The posterior approach with decompression and pedicle screw fixation is a less invasive procedure with better familiarity and promotes faster recovery with early mobilization in thoracolumbar spinal tuberculosis.
Dr. Shivank Khurana, Department of Orthopedic Surgery, Jawaharlal Nehru Medical College, Faculty of Medicine, Aligarh Muslim University, Aligarh - 202002, Uttar Pradesh, India. E-mail: sshivankhurana2@gmail.com
Introduction: Spinal tuberculosis (TB) is a significant health problem. While chemotherapy is the primary treatment, surgery is necessary in some cases. This study investigates the posterior approach for treating thoracolumbar spinal TB with neurological involvement.
Materials and Methods: This prospective observational study included 75 patients with thoracolumbar TB and neurological deficits. All underwent posterior decompression and stabilization using pedicle screw fixation. Pre and post-operative neurological status, pain scores, and kyphotic angle were assessed.
Discussion: The posterior approach demonstrated advantages over the traditional anterior approach. It facilitated decompression, improved neurological function, and corrected spinal deformity. Posterior fixation allowed early mobilization, reducing complications from prolonged bed rest. These findings align with previous research supporting the posterior approach for spinal TB.
Conclusion: The posterior approach with decompression and pedicle screw fixation is a safe and effective surgical method for thoracolumbar spinal TB with neurological involvement. It offers good clinical outcomes, minimizes complications, and facilitates faster patient recovery.
Keywords: Spinal tuberculosis, posterior approach, neurological deficit, kyphotic deformity, pedicle screw fixation.
From the dawn of history, tuberculosis (TB) influenced mankind. Hippocrates (469 B.C.), the father of medicine termed it “phthisis” which means to “dry up.” The disease was also known as “Captain of Men Death” and “The Great White Plague” [1]. TB is a public health problem in most of the countries. Approximately one-third of the world’s population is infected with Mycobacterium TB. Spinal TB occurs in 2% of all cases of TB. It is up to 15% of cases of extrapulmonary TB and 50% of cases of skeletal TB. Lower thoracic and lumber vertebra are most commonly involved but it may affect any part of the spine. Osteoarticular TB is the most common secondary infection with the primary lesion being in the lung, lymph node, or intestine [2]. Spinal TB is the most dangerous among bone and joint TB because it causes bone destruction, kyphotic deformity, severe neurological deficit, and paraplegia. Antitubercular chemotherapy is the mainstay of spinal TB treatment [2]. The aim of spinal TB surgery is debridement, decompression, circulation restoration, stability maintenance, deformity correction, and prevention of deformity progression. Various surgical approaches, such as anterior, combined anterior and posterior, and posterior alone approaches have been widely used for surgical management of spinal TB [3]. The anterior approach has its own disadvantages as it causes more morbidity to patients (compromises pulmonary function), requires more expertise for the surgery, has poor sagittal spinal correction, and is not so effective in the correction of pre-existing kyphosis. Besides this, there are problems regarding the stability of anterior fixation because concomitant osteoporosis associated with infection renders the vertebra structurally weak and may prevent adequate fixation [4, 5]. The combined anterior and posterior approach helps to mitigate stability-related problems of the anterior approach alone; however, it requires two surgeries which cause additional morbidity to the patient [4]. The posterior approach gained popularity in the past decade because it offers excellent exposure for spinal cord decompression and allows posterior instrumentation for deformity correction and stabilize the spine. Several authors stated that using the posterior approach along with debridement and fixation for managing spinal TB led to favorable clinical outcomes [6, 7]. However, posterior approach remains controversial because it may affect posterior spinal stability. The posterior approach has many advantages in comparison to anterior approach: Less morbid for the patient, Familiar to the spine surgeon, Universally applicable, Diaphragm and vessels can be preserved, Biomechanically superior posterior implants (specially pedicle screw constructs) as compared to anterior implants, for non-inflamed bone – implants have a good hold, longer lever arm for correction of deformities, avoids excessive removal of bone from the diseased anterior column that can result in creation of large defects [7-10]. The present study was undertaken with the aim to study the clinical, radiological, and functional outcome of the posterior approach (pedicle screw fixation ± decompression) for the treatment of thoracic and lumbar spine TB and to study the impact of posterior decompression and stabilization on correction of spinal deformity in thoracic and lumbar spine TB.
