Intralesional doxycycline ablation can be an effective alternative for the treatment of aneurysmal bone cysts located in anatomically complex areas, in non-expendable bones, and instances of recurrence.
Dr. Katrina Ysabel R Naraval, Department of Orthopaedics, Institute of Orthopaedics and Sports Medicine, St. Luke’s Medical Center, Quezon, Philippines. E-mail: khayanaraval@gmail.com
Introduction: Aneurysmal bone cysts (ABCs) are benign, locally destructive, blood-filled reactive lesions of the bone most commonly presenting as pain or mass effect. Most are frequently located in the proximal humerus, distal femur, proximal tibia, spine, uncommonly the sacrum, and rarely the sacroiliac (SI) joint. We present a rare case of ABC in the SI joint and its recurrence treated with percutaneous intralesional doxycycline ablation and the corresponding outcome.
Case Report: A 29-year-old female presented with persistent gluteal pain and radiculopathy and was subsequently diagnosed with ABC in the left SI joint. She underwent intralesional extended curettage with the application of synthetic bone graft substitute over the defect. One year postoperatively, local recurrence of the mass was noted after presenting with similar symptoms of radiculopathy. She then underwent six sessions of CT-guided percutaneous intralesional doxycycline ablation at 2–3-month intervals. Serial monitoring through plain CT scan showed interval development of intralesional osseous formation and decreased lytic spaces. At the latest follow-up of 3½ years after treatment cessation, the patient remained asymptomatic with no recurrence.
Conclusion: This reports the only known local experience using non-invasive treatment for the recurrence of ABC in the SI joint through CT-guided intralesional ablation of doxycycline resulting in relief of symptoms and absence of recurrence at 3½ years post-treatment. This supports previous studies showing doxycycline administration as an effective alternative in the treatment of ABCs in recurrent cases, in challenging cases due to its location, or when located in non-expendable areas such as the SI joint and sacrum. More extensive studies with longer follow-ups are needed to validate these findings.
Keywords: Aneurysmal bone cyst, sacroiliac joint, doxycycline.
Aneurysmal bone cysts (ABC) are benign yet aggressive, expansile, blood-filled reactive bone lesions, characterized histologically by hemorrhagic tissue with cavernous spaces separated by cellular stroma and fibrous cysts walls [1]. ABCs comprise 1% of primary bone tumors, affecting the meta-epiphyseal regions of long bones in 50%, the spine in 30%, and the pelvis in 20% of cases [2, 3]. In a retrospective study involving 40 patients with ABCs of the pelvis and sacrum, nine were found to be intra-articular (22%), with only two found to occur at the sacroiliac (SI) joint (5%) [4]. Further, various studies report a wide range of recurrence rates from as low as 5% to as high as 71% [5-7]. The current treatment standard for these lesions is surgery. Options include curettage and application of bone graft or polymethylmethacrylate (PMMA), or resection of lesions [1]. In cases where surgery may be challenging due to the location of the cyst or if it could lead to destabilizing effects on the bone, minimally invasive forms of management are offered. These include radiotherapy, radionuclide ablation, bisphosphonate injection, and targeted molecular therapy using denosumab with varying ranges of recurrence and success rates [8]. In recent studies, percutaneous intralesional injection of doxycycline, an antibiotic with bacteriostatic properties, has demonstrated antitumoral properties and showed promising results in the treatment of ABCs [3, 5, 10, 11]. This paper describes a case of local recurrence following initial curettage and bone grafting of an ABC in the SI joint treated with the off-label use of percutaneous intralesional doxycycline and its outcome.
History and physical examination
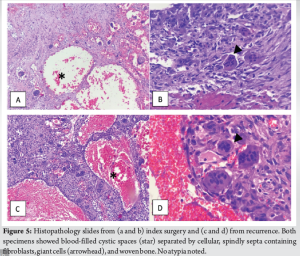
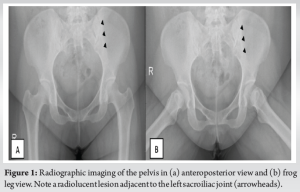
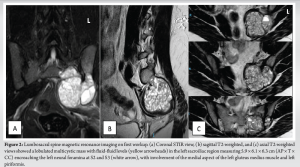
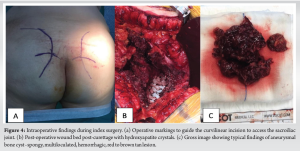
A 28-year-old female presented with a 3-week history of dull and persistent gluteal pain with associated radiculopathy to the left lower extremity and resultant antalgic gait. There was no palpable mass, but infragluteal tenderness was present. Neurologic testing showed weakness of the left extensor hallucis longus but with no sensory deficits and tension signs. Pelvic radiographs showed a subtle area of lucency adjacent to the left SI joint (Fig. 1). Plain magnetic resonance imaging (MRI) of the lumbosacral spine exhibited a multicystic lobulated mass measuring 5.9 × 6.1 × 6.3 cm (AP × T × CC) encroaching the left neural foramina at S2 and S3, with involvement of the left gluteus medius muscle and piriformis, suggesting an ABC (Fig. 2). Further, an angiography revealed the main blood supply branching off the superior gluteal and lateral sacral arteries (Fig. 3a). She then underwent CT-guided biopsy and embolization before definitive surgery (Fig. 3b). Extended curettage was performed seven days later (Fig. 4a), accompanied by cauterization and soaking of the cyst wall in 200 mL plain saline mixed with 1cc of epinephrine. Gel foam was applied in the subchondral area adjacent to the SI joint and the defect was packed with 10cc of synthetic bone graft using hydroxyapatite crystals (Bongros, Daewoong Pharmaceutical Company Indonesia) (Fig. 4b). Gross specimen was typical of ABC (Fig. 4c). Final histopathology confirmed the diagnosis (Fig. 5a and b).

Postoperatively, she was maintained on non-weight bearing for 6 weeks. She was able to tolerate independent ambulation at 12 weeks. However, 1 year after surgery, she sought consult due to a recurrence of low back and gluteal pain radiating to the left leg. No weakness, numbness, or bowel and bladder symptoms were documented.
Diagnostic tests
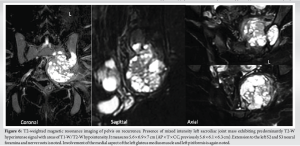
MRI on follow-up showed a left SI joint mass measuring 5.6 × 6.9 × 7 cm (AP × T × CC) exhibiting a predominantly T2-weighted hyperintense signal with fluid-fluid levels (Fig. 6). Extension to the left S2 and S3 neural foramina and nerve roots was again noted. Involvement of the left gluteus medius muscle and left piriformis muscle was unchanged.
On plain computed tomography (CT) scan, a lytic, expansile bone lesion centered in the left SI joint, measuring 6.2 × 7.3 × 6.5 cm (AP × T × CC) with extension into the ipsilateral sacrum and iliac bones and associated osseous expansion and sclerotic borders was noted (Fig. 7a). CT-guided biopsy was done to confirm the diagnosis of local recurrence of ABC. Histopathology showed characteristic hemorrhagic tissue with cavernous spaces separated by cellular stroma, while the cells that line the cyst wall showed fibrous components, macrophages, giant cells, and islands of bone (Fig. 5c and d). Subsequently, angiography and embolization were done, revealing devascularization and non-visualization of the previous tumor staining seen previously.
After recurrence was established, treatment options were discussed. Surgery with wide resection and spinopelvic fusion versus percutaneous intralesional doxycycline ablation was offered. She opted to undergo the less invasive approach; hence, she was referred to interventional radiology for co-management.
Procedure performed and post-operative course
Technique
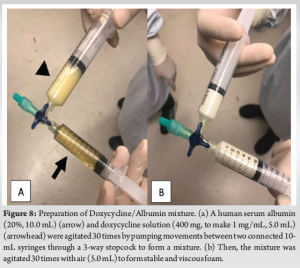
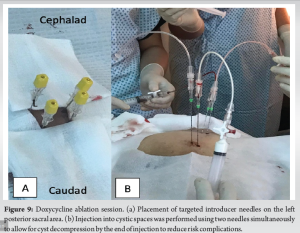
The ablative agent was prepared minutes before injection. Human serum albumin 20% (10.0 mL) and doxycycline (four 100 mg capsules combined with PNSS solution to make 5.0 mL) were admixed by pumping the solution between two interconnected syringes. Thereafter, 5.0 mL of the solution was withdrawn and agitated 30 times with 5.0 mL of air between two new interconnected syringes. Doxycycline 1mg/mL was added until a stable, viscous foam was created (Fig. 8b).
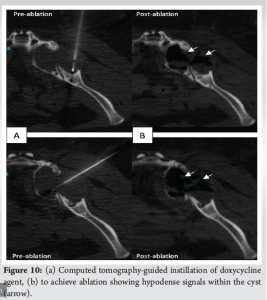
The patient was placed in a prone position under total intravenous anesthesia. Preliminary scanning through CT scan was done to localize the SI mass. Puncture sites were identified (Fig. 9). Gauge 18 × 20 cm introducer needles were placed through the skin toward several sites of the target lesion pre-determined by CT scan (Fig. 10a). One needle was used for injection and another for outflow simultaneously (Fig. 10b). A post-procedural CT scan showed ablation of the mass (Fig. 10b).
A total of six sessions of treatment were performed. The first two sessions were done at an 8-week interval and then every 12 weeks thereafter.
Post-operative course
She reported severe low back pain with a visual analog scale (VAS) of 8/10 during the first two sessions and was treated initially with patient-controlled analgesia Fentanyl. This was then shifted to pregabalin (ranging from 150 mg to 300 mg/dose), paracetamol (650 mg/tab), and Fentanyl patch (dose ranging from 50 to 150 mg). After the last session, pain was controlled with a VAS of 3/10. CT scan was repeated every 6 months after the last session (Fig. 7). At 1 year after initiation of doxycycline treatment, there was osseous formation within the lesion, development of sclerosis, and significant decreased cystic volume to 4.3 × 5.7 × 5.9 cm. The interval appearance of a well-delineated neural foramina hosting the corresponding nerve roots was also appreciated (Fig. 7b). Clinically, the patient reported improved symptoms with a decreased intake of pain medications. Significant bone formation with a further decrease in cystic volume to 4.6 × 4.9 × 5.5 cm was noted 2 years post-treatment initiation (Fig. 7c). At 1 year post-treatment cessation, the patient reported no pain, radiculopathy, or neurologic deficits. CT scan showed no tumor recurrence (Fig. 7d). At the latest follow-up at 1½ years post-treatment cessation, the patient remained asymptomatic with no tumor recurrence (Fig. 7e).
ABCs encompass only 1% of all primary bone tumors and are more commonly located in meta-epiphyseal areas of long bones or the spine [2]. ABCs are rarely seen in the pelvis, with an occurrence of only 7% [12]. A study by Bayraktutan et al. analyzed 16 cases of pelvic bone cysts and showed that most of these cysts occur in the ilium, followed by the pubic ramus and ischium. The least number of lesions occurred adjacent to the SI joint, none involving the joint itself [13]. In a literature review, only one case report documents the occurrence of an ABC on the SI joint [13]. Treatment of ABCs is mainly surgical. The standard of care remains to be curettage with or without insertion of bone graft or PMMA, especially in contained primary lesions [1, 2]. However, resection may be performed in cases where an ABC is extensive or recurrent and located in expendable bone. To date, there is still no clear consensus for the management of ABCs, and recurrence rates vary depending on the procedure done. In patients who undergo curettage, recurrence rates may range from as low as 12% to as high as 71%, usually attributed to incomplete curettage of the lesion [5, 6, 14]. In a review of 272 patients, the recurrence after curettage was noted within 6 months after the index surgery [7]. On the other hand, those who undergo resection had lower recurrence; however, they require more extensive reconstruction and may result in increased morbidity and compromised functional outcomes [6, 15]. In our case, since the patient’s mass was in a non-expendable bone, traditional curettage with the application of synthetic bone graft was utilized during the index surgery, with documentation of recurrence 1 year later. Patients with lesions affecting the sacrum often present late due to severe pain and neurologic symptoms and rather challenging cases due to its location and limited surgical options. Due to the highly vascular nature of ABCs and the relative difficulty in access to the lesion, selective arterial embolization (SAE) can be done preoperatively to decrease intraoperative bleeding. A decrease in local recurrence (0–12%) has been observed in earlier reports after SAE [16, 17]. However, a recent literature review showed no significant reduction in local recurrence after SAE [7]. The role of radiotherapy has also been reported as an effective, less invasive treatment option, but due to the possibility of secondary malignancies, it is often reserved for selected cases [18]. In areas where adequate curettage may be impossible and may lead to destabilizing effects such as in the spine or SI joint, or may impair growth being close to the physis, various options for non-invasive treatment, including radionuclide ablation, bisphosphonate injection, and targeted molecular therapy using denosumab, have been reported [8, 11]. A retrospective study involving 20 patients diagnosed with ABC reported outcomes of denosumab administration with an average follow-up of 18–24 months [5]. Indications for the procedure include recurrence after surgical curettage and bone grafting and patient or surgeon request for an alternative treatment. A significant decrease in lytic lesions was noted during the third session, with increased cortical thickening and a 5% overall recurrence rate [5]. Previously, injection of polidocanol and an alcoholic solution has shown a 58–94% response rate but has been discontinued mainly for significant complications, including pulmonary embolism, skin necrosis, pain, swelling, and fever [9]. Our case presented with a local recurrence in the SI joint after surgical curettage and bone grafting. A less invasive treatment was opted for the patient; hence, she was indicated for the off-label use of doxycycline through percutaneous intralesional ablation. Treatment of ABC with intraosseous doxycycline injection was first introduced in 2012, with the aim of restoring normal anatomy and function while reducing local recurrence and minimizing morbidities [3, 5, 7, 11]. Primarily used as an antibiotic, doxycycline has also been shown to have antitumoral properties by inhibiting matrix metalloproteinases and angiogenesis in some bone and soft-tissue malignancies, inducing osteoclastic apoptosis and causing a reaction leading to fibrin and collagen deposition [19, 20]. Its use as an osteotactic agent with albumin as the drug vehicle has also been reported [5, 11, 20]. Hence, for our patient, human serum albumin 20% was used together with doxycycline. Previous studies have shown that doxycycline administration is an effective alternative in the treatment of ABCs in non-expendable areas [5, 7, 11]. The outcome of our patient supports this finding. Six months after her last treatment session, significant intralesional ossification and decreased lytic areas were noted. At 3½ years after treatment, the patient remained asymptomatic with no tumor recurrence. Literature describes ABC as healed if no recurrence is seen within 2 years after completing treatment [5, 11]; hence, we can consider the patient healed after her doxycycline ablation treatment.
This reports the only known local experience using non-invasive treatment for the recurrence of ABC in the SI joint through CT-guided intralesional ablation of doxycycline along with an adjunct of pre-operative SAE. This case supplements previous studies showing doxycycline administration as an effective alternative in the treatment of ABCs in non-expendable areas such as the SI joint and sacrum, with no signs of recurrence 3½ years post-treatment. More extensive studies are needed to validate these findings as significant.
This case demonstrates the challenges in the treatment of ABCs despite their benign nature. Inadequate curettage or surgical access challenges can lead to a high recurrence risk. The use of intralesional doxycycline ablation can be considered as a treatment alternative in such cases, especially when opting for less invasive approaches. Our case illustrates the effectiveness of this treatment modality, which can lead to successful healing and sustained absence of recurrence.
References
- 1.Mankin HJ, Hornicek FJ, Ortiz-Cruz E, Villafuerte J, Gebhardt MC. Aneurysmal bone cyst: A review of 150 patients. J Clin Oncol 2005;23:6756-62. [Google Scholar]
- 2.Alhabshi SM, Haflah NH, Suraya A, Tan SP. Pelvic aneurismal bone cyst. Biomed Imaging Interv J 2011;7:e24. [Google Scholar]
- 3.Puri A, Hegde P, Gulia A, Parikh M. Primary aneurysmal bone cysts. Bone Joint J 2020;102-B:186-90. [Google Scholar]
- 4.Papagelopoulos PJ, Choudhury SN, Frassica FJ, Bond JR, Unni KK, Sim FH. Treatment of aneurysmal bone cysts of the pelvis and sacrum. J Bone Joint Surg Am 2001;83:1674-81. [Google Scholar]
- 5.Shiels WE 2nd, Mayerson JL. Percutaneous doxycycline treatment of aneurysmal bone cysts with low recurrence rate: A preliminary report tumor. Clin Orthop Relat Res 2013;471:2675-83. [Google Scholar]
- 6.Peeters SP, Van Der Geest IC, De Rooy JW, Veth RP, Schreuder HW. Aneurysmal bone cyst: The role of cryosurgery as local adjuvant treatment. J Surg Oncol 2009;100:719-24. [Google Scholar]
- 7.Parker J, Soltani S, Boissiere L, Obeid I, Gille O, Kieser DC. Spinal aneurysmal bone cysts (ABCs): Optimal management. Orthop Res Rev 2019;11:159-66. [Google Scholar]
- 8.Bush CH, Drane WE. Treatment of an aneurysmal bone cyst of the spine by radionuclide ablation. Am J Neuroradiol 2000;21:592-4. [Google Scholar]
- 9.Adamsbaum C, Mascard E, Guinebretière JM, Kalifa G, Dubousset J. Intralesional Ethibloc injections in primary aneurysmal bone cysts: An efficient and safe treatment. Skeletal Radiol 2003;32:559-66. [Google Scholar]
- 10.Burrows PE, Mitri RK, Alomari A, Padua HM, Lord DJ, Sylvia MB, et al. Percutaneous sclerotherapy of lymphatic malformations with doxycycline. Lymphat Res Biol 2008;6:209-16. [Google Scholar]
- 11.Ii WE 2nd, Beebe AC, Mayerson JL. Percutaneous doxycycline treatment of juxtaphyseal aneurysmal bone cysts. J Pediatr Orthop 2016;36:205-12. [Google Scholar]
- 12.Bloem JL, Reidsma II. Bone and soft tissue tumors of hip and pelvis. Eur J Radiol 2012;81:3793-801. [Google Scholar]
- 13.Bayraktutan U, Sade R, Kantarci M, Karaca L. Sacral and iliac aneurysmal bone cyst involving the sacroiliac joint. Spine J 2015;15:e45-6. [Google Scholar]
- 14.Çelik S, Uludağ A, Tosun HB, Serbest S, Gürger M, Kılıç S. Unicameral (simple) and aneurysmal bone cysts: The effect of insufficient curettage on recurrence. Pan Afr Med J 2016;24:311. [Google Scholar]
- 15.Huang JF, Shen J, Li X, Rengan R, Silvestris N, Wang M, et al. Incidence of patients with bone metastases at diagnosis of solid tumors in adults: A large population-based study. Ann Transl Med 2020;8:482-2. [Google Scholar]
- 16.Kim CG, Kweon SH. Primary aneurysmal bone cyst in the iliac bone: A case report. Hip Pelvis 2014;26:202. [Google Scholar]
- 17.Rossi G, Rimondi E, Bartalena T, Gerardi A, Alberghini M, Staals EL, et al. Selective arterial embolization of 36 aneurysmal bone cysts of the skeleton with N-2-butyl cyanoacrylate. Skeletal Radiol 2010;39:161-7. [Google Scholar]
- 18.Ghermandi R, Terzi S, Gasbarrini A, Boriani S. Denosumab: Non-surgical treatment option for selective arterial embolization resistant aneurysmal bone cyst of the spine and sacrum. Case report. Eur Rev Med Pharmacol Sci 2016;20:3692-5. [Google Scholar]
- 19.Duivenvoorden WC, Vukmirović-Popović S, Kalina M, Seidlitz E, Singh G. Effect of zoledronic acid on the doxycycline-induced decrease in tumour burden in a bone metastasis model of human breast cancer. Br J Cancer 2007;96:1526-31. [Google Scholar]
- 20.Liu X, Han SB, Si G, Yang SM, Wang CM, Jiang L, et al. Percutaneous albumin/doxycycline injection versus open surgery for aneurysmal bone cysts in the mobile spine. Eur Spine J 2019;28:1529-36. [Google Scholar]