Longitudinal atlanto-occipital dissociation (L-AOD) is a rare diagnosis with a high rate of neurological deficits and mortality. The advancements in emergency care, diagnostic methods, and treatment options have increased survival rates and overall prognosis of the atlanto-occipital dissociation. A VISOR (head-neck-chest) orthosis and careful observation could be one of the treatment options for longitudinal atlanto-occipital dissociation (L-AOD).
Dr. Rajendra Sakhrekar, Department of Spine Surgery, Children Hospital Westmead, Sydney, Australia. E-mail: raj.sakhrekar1@gmail.com
Introduction: Death is the most common outcome of longitudinal atlanto-occipital dissociation (L-AOD). Even though rare, survival is commonly seen in the pediatric population. This study reports a successful outcome of a pediatric patient with an L-AOD without neurodeficits, immobilized in a visor (head-neck-chest) orthosis.
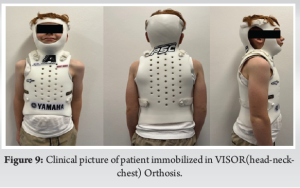
Case Report: A 9-year-old boy came off his motorbike during a jump at ~50 kph. He was transferred from the primary hospital with spine precautions and a cervical collar with multiple injuries with neurologically intact on presentation. The computed tomography (CT) spine demonstrated a widening of the basion–dens interval, estimated approximately at 16 mm (normal <10 mm), with the widening of the atlanto-occipital articulations with occipital condyles and atlas facet distance markedly widened approximately at 7 mm (normal <5 mm). Considering intact neurology and no complete tear of the tectorial membrane, the decision was made to immobilize in a visor (head-neck-chest) orthosis for controlled vertical cranial settling to occur. Periodic cervical spine imaging over 3 months was done to assess the reduction. At the end of 3 months, dynamic cervical spine X-rays and CT scans confirmed atlanto-occipital articulations with the basion–dens interval and intercondylar distance within normal limits.
Conclusion: L-AOD is a rare diagnosis with a high rate of neurological deficits and mortality. The advancements in emergency care, diagnostic methods, and treatment options have increased survival rates and overall prognosis of the atlanto-occipital dissociation. A visor (head-neck-chest) orthosis and careful observation could be one of the treatment options for L-AOD.
Keywords: Longitudinal atlanto-occipital dissociation, visor (head-neck-chest) orthosis, pediatric cervical spine injury.
Death is the most common outcome of longitudinal atlanto-occipital dissociation (L-AOD). Even though rare, survival is commonly seen in the pediatric population [1-3]. Considering its rare representation and associated life-threatening injuries like head injury and carotid and vertebral artery injuries, missed diagnosis of atlanto-occipital dissociation (AOD) is not uncommon, and delayed diagnosis as long as 2 years post-injury is documented in the literature [4-6]. This study reports a successful outcome of a pediatric patient with an L-AOD without neurodeficits, immobilized in a visor (head-neck-chest) orthosis.
A 9-year-old boy came off his motorbike during aHe was transferred from the primary hospital with spine precautions and cervical collar with multiple injuries: subarachnoid hemorrhage, right internal carotid artery dissection, suspected cervical spine injury, left wrist fracture, bilateral pulmonary contusions, left knee lacerations, and lower lip laceration to our tertiary care hospital. He was neurologically intact on presentation. The CT spine demonstrated widening of the basion–dens interval, estimated approximately at 16 mm (normal <10 mm), with the widening of the atlanto-occipital articulations with occipital condyles and atlas facet distance markedly widened approximately at 7 mm (normal <5 mm), (Fig 1,2) while the magnetic resonance imaging (MRI) spine imaging demonstrated stripping of the anterior and the left posterior atlanto-occipital membrane and stripping of the proximal tectorial membrane, the complete tear of the apical ligament with fracture avulsion of the right alar ligament. The spinal cord edema from C3-C6 demonstrated traumatic central cord syndrome.(Fig. 3).

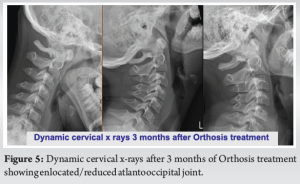
Considering intact neurology and no complete tear of the tectorial membrane, the decision was made to immobilize in a visor (head-neck-chest) orthosis for controlled vertical cranial settling to occur. Periodic cervical spine imaging over 3 months was done to assess the reduction. (Fig. 4) At the end of 3 months, dynamic cervical spine X-rays and CT scans confirmed atlanto-occipital articulations with the basion–dens interval and intercondylar distance within normal limits.(Fig. 5).