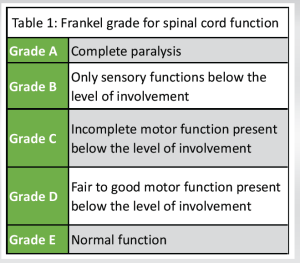
This is a prospective observational study. Seventy-five patients having thoracolumbar spine TB with neurological deficit or deformity presented to a tertiary care hospital in Northern India. Inclusion criteria included patients of thoracic and lumbar spinal TB having either limited improvement/no improvement even with anti-TB therapy for 4–6 weeks or having deteriorating neurology while undergoing conservative treatment or having kyphosis with active disease or progression of the kyphotic deformity. Patients with thoracic or lumbar spine TB without any neurological involvement or deformity or treated by other surgical approaches or having severe comorbidity and not fit for surgical intervention were not included in the study. Pre-operative evaluation included the detailed clinical history of the patient’s complaints, duration and progression of disease, and degree of neurological dysfunction. Examination encompassed inspection including curvature of the spine, midline furrow, paravertebral fullness, and palpation including local temperature, tenderness, and palpable gibbous/kyphus. Detailed Neurological examination was also carried out pre- and post-surgery and at follow-ups. The radiological examination included X-rays of spine anteroposterior and lateral views as well as magnetic resonance imaging. Laboratory investigations for basic pre-anesthetic check-ups and inflammatory markers, such as C-reactive protein and erythrocyte sedimentation rate were also done. Paraplegia grading (Frankel grading, association impairment scale) (Tables 1 and 2), visual analogue scale (VAS) for pain, and Cobb’s angle (Fig. 1) for kyphotic deformity and loss of kyphotic correction were also done.
Surgical procedure
After necessary pre-operative investigation and anesthesia clearance (pre-anesthesia checkup) all patients were operated under general anesthesia. Patients underwent posterior decompression and stabilization by pedicel screw fixation to promote neurological recovery and correction of deformity of the spine (Fig. 2). All the patients were operated in the prone position and posterior midline incision was practiced at the affected vertebral levels. Post-operative care involved bed rest, hourly change of posture by log rolling along with physiotherapy of all joints. Intravenous antibiotics were given for 3 days post-operatively followed by a shift to oral antibiotics. The drain was removed 24 h post-operatively followed by a check X-ray. Patients were mobilized on wheel wheelchairs with high Taylor braces after adequate pain relief. Stitches were removed on day 12th post-operatively. Patients were followed up every 4 weeks for 3 months and then every 12 weeks till the past follow-up. The neurological status of each patient was evaluated on initial presentation pre-operatively, at the time of discharge, and during subsequent follow-up visits.
75 patients of thoracic spine TB with neurological involvement were included in the study, out of which 25 patients (33.3%) were male and 50 patients (66.7%) were female with the mean age of presentation being 28.86 years (11–60). 60 Patients (80%) involved two vertebrae and 15 patients (20%) had more than two vertebrae involvement. Out of 75 patients, 60 had spastic paraplegia and 15 were having flaccid paraplegia. 25 out of 75 patients were of Frankel Grade A (complete paraplegia), 20 were of Grade B (sensory functions present), 25 were of Grade C (incomplete motor function present) and 5 were in Grade D (fair to good motor function present). Pre-operative VAS scores ranged from 3 to 6 with a mean of 4.8. Pre-operative kyphosis (Cobb’s angle) was from 11° to 55° with a mean of 28.8°. The total number of patients was 75 (50 females and 25 males). The average age of patients was 28.86 years (range 11–60 years). The mean follow-up duration was 9 months (range 2–21 months). Neurological improvement was seen in 55 patients (73.33%). 20 patients had no neurological recovery (26.6%). 15 out of these 20 patients (75%) were of flaccid paraplegia. Out of 25 patients of Grade A, 10 improved to Grade E, 5 improved to Grade D (Fig. 3), and 10 patients remained in Grade A. Out of 20 patients of Grade B, 10 improved to Grade E and 10 remained in Grade B. Out of 25 patients of Grade C, 10 improved to Grade D, and 15 improved to Grade E (Fig. 4). 5 patients of Grade D improved to Grade E (Table 3).
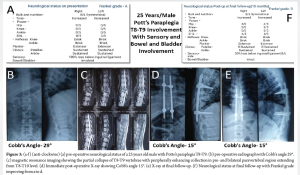
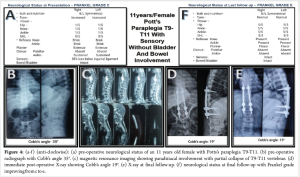
The mean pre-operative VAS was 4.8 (range 3–6), mean VAS at the final follow-up was 1.46 (range 0–3). The mean improvement in VAS was 3.34 (range 2–6). Pre-operative Cobb’s angle ranged from 11° to 55° with a mean of 28.8°. Post-operative Cobb’s angle ranged from 09° to 41° with a mean of 18.26°. The mean kyphotic correction was 10.64° (range 2°–44°). A total of 5 cases of complications were encountered. Post-operative septicemia and deep surgical site infection were seen in one patient (1.33%) (Fig. 5). Superficial surgical site infection was seen in two patients (2.66%). Two patients (2.66%) had implant loosening. No patient had implant breakage.
TB of the spine can be managed by conservative or surgical methods. The Conservative method comprises chemotherapy, bed rest with or without plaster casts, followed by resumption of activity with braces. It requires a long period of immobilization and leads to complications of prolonged recumbency, such as bed sore, chest infection, deep vein thrombosis, and kyphotic deformity progression that cannot be prevented. To avoid the problems associated with conservative management and when patients do not show signs of progressive recovery, neurological deterioration during conservative therapy, and advanced cases of paraplegia, surgery is indicated. For the debridement and decompression of Pott’s spine, various approaches are available, each having advantages and disadvantages [11, 12]. Hodgson and Stock in 1960 popularized anterior radical surgery. The anterior approach has various advantages, such as direct access to the disease to perform decompression, direct visualization of the area, and prevent the possible progression of the kyphotic deformity. The disadvantages of the anterior approach are higher morbidity and mortality associated with this approach. It has problems, such as chest infection, atelectasis, pneumothorax, post-operative ileus after surgical decompression, and an increase in spinal instability in the post-operative period [5]. Oga et al. studied the adherence capacity of the pathogen (Mycobacterium TB) to stainless steel and concluded that there is negligible adherence and it is safe to use implants in the regions with active TB infection unlike pyogenic organisms the tubercle bacilli do not form any biofilm and adhere to metal [13]. Guven and co-workers used a pedicle screw or hook system for posterior instrumentation for 10 patients with TB of the thoracolumbar spine. They found clinical and radiological evidence of stable fusion in all their patients [7]. In this study, we used posterior decompression and transpedicular screws for fixation because it has been proven to be a good method for stabilizing the thoracic and lumbar spine. It is not as radical as that of the anterior approach. During instrumentation of the pedicle screws in the thoracic spine, we inserted the screws into the healthy pedicles adjacent to the areas of bone destruction. There is a quick relief of instability in patients treated for spinal TB with transpedicular instrumentation. The posterior approach has the advantage that it avoids contact with the infectious focus because the tuberculous infection usually involves the anterior column. The transpedicular instrumentation maintains the spinal alignment and stabilizes the involved vertebra. The posterior instrumentation acts as a spacer allows the healing of the involved anterior part and supports the anterior column. Posterior instrumentation has been very effective in preventing the progression of kyphosis. The main advantage of posterior instrumentation is that it can provide good fixation through posterior elements as the disease pathology is anterior. Correction of pre-existing kyphosis can be effectively done by posterior fixation. Lee et al. study concluded that transpedicular instrumentation offers quick relief of instability. It also avoids late angular deformity in patients with thoracolumbar and lumbar spine TB who had minimal (50%) bone loss. In addition to stable posterior instrumentation, spinal cord decompression is conducted under clear vision. It can be extended above and below if multiple-level fixation is needed. The cord was decompressed by excising spinous process and lamina to allow access to the cord. The debridement was done for decompression of the cord without creating a large defect. The posterior instrumentation allows early mobilization, thus avoiding the complications of prolonged recumbency [14]. In our study, 75 patients with thoracolumbar spinal TB with neurological involvement were operated. Neurological improvement was seen in 55 patients (73.33%) and 20 patients had no neurological recovery (26.6%), fifteen out of these twenty patients (75%) who did not recover were of flaccid paraplegia. In a study done by Guzey et al., out of 8 patients with neurological deficits seven had improvement in neurological status and one patient did not recover (American Spinal Injury Association Grade C) [6]. In a study done by Lee et al., out of 7 patients with a neurological deficit three had improvements in Frankel grades. Three patients remained in Grade D and one patient deteriorated from Grade E to Grade D [15]. Rawall et al. studied 67 patients in which single-stage all posterior surgery was done and followed up for 31.37 months. Out of 38 patients with neurological deficits, 8 improved by 3 Frankel grades, 16 improved by 2 Frankel grades, and 10 improved by 1 Grade. Two patients deteriorated by 1 Grade [16]. Post-operatively patients had significant relief in pain which was recorded on a VAS. In our study mean pre-operative VAS score was 4.8 (range 3–6) and the mean VAS score at the final follow-up was 1.46 (range 0–3). The mean improvement in VAS score was 3.34 (range 2–6). In a study by Guzey et al., only three out of 19 patients experienced intermittent back or low-back pain at the time of the past follow-up examination. In a study done by Lee et al., on 10 patients, the mean pre-operative VAS was 7.28 ± 1.21 which decreased significantly to an average of 2.56 ± 1.03 after surgery. Reduction of kyphosis was seen in all patients and recorded as Cobb’s angle. In our study pre-operative Cobb’s angle ranged from 11°–55° with a mean of 28.8° and post-operative Cobb’s angle was from 09°–41° with a mean of 18.26°. The mean kyphotic correction is 10.64° (2°–44°). At the final follow-up average kyphotic angle was 20.73° (9–41°) and the mean loss of correction was 2.47°. In the study done by Guzey et al., mean angulation measured in 13 patients with kyphotic deformity was 18.2° (range 5–42°) pre-operatively, which was reduced to 17.3° (range 0–42°) post-operatively. 2.8° loss of correction (range 2–5°) was seen after 44.3 months at the final follow-up. In the study of Lee et al., the mean pre-operative kyphotic angle of 19.91° was reduced to 14.89° after surgery (25.3% correction). At the past follow-up, the mean kyphotic angle was 20.29° and the correction loss was 5.40°. Post-operative septicemia and deep surgical site infection were seen in one patient (1.33%) for which debridement was done and the wound healed after secondary closure was done at 5 weeks post-operatively. This patient had complete neurological recovery from Frankel Grade A to Grade E. Superficial infection at the surgical site was seen in two patients (2.66%) who recovered with daily dressing. Two patients (2.66%) had implant loosening and there was no implant breakage. Guzey et al. studied 19 patients out of which one patient suffered a superficial infection of a wound that was treated successfully with antibiotic therapy. One patient died due to myocardial infarction 10 days after surgery. A pedicle screw was broken in one patient. In the study of 67 patients by Rawall et al., in 65 patients the surgical wounds healed normally, whereas in two patients by secondary intention. Two cases of deep infections needed debridement and implant removal. The other two patients needed revision of instrumentation (1 each for proximal and distal kyphosis). Apart from these, 6 superficial infections and 2 cerebrospinal fluid leaks were managed conservatively.
The posterior approach (decompression and pedicel screw fixation) for the treatment of Pott’s spine gives reasonable access for adequate decompression of the cord and is less morbid avoiding problems associated with thoracotomy. It provides better functional outcomes (neurological recovery) and relief of pain. In posterior decompression and stabilization by pedicel screw fixation, there is significantly better kyphosis correction and maintenance. It facilitates early mobilization of patients and avoids problems of prolonged recumbency. Moreover, the posterior approach is preferred because of its familiarity to surgeons and low complication rate.
For surgeons treating patients with thoracolumbar spinal TB and neurological deficits, this study emphasizes the posterior approach with decompression and pedicle screw fixation as the go-to surgical technique which offers significant advantages over the traditional anterior approach. It minimizes surgical invasiveness, improving patient recovery and comfort. Most importantly, the posterior approach effectively decompresses the spinal cord, leading to better neurological outcomes. Furthermore, it allows for the correction of spinal deformity while minimizing complications associated with prolonged bed rest by facilitating early patient mobilization.
