Patients with femur fractures are likely to seek non-medical forms of treatment due to the socioeconomic constraints and this can lead to malunion along with knee stiffness and shortening, presenting a great challenge for orthopedic surgeons and can be successfully managed with one-stage open nailing, either with or without bone resection, achieving an excellent outcome.
Dr. Nilesh S Sakharkar, Department of Orthopaedics, Government Medical College and Hospital, Nagpur, Maharashtra, India. E-mail: orthodrnilesh@gmail.com
Introduction: Most patients with these injuries are taken to hospitals frequently for specialized orthopedic treatment. However, because quackery is a common practice in the many regions, it is common in underdeveloped nations, particularly in rural India, for these injuries to be initially overlooked. This study aimed to assess the efficacy of open intramedullary nailing in the treatment of patients with neglected bilateral fracture shaft femurs in terms of union achievement and functional outcomes.
Case Report: The first presentation was a 27-year-old male patient with bilateral untreated malunited shaft femur fractures that had occurred 10 months prior. The patient had a history of a car accident that resulted in bilateral shaft femur fractures. We aimed to treat both fractures simultaneously in a single setting with open reduction and femoral nailing. The patient has followed up for 10 months after surgery with full weight bear walking without support and can sit cross legged and squat.
Conclusion: The prognosis is typically poorer for neglected femoral shaft fractures than for those that are treated immediately. Any surgeon who works in low facilities setting needs to be aware of difficulties in the management of neglected or non-union shaft femur fracture.
Keywords: Neglected, quackery, open reduction, malunion.
The most frequent fractures seen in the field of orthopedics are femoral diaphyseal fractures. Bilateral shaft femur fracture results from high-energy trauma account for 2% to 7% of all femur fractures, and these fractures are more likely to result in systemic complications, the need for resuscitation, and mortality [1]. Considering the largest bone in the body and one of the most important weight-bearing bones in the lower limb, femur fractures can result in prolonged morbidity and severe impairment if specific management has not been given. Most femur fracture patients have misalignment, shortening of the limb, and stiffness in the knee because they prefer non-operative therapy from traditional bone setters, who typically treat these fractures with insufficient splinting and local ayurvedic fromulation applications. Due to quackery malpractice, patients’ lack of knowledge, and low socioeconomic status, we encountered malunited femur fractures in our country’s population. The course of treatment has changed throughout time, evolving from non-operative immobilization techniques to open reduction and plate fixation, unlocked intramedullary nailing, and finally locked intramedullary nailing [2-4]. The majority of acute femoral shaft fractures are currently treated with closed interlocking intramedullary nailing, and numerous studies have proven this approach to be beneficial over time [1-5]. Nevertheless, there are several circumstances such as old neglected fractures in which closed reduction and nailing may not be an option due to the overriding of fracture ends, interposition of soft tissue, and callus formation around the fracture site. Open reduction and interlocking nailing are the treatment of choice in neglected cases of femur fractures as it helps in anatomical reduction, proper realignment of fragments, rotational deformity correction, and canal preparation in the sclerotic fracture ends. Furthermore, acute lengthening is associated with neurovascular complications; therefore, sequential surgery or pre-operative traction is needed in cases of gross overriding. Even though single-stage open nailing has been documented using selective bone excision and manual traction without prior skeletal traction.
A 10-month-old bilateral untreated malunited shaft femur fracture in a 27-year-old male patient was the initial presentation. The patient had a history of a car accident that resulted in bilateral shaft femur fractures. Following this, the patient visited a local bone setter where local herbs were applied repeatedly. After 10 months, a patient came to our facility with shortening of the limbs, deformities, and inability to sit cross-legged, squat, or walk. An anteroposterior and lateral view radiograph of each lowered limb was used to assess the patient. Huge overriding with callus formation and sclerotic fracture ends are shown on X-rays (Fig. 1a, b, c, d).
