1.5-stage total hip arthroplasty with custom-made articulating spacers (CUMARS) is a viable management option for destructive hip septic arthritis with benefits of effective infection eradication, good functional outcomes, cost-effectiveness with reduced physical and psychological burden in avoiding a second operation, yet not precluding the possibility of a two-stage exchange THA if required.
Lim Hui-Shan Angela, Department of Orthopedics Surgery, Changi General Hospital, Singapore, Mailing Address: 2 Simei Street 3, Singapore. E-mail: angelalhs1298@gmail.com
Introduction: Prompt diagnosis and management of septic arthritis are pivotal for early infection eradication, joint preservation, and prevention of quality-of-life impact consequences. Total hip arthroplasty has been introduced for the management of severe destructive septic arthritis with the aims to eradicate infection while preserving hip function. Few case studies have been done on two-stage exchange total hip arthroplasty for treatment of native hip septic arthritis using prosthesis with antibiotic-loaded acrylic cement articulating spacer with generally good outcomes. However, a small percentage of patients electively chose not to proceed with the second-stage exchange arthroplasty. Therefore, 1.5-stage total hip arthroplasty was considered a viable option; however, it has only been established in periprosthetic infection management, but not in native hip septic arthritis. Custom-made articulating spacers are considered an ideal option as has no constraints, are more readily available, and were designed to be a functional single-stage spacer that can remain permanent yet not preclude the possibility of a second-stage exchange surgery if required. Overall, this led to the consideration of 1.5-stage total hip arthroplasty using custom-made articulating spacers for the management of chronic destructive hip septic arthritis.
Case report: We report a 67-year-old patient with functional decline from fully independent without aids to chairbound over 8 months. Work-up revealed raised inflammatory markers and bilateral destructive hip septic arthritis. He underwent bilateral 1.5-stage total hip arthroplasty with antibiotic-loaded custom-made articulating spacers. One-year post-operation, he remains infection-free and is progressing well with rehabilitation – ambulating independently with walking frame.
Conclusion: Management of septic arthritis varies largely depending on infection duration, activity level, and extent of joint destruction. In significantly destructed hip septic arthritis, 1.5-stage total hip arthroplasty using antibiotic-loaded custom-made articulating spacer is a viable option with the benefits of effective infection eradication, good functional outcomes, cost-effectiveness, reduced physical and psychological burden in avoiding a second operation, all whilst not precluding the possibility of a second-stage exchange arthroplasty if required with ease.
Keywords: Septic arthritis, hip, infection, custom-made articulating spacer, antibiotic cement.
Management of destructive and recalcitrant hip septic arthritis (SA) can be complicated and remains controversial. In these cases, there is osteomyelitis of the acetabulum and proximal femur resulting in the destruction of articular cartilage and underlying bone with significant joint deformity. Conventionally, resection arthroplasty was the treatment of choice for effective infection control; however, patients often have chronic joint pain, limb length discrepancy, inability to weight bear on the affected limb, and significantly poor functional results [1]. Therefore, total hip arthroplasty (THA) has been introduced in the past decade as a new therapeutic surgical treatment.
Both 1.5-stage and 2-stage exchange arthroplasty has been established as viable treatment options for infected THA that controls infection and improves pain and function [2]. Studies on 2-stage exchange THA for primary destructive hip SA are limited. Two case series by Fleck et al. and Younger et al. studied a subset of fourteen and sixty-one patients, respectively [3,4], both using prosthesis with antibiotic-loaded acrylic cement (PROSTALAC) articulating spacer (Depuy, Warsaw, Indiana) and reported 14.2% and 3% of the patients electing to keep their adequately functional spacer. Infection was controlled in majority of these patients, except a single case reported by Fleck et al. [3] and three cases reported by Younger et al. [4]. To our knowledge, 1.5-stage THA has only been described in infected THA but not in the context of native hip SA. Tsung et al. described a 1.5-stage THA using custom-made articulating spacer (CUMARS) in infected THA where 44.7% of patients kept a spacer that was functional [5]. This provides the benefit of avoiding a second surgery, yet not precluding the surgeon from performing a two-stage exchange THA as the articulating spacer can be left in situ for as long as possible until the spacer loosens, implant fails, or infection recurs. CUMARS system includes the Exeter Femoral stem (Stryker, Mahwah, NJ, USA) and a polyethylene acetabular liner [5]. Overall, this led us to consider antibiotic-loaded CUMARS in a 1.5-stage operation as a viable option in the context of native hip SA with the benefit of infection eradication, functional weight bearing, whilst not precluding the possibility of a 2-stage revision arthroplasty with ease. We describe a novel technique using antibiotic-loaded CUMARS in a 1.5-stage THA in the management of a case of chronic destructive SA in bilateral hip joints.