References
- 1.Ananthanarayanan R, Jayaram Panikar CK. Textbook of Microbiology. 7th ed., Ch. 39. Hyderabad: Orient Blackswan; ???. [Google Scholar]
- 2.Krishnamoorthy R, Taore VK, Salya RS. Pott’s paraplegia. Indian J Orthop 1975;9:6-12. [Google Scholar]
- 3.Arct MW. Operative treatment of tuberculosis of the spine in old people. J Bone Joint Surg Am 1968;50:255-67. [Google Scholar]
- 4.Chen WJ, Wu CC, Jung CH, Chen LH, Niu CC, Lai PL. Combined anterior and posterior surgeries in the treatment of spinal tuberculous spondylitis. Clin Orthop Relat Res 2002;398:50-9. [Google Scholar]
- 5.Hodgson AR, Stock FE, Fang HS, Ong GB. Anterior spinal fusion. The operative approach and pathological findings in 412 patients with Pott’s disease of the spine. Br J Surg 1960;48:172-8. [Google Scholar]
- 6.Guzey FK, Emel E, Bas NS, Hacisalihoglu S, Seyithanoglu MH, Karacor SE, et al. Thoracic and lumbar tuberculous spondylitis treated by posterior debridement, graft placement, and instrumentation: A retrospective analysis in 19 cases. J Neurosurg Spine 2005;3:450-8. [Google Scholar]
- 7.Guven O, Kumano K, Yalçin S, Karahan M, Tsuji S. A single stage posterior approach and rigid fixation for preventing kyphosis in the treatment of spinal tuberculosis. Spine (Phila Pa 1976) 1994;19:1039-43. [Google Scholar]
- 8.Pang X, Shen X, Wu P, Luo C, Xu Z, Wang X. Thoracolumbar spinal tuberculosis with psoas abscesses treated by one-stage posterior transforaminal lumbar debridement, interbody fusion, posterior instrumentation, and postural drainage. Arch Orthop Trauma Surg 2013;133:765-72. [Google Scholar]
- 9.Zhang HQ, Li JS, Zhao SS, Shao YX, Liu SH, Gao Q, et al. Surgical management for thoracic spinal tuberculosis in the elderly: Posterior only versus combined posterior and anterior approaches. Arch Orthop Trauma Surg 2012;132:1717-23. [Google Scholar]
- 10.Sundararaj GD, Behera S, Ravi V, Venkatesh K, Cherian VM, Lee V. Role of posterior stabilisation in the management of tuberculosis of the dorsal and lumbar spine. J Bone Joint Surg Br 2003;85:100-6. [Google Scholar]
- 11.Tuli SM. Results of treatment of spinal tuberculosis by “middle path regime”. J Bone Joint Surg Br 1975;57:13-23. [Google Scholar]
- 12.Wilkinson MC. Tuberculosis of the spine treated by chemotherapy and operative debridement. A long-term follow-up study. J Bone Joint Surg Am 1969;51:1331-42. [Google Scholar]
- 13.Oga M, Arizono T, Takasita M, Sugioka Y. Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Clinical and biologic study. Spine (Phila Pa 1976) 1993;18:1890-4. [Google Scholar]
- 14.Lee TC, Lu K, Yang LC, Huang HY, Liang CL. Transpedicular instrumentation as an adjunct in the treatment of thoracolumbar and lumbar spine tuberculosis with early stage bone destruction. J Neurosurg 1999;91:163-9. [Google Scholar]
- 15.Lee SH, Sung JK, Park YM. Single-stage transpedicular decompression and posterior instrumentation in treatment of thoracic and thoracolumbar spinal tuberculosis: A retrospective case series. J Spinal Disord Tech 2006;19:595-602. [Google Scholar]
- 16.Rawall S, Mohan K, Nene A. Posterior approach in thoracolumbar tuberculosis: A clinical and radiological review of 67 operated cases. Musculoskeletal Surg 2013;97:67-75. [Google Scholar]
