Essential anatomy to know
Ligament anatomy
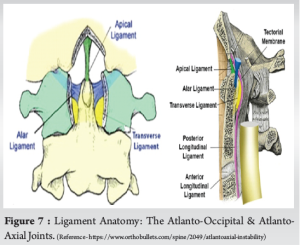
The primary ligament stabilizers of the atlanto-occipital junction are the tectorial membrane, paired alar ligaments, apical ligament of the dens, and posterior atlanto-occipital membrane (Fig. 6, 7). The tectorial membrane connects the posterior body of the axis to the anterior foramen magnum and is the cephalad continuation of the posterior longitudinal ligament, which prevents excessive extension. The paired alar ligaments are relatively strong structures and connect the odontoid to the occipital condyles and prevent excessive rotation. The transverse ligament connects the posterior odontoid to the anterior atlas arch, inserting laterally on bony tubercles. The apical ligament’s relatively weak midline structure runs vertically between the odontoid and foramen magnum and is prone to ruptures during O-C1 injuries.

Bony anatomy
The occipital-atlantoaxial complex – The occiput, atlas, and axis relationship form the occipital-atlantoaxial joint. (Fig. 6). The six main synovial joint articulations are as follows:
- Anterior and posterior median atlanta-odontoid joints
- Paired atlanto-occipital joints
- Paired atlantoaxial joints.
Clinical presentation
Associated injuries make the diagnosis of AOD challenging. Closed head injury and low Glasgow Coma Scale make it difficult to assess the neurologic deficits at presentation. Vascular injuries and intracranial or brainstem damage are life-threatening. Incomplete neurological deficits are more common than incomplete due to O-C1 spinal cord injuries. Respiratory deficits due to direct brainstem damage, diaphragmatic paralysis, or pulmonary contusions are seen too. Sixth (abducens) nerve palsy causing strabismus (eye misalignment) is more common than other cranial nerve injuries. The overall prognosis of children with AOD depends on associated injuries and the severity of the neurologic findings due to AOD [7,8]. Some patients return to normal if neurological improvement is noted in the initial recovery period. However, most are left with a deficit, either complete or partial.
Mechanism of injury
The pediatric spine is considered from birth to 9 years and represents unique features compared to the adult spine. The ligaments and joint capsules in the pediatric spine are elastic; facet joints are shallow and more horizontal; intervertebral discs are more expansile; and vertebral bodies are anteriorly wedged due to lack of complete ossification. Due to its elastic nature, hypermobility and flexibility to external forces allow significant movement between spinal segments without damage. Unfortunately, with a proportionately heavy head as compared to the cervical spine and susceptible cervical anatomy, the fulcrum of movements in younger children lies in the upper cervical spine, making it more susceptible to the spinal column and spinal cord injuries. Leventhal reported that the spinal column could lengthen by two without damage, while the spinal cord could be only 0.25 [9]. High-energy trauma causing hyperextension with disruption of the tectorial membrane and lateral or hyperflexion with disruption of the alar ligaments and posterior atlanto-occipital ligament are thought to co-occur. Multiple ligament ruptures are more likely to give atlanto-occipital instability than a single ligament rupture [2, 3, 6].
Imaging
The Spinal Cord Society recently proposed the radiological protocol, stating that a multidetector CT scan with reformatted images is the initial imaging option for trauma patients. Radiographs should be used only if CT is unavailable or unaffordable. MRI should be indicated in patients with neurological involvement to evaluate spinal cord compromise, epidural-space compromise, disco-ligamentous injury, and soft tissue injuries. CT angiograms should be advised in suspected vertebral and carotid artery injuries [10-12].

Classification
Traynelis classification [8].
It is based on the direction of displacement of the skull.
Type I – Anterior occiput dissociation
Type II – Longitudinal dissociation
Type III – Posterior occiput dissociation
The longitudinal dissociation/distraction type is considered difficult to diagnose and is the most fatal. Types 1 and 2 constitute 40% of all types, 5% are type 3, and 15% are mixed types.
Power ratio
It is the ratio between the distance from the basion and the posterior spinolaminar line of the atlas/the distance from the opisthion and the anterior arch of the atlas.
ratio ~1 is normal,
>1.0 raises concern for anterior dissociation,
<1.0 raises concern for posterior AOD, odontoid fractures, a ring of atlas fractures Harris’s rule of 12 [11,13].
Basion–dens interval or basion-posterior axial interval, >12 mm, suggests longitudinal occipitocervical dissociation.
Our study demonstrated a basion–dens interval of >16 mm. (Fig. 8).
L-AOD is a rