Para-articular osteochondroma of the infrapatellar fat pad. J Knee Surg 2011;24:209-13. [Google Scholar]
- 18.Nouri H, Ben Hmida F, Ouertatani M, Bouaziz M, Abid L, Jaafoura H, et al. Tumour-like lesions of the infrapatellar fat pad. Knee Surg Sports Traumatol Arthrosc 2010;18:1391-4. [Google Scholar]
- 19.Mulcahy H, Hoch B. An extraskeletal para-articular osteochondroma of Hoffa’s fat pad. Radiol Case Rep 2010;5:420. [Google Scholar]
- 20.De Maio F, Bisicchia S, Potenza V, Caterini R, Farsetti P. Giant intra-articular extrasynovial osteochondroma of the knee: A report of two cases. Open Orthop J 2011;5:368-71. [Google Scholar]
- 21.Park JH, Park JH, Lee AH, Lee DH. An unusual presentation of Hoffa's disease in an elderly patient with no trauma history: A case report. Acta Orthop Traumatol Turc 2011;45:195-9. [Google Scholar]
- 22.Sen D, Satija L, Kumar KS, Rastogi V, Sunita BS. Giant intra-articular extrasynovial osteochondroma of the Hoffa’s fat pad. Med J Armed Forces India 2015;71:S8-11. [Google Scholar]
- 23.Singh R, Jain M, Siwach R, Rohilla S, Sen R, Kaur K. Large para-articular osteochondroma of the knee joint: A case report. Acta Orthop Traumatol Turc 2012;46:139-43. [Google Scholar]
- 24.Sourlas I, Brilakis E, Mavrogenis A, Stavropoulos N, Korres D. Giant intra-articular synovial osteochondromata of the knee. Hippokratia 2013;17:281-3. [Google Scholar]
- 25.Larbi A, Cyteval C, Hamoui M, Dallaudiere B, Zarqane H, Viala P, et al. Hoffa’s disease: A report on 5 cases. Diagn Interv Imaging 2014;95:1079-84. [Google Scholar]
- 26.Mozella AP, Da Silveira Moller JV, De Araújo Barros Cobra HA. Tumor formation in Hoffa’s infrapatellar fat: Case report. Rev Bras Ortop 2015;50:117-21. [Google Scholar]
- 27.Bombaci H, Bilgin E. Infrapatellar fat pad para-articular osteochondroma: A ten-year follow-up and review. Arch Trauma Res 2015;4:e28381. [Google Scholar]
- 28.Osteochondroma at its Rarest Site Case Report. 2015; Available from: https://www.jocr.co.in [Google Scholar]
- 29.Rajkumar N, Soundarrajan D, Dhanasekararaja1 P, Rajasekaran S. Learning Point of the Article: Para-articular Osteochondroma of Patella with Coexisting Osteoarthritis. Available from: https://www.jocr.co.in [Google Scholar]
- 30.Nishimura T, Saku I, Kanda S, Fukushima T, Akiyama T. Para-articular osteochondroma of the infrapatellar fat pad: A report of three cases. Int J Surg Case Rep 2020;69:105-8. [Google Scholar]
- 31.Panta S, Thapa SK, Paudel KP, Kandel M, Adhikari BR. Hoffa’s osteochondroma-para-articular extrasynovial infrapatellar fat pad osteochondroma: A case report. J Nepal Med Assoc 2021;59:799-801. [Google Scholar]