We aimed to treat both fractures simultaneously in a single setting. Right lateral decubitus positioning was given after epidural anesthesia. Since there was greater overlapping on the left side, we started operating the left side first. The fracture site was made visible, and the callus around it was removed and preserved for later insertion. Fibrous tissue was removed to expose the fracture ends. Sclerotic bony ends were cut off with a saw and fracture margins were freshened with nibbler and curette till the bleeding ends were confirmed. The medullary canal was first opened by drilling, followed by sequential reaming of proximal and distal ends. With the hip in flexion and adduction, a sharp reamer was used to create the entry portal for the nail in a retrograde fashion. From the entry portal to a point just proximal to the fracture site, a guidewire was introduced. Bone-holding clamps were used to hold both fracture ends together while angulation was used to approximate them. While maintaining this position, a guidewire was placed into the distal fragment, and reduction was carried out gently to allow the soft tissues to stretch out. End-to-end fracture reduction carried with manual traction and leverage of bony ends. Through the entry point, a femur interlocking nail of appropriate size was inserted. Alignment, axial stability, and rotation were checked. Proximal and distal locking was done under C-arm guidance. Knee joint manipulation was done to gain the range of motion. The wound was thoroughly lavaged, and the callus that had previously been removed was put into the fracture site. A suction drain was left in place, and the wound was closed in layers. The patient was then shifted to a left lateral decubitus position so that the second side could be operated. The same procedure used for the right-side femoral shaft was also applied to the left side.
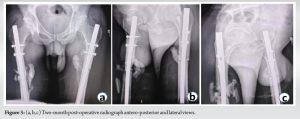
For this patient, the standard post-operative treatment protocol was used. After 48 h, the drains were taken out, and post-operative AP and lateral radiographs were taken (Fig. 2a and b). Knee mobilization and toe touch weight bearing with walker support were started. The hospital stay was 10 days. The patient was informed about the weight-bearing protocol and physiotherapy treatment at the time of discharge. After 15 days following surgery, the sutures were removed. Following surgery, the patient was asked to follow-up every 2 weeks for the first 3 months and then once a month for a year (Fig. 3a, b, c).
Standard AP and lateral radiographs of the femur were taken at the subsequent visit, and the range of motion of the knee was evaluated. Progressive weight bearing was done in accordance with the callus formation that was seen on radiographs. Walking aids were discontinued 4–6 weeks postoperatively. At 10 months follow-up, X-rays showed tremendous callus formation and union around the fracture site and the patient was able to sit cross-legged, squat, and walk with full weight bearing without any support(Fig. 4-6).


Bilateral malunited femoral shaft fractures not only look undesirable but can also cause significant physical impairment. Even though they are typically functionally compatible, they still pose a huge challenge to an orthopedic surgeon when they need to be fixed. Even though they are uncommon in developed countries, neglected femur shaft fractures are widespread in developing countries, particularly in rural regions. Poor socioeconomic status, illiteracy, and the widespread use of quacks and traditional bone setters are the main causes of this issue [5, 6]. The majority of these fractures can be stabilized with intramedullary nail or plate osteosynthesis with or without bone grafting. Some surgeons prefer to perform it in a single stage, while others favor a two-stage procedure (soft tissue release followed by traction in the first stage and definitive treatment in the second stage) [7]. Femoral diaphyseal fractures are treated effectively by intramedullary nailing with almost universally excellent results [8-10]. While closed interlocking intramedullary nailing is the preferred treatment for most fresh femoral shaft fractures, it is not effective in neglected cases due to factors such as soft tissue interposition, bone overriding, and the formation of fibrous tissue around the fracture site. In addition, there is an associated knee joint stiffness in these patients, which needs to be managed. In such situations, restoring knee function remains a functional challenge that necessitates extensive, well-supervised physical treatment. Neglected cases of femur shaft fracture are treated with internal fixation using interlocking intramedullary nailing and open reduction. These patients benefit from open nailing because it is simpler to achieve absolute anatomical reduction, precise interdigitation of the fracture fragments improves rotational stability, ease of opening the medullary canals of the sclerotic bone, and a very low incidence of rotational mal-alignment. As a result, as shown by numerous studies, open reduction and internal fixation with intramedullary interlocking nailing is now thought to be the preferred treatment for neglected femoral shaft fractures [7, 11-13].