A 67-year-old male was admitted three times under various specialties over a span of 8 months. He was pre-morbidly independent in Activities of Daily Living (ADL) and community ambulant without aids. Significant past medical history includes diabetes mellitus, hypertension, hyperlipidemia, and ischemic heart disease with heart failure with reduced ejection fracture. Others include prostate cancer status post-robot-assisted radical prostatectomy, and he remains in remission till date. He was first admitted for a 4-month history of unintentional weight loss, borderline blood pressure, and functional decline since his prostate cancer resection surgery. Laboratory tests revealed serum white blood cell count of 21.39× 109/L, C-reactive protein level of 122.7 mg/L, and procalcitonin level of 0.58 ug/L. A computed tomography scan of the thorax, abdomen, and pelvis (CT TAP) (Fig. 1) done for source identification incidentally revealed mild non-specific right hip effusion. X-rays appeared normal (Fig. 2). Without inflammatory symptoms, he was diagnosed to have right hip osteoarthritis and was discharged after 2-week hospitalization. At this time, no additional assessment or orthopedic referral was done to rule out the possibility of SA.
Over 5 months, he continued to functionally decline and was mostly bedbound. He was re-admitted due to a fall secondary to lower limb weakness, right worse than left. Physical examination revealed right lower limb shortening and limited hip ranging with mild tenderness. X-rays revealed right hip destruction involving the superior acetabulum with superior subluxation and left hip degenerative changes (Fig. 3). An orthopedic review was requested and magnetic resonance imaging (MRI) of the pelvis and right hip showed evidence of bilateral hip effusion, worse on the right, with joint effusion partially decompressing into periarticular soft tissues (Fig. 4). In addition, there was acute osteomyelitis of the right acetabulum and femoral head with bony destruction and subluxation. Blood cultures grew pseudomonas aeruginosa. Ultrasound-guided right hip joint aspiration and core biopsy yielded no bacteria despite holding off antibiotics. Intravenous (IV) tazocin was started for pseudomonas bacteremia coverage.

For infection eradication, he underwent bilateral arthrotomy, debridement, synovectomy, and washout through an anterior-based muscle-sparing (ABMS) approach. Intra-operative cultures yielded pseudomonas aeruginosa and he received organism-specific IV ciprofloxacin daily for 2-week post-surgery, followed by oral ciprofloxacin for 6 more weeks. Post-operatively, despite improvement of his hip pain, he remained bedbound requiring assistance for transfers.
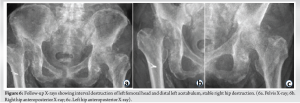
2 months post-operatively, repeat MRI revealed interval progression of SA worse over the left hip (Fig. 5). Inflammatory markers remained raised with serum white blood cell count of 15.7× 109/L and C-reactive protein level of 28.6 mg/L. Interval X-rays showed left hip progressive destruction while the right hip remained grossly stable since last discharge (Fig. 6). He was re-admitted for repeat bilateral hip joint washout, synovectomy debridement and a 1.5-stage antibiotic-loaded THA with CUMARS through ABMS approach in a single setting. An anterior-based approach was chosen to preserve soft tissue and muscle and reduce the risk of dislocation after THA. The surgery was performed under general anesthesia in lateral decubitus position. Intra-operative right hip findings include recalcitrant SA and osteomyelitis with synovitis and no purulent fluid, false acetabulum with Paprosky 3A bone loss, and subluxation more than 3 cm. Meanwhile, intra-operative left hip findings include SA with synovitis with no purulent fluid, deformed and unhealthy femoral head, and superolateral acetabular wall containing bone loss with superior wall intact. The damaged femoral head and neck were excised. Meticulous and radical debridement was performed to remove remnant infective tissues. The acetabulum was debrided using an acetabular reamer. Five tissues from each side were taken and sent for culture. Before reconstruction, the surgical site was re-draped and surgical team re-gowned with new sets of surgical instruments. The articulating spacers for the right hip were prepared using a Stryker RimFit cup 50 mm OD 32 mm ID, Stryker LFIT V40 femoral head 32 mm OD, +4 offset, and Exeter V40 cemented hip stem 35.5 offset stem length 125 mm stem length. The articulating spacers for the left hip were prepared using a Stryker RimFit cup 52 mm OD 36 mm ID, Stryker LFIT V40 femoral head 36mm OD, 0 offset, and Exeter V40 cemented hip stem 35.5 offset stem length 125 mm stem length (Stryker NY). 2g of ceftazidime was added to each packet of Palacos cement. Due to the significant amount of acetabulum bone loss for the right hip, an additional 2×3.5 cm cancellous screw was inserted to the superior acetabular wall defect. At the end of each section of the surgery, first being wound debridement and joint washout with subsequent 1.5-stage THA, the hip was irrigated with copious amounts of normal saline, chlorhexidine subsequently soaked in 9mls of 10% iodine mixed with 250 ml of normal saline. Intra-operative cultures revealed no bacterial growth. Post-operatively, he completed 2 more weeks of oral ciprofloxacin and was allowed to full weight bear immediately. However, his rehabilitation recovery was slow due to sarcopenia from prolonged functional decline and bedrest. On 1-month review, he was able to ambulate with walking frame with minimum assistance. There was no clinical or biochemical evidence of recurrent infection with serum white blood cell count of 9.1 × 109/L, C-reactive protein level of 0.9 mg/L. On 1-year review, he was he is able to ambulate with walking frame independently (Fig. 7) and there was no clinical evidence of infection recurrence. Overall, post-operative X-rays done on day 0, 1-month, and 1-year review revealed stable bilateral hip replacement prostheses with no evidence of periprosthetic fractures or loosening (Fig. 8).

Conventionally, hip SA with significant joint destruction was managed with resection hip arthroplasty for infection eradication, although with poor functional outcomes [6]. To allow for satisfactory clinical and functional outcomes while ensuring infection eradication, two-stage THA is currently considered the treatment of choice [7]. In a 2-stage THA, the first step can be resection arthroplasty or the implantation of an antibiotic-loaded hip spacer with the former having significantly poorer outcomes. However, patients with chronic destructive SA tend to have multiple comorbidities, are deconditioned, and may be unfit or unwilling to undergo a second surgery. Hipfl et al. reported the result of largest series of two-stage THA after resection arthroplasty for destructive hip SA [8] of which 33% have treatment failure with a considerable number of patients who failed to undergo definitive THA. In addition, resection hip arthroplasty in the first stage can lead to muscle contractures, pain, further deconditioning, poor functional result and hamper reimplantation surgery at the second stage. In contrast, few papers studied two-stage THA using antibiotic-loaded hip spacer as the first stage has been proven to be effective in infection eradication with success rates ranging from 92 to 100% while providing excellent functional outcomes [7]. Antibiotic-loaded spacers offer the advantage of distributing highly concentrated antibiotics to a localized area while maintaining the joint space and soft tissue tension for future component reimplantation [9]. However, high rates of cement spacer-related complications have been reported, including spacer migration, dislocation, and spacer fracture [10]. Hence, the strength of the spacer is important and must be able to resist stress and shear force. The ideal operation for this group of patients is one that can achieve high infection eradication rates while preserving hip function and potentially avoiding a second operation. In avoiding a second operation with a 1.5-stage THA, it is more cost effective, provides satisfactory functional outcomes, and eliminates the physical and psychological burden of a repeat operation [11]. This is an important consideration, especially in frail patients with multiple comorbidities. However, in the unfortunate context of spacer-related complications or infection recurrence, it is ideal to have the option of a second-stage exchange THA. PROSTALAC and CUMARS are both possible antibiotic-loaded spacer options. CUMARS was first described in 2001, and it includes using the readily available cemented hip system as a “long-term spacer” [5] while PROSTALAC was designed to remain in situ short term thereafter requiring a second surgery for implantation of a permanent THA prosthesis [12, 13]. This gives CUMARS the benefit of a 1.5-stage THA and has been reported to have better inter-stage functionality, easier removal, and good infection eradication, all whist allowing for a second-stage exchange THA if required [14, 15]. In addition, PROSTALAC is a semi-constrained implant that has the benefit of stability but risk of increased stress on the prosthesis and bone interface unlike CUMARS which is a THA without constraints. Lastly, PROSTALAC has limited sizes unlike CUMARS which is also more common and readily available. At present, in the literature, both 1.5-stage THA and CUMARS have only been described in the context of PJI, which has been shown to be an effective management option [2, 5, 14, 15]. In the future, the use of 1.5-stage THA with CUMARS in the context of native hip SA would be advantageous for effective infection eradication, cost-effectiveness, and reducing physical and psychological burden in avoiding a potential second surgery, yet not precluding the surgeon from performing a two-stage exchange THA with ease if required. However, this procedure requires experience to address the deformities and poor bone stock caused by the SA. To achieve high success rate in the treatment of hip SA with 1.5-stage THA, it is important to adhere to a strict protocol. This is inclusive of but not limited to:
- Obtaining joint aspirate pre-operatively for microbial data
- Radical and meticulous debridement of all infected tissue (if performed)
- Copious amounts of irrigation
- Re-drape and re-gown
- Using a new set of surgical instruments for the reconstruction
- Use of appropriate organism-specific antibiotic for the cement spacer
SA is a rare but morbid condition that can have a significant impact on one’s function and quality of life rapidly. Management of SA is largely dependent on duration and activity level of the infection and extent of joint destruction. In a significantly deformed hip joint due to SA, 1.5-stage THA with CUMARS is a viable option with benefits of effective infection eradication, good functional outcomes, cost-effectiveness with reduced physical and psychological burden in avoiding a second operation, yet not precluding the possibility of a two-stage exchange THA if required.
1.5-stage THA in destructive hip SA using CUMARS brings about the benefit of good functional outcomes with reduced physical and psychological burden in avoiding a second surgery, especially in frail patients, yet not precluding the possibility of a two-stage exchange if required.
References
- 1.McElwaine J, Colville J. Excision arthroplasty for infected total hip replacements. J Bone Joint Surg Br 1984;66:168-71. [Google Scholar]
- 2.Nace J, Chen Z, Bains SS, Kahan ME, Gilson GA, Mont MA, et al. 1.5-Stage versus 2-stage exchange total hip arthroplasty for chronic periprosthetic joint infections: A Comparison of Survivorships, reinfections, and patient-reported outcomes. J Arthroplast 2023;38:S235-41. [Google Scholar]
- 3.Fleck EE, Spangehl MJ, Rapuri VR, Beauchamp CP. An articulating antibiotic spacer controls infection and improves pain and function in a degenerative septic hip. Clin Orthop Relat Res 2011;469:3055-64. [Google Scholar]
- 4.Younger AS, Duncan CP, Masri BA, McGraw RW. The outcome of two-stage arthroplasty using a custom-made interval spacer to treat the infected hip. J Arthroplasty 1997;12:615-23. [Google Scholar]
- 5.Tsung JD, Rohrsheim JA, Whitehouse SL, Wilson MJ, Howell JR. Management of periprosthetic joint infection after total hip arthroplasty using a custom made articulating spacer (CUMARS); the Exeter experience. J Arthroplasty 2014;29:1813-8. [Google Scholar]
- 6.Charlton WP, Hozack WJ, Teloken MA, Rao R, Bissett GA. Complications associated with reimplantation after girdlestone arthroplasty. Clin Orthop Relat Res 2003;407:119-26. [Google Scholar]
- 7.Russo A, Cavagnaro L, Chiarlone F, Clemente A, Romagnoli S, Burastero G. Clinical outcomes and survivorship of two-stage total hip or knee arthroplasty in septic arthritis: A retrospective analysis with a minimum five-year follow-up. Int Orthop 2021;45:1683-91. [Google Scholar]
- 8.Hipfl C, Karczewski D, Oronowicz J, Pumberger M, Perka C, Hardt S. Total hip arthroplasty for destructive septic arthritis of the hip using a two-stage protocol without spacer placement. Arch Orthop Trauma Surg 2023;143:19-28. [Google Scholar]
- 9.Masri BA, Duncan CP, Beauchamp CP. Long-term elution of antibiotics from bone-cement: An in vivo study using the prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) system. J Arthroplasty 1998;13:331-8. [Google Scholar]
- 10.Anagnostakos K, Jung J, Schmid NV, Schmitt E, Kelm J. Mechanical complications and reconstruction strategies at the site of hip spacer implantation. Int J Med Sci 2009;6:274. [Google Scholar]
- 11.Pignatti G, Nitta S, Rani N, Dallari D, Sabbioni G, Stagni C, et al. Two stage hip revision in periprosthetic infection: Results of 41 cases. Open Orthop J 2010;4:193-200. [Google Scholar]
- 12.Palmer CK, Gooberman-Hill R, Blom AW, Whitehouse MR, Moore AJ. Post-surgery and recovery experiences following one-and two-stage revision for prosthetic joint infection-a qualitative study of patients’ experiences. PLoS One 2020;15:e0237047. [Google Scholar]
- 13.Depuy Orthopaedics I. Prostalac Hip System. Johnson & Johnson; 2004. [Google Scholar]
- 14.Burastero G, Basso M, Carrega G, Cavagnaro L, Chiarlone F, Salomone C, et al. Acetabular spacers in 2-stage hip revision: Is it worth it? A single-centre retrospective study. Hip Int 2017;27:187-92. [Google Scholar]
- 15.Quayle J, Barakat A, Klasan A, Mittal A, Stott P. External validation study of hip peri-prosthetic joint infection with cemented custom-made articulating spacer (CUMARS). Hip Int 2022;32:379-85. [Google Scholar]