For orthopedic surgeons working in settings with limited resources, treating non-unions and malunions of femoral shaft fractures is a significant problem. When femoral shaft fractures are neglected, the prognosis tends to be worse than when the fractures are managed immediately. Any surgeon who comes to work in this type of environment needs to be aware of these difficulties. It is essential to establish facilities for the timely closed nailing of femoral shaft fractures in resource-limited areas and to ensure that orthopedic care is accessible to the economically disadvantaged.
Malunited femoral shaft fractures not only appear terrible but also can cause significant physical impairment. When they need to be corrected, even though they are often compatible with function, orthopedic surgeons have an immense challenge. Most of these fractures can be fixed with open reduction and internal fixation using intramedullary nail or plate osteosynthesis, either with or without bone grafting, in one-stage or two-stage procedures.
References
- 1.Denisiuk M, Afsari A. Femoral shaft fractures. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar]
- 2.Brumback RJ, Ellison PS Jr., Poka A, Lakatos R, Bathon GH, Burgess AR. Intramedullary nailing of open fractures of the femoral shaft. J Bone Joint Surg Am 1989;71:1324-31. [Google Scholar]
- 3.Christensen NO. Küntscher intramedullary reaming and nail fixation for non-union of fracture of the femur and the tibia. J Bone Joint Surg Br 1973;55:312-8. [Google Scholar]
- 4.Christie J, Court-Brown C, Kinninmonth AW, Howie CR. Intramedullary locking nails in the management of femoral shaft fractures. J Bone Joint Surg Br 1988;70:206-10. [Google Scholar]
- 5.Boopalan PR, Sait A, Jepegnanam TS, Matthai T, Varghese VD. The efficacy of single-stage open intramedullary nailing of neglected femur fractures. Clin Orthop Relat Res 2014;472:759-64. [Google Scholar]
- 6.Onuminya JE. The role of the traditional bonesetter in primary fracture care in Nigeria. S Afr Med J 2004;94:652-8. [Google Scholar]
- 7.Mukherjee SK, Jain V. Neglected femoral diaphyseal fracture. Clin Orthop Relat Res 2005;431:72-9. [Google Scholar]
- 8.Canadian Orthopaedic Trauma Society. Nonunion following intramedullary nailing of the femur with and without reaming. Results of a multicenter randomized clinical trial. J Bone Joint Surg Am 2003;85:2093-6. [Google Scholar]
- 9.Kanellopoulos AD, Yiannakopoulos CK, Soucacos PN. Closed, locked intramedullary nailing of pediatric femoral shaft fractures through the tip of the greater trochanter. J Trauma 2006;60:217-22; discussion 222-3. [Google Scholar]
- 10.Wolinsky PR, McCarty E, Shyr Y, Johnson K. Reamed intramedullary nailing of the femur: 551 cases. J Trauma 1999;46:392-9. [Google Scholar]
- 11.Akinyoola L, Orekha O, Odunsi A. Open intramedullary nailing of neglected femoral shaft fractures: Indications and outcome. Acta Orthop Belg 2011;77:73-7. [Google Scholar]
- 12.Gahukamble A, Nithyananth M, Venkatesh K, Amritanand R, Cherian VM. Open intramedullary nailing in neglected femoral diaphyseal fractures. Injury 2009;40:209-12. [Google Scholar]
- 13.Mahaisavariya B, Laupattarakasem W. Late open nailing for neglected femoral shaft fractures. Injury 1995;26:527-9. [Google Scholar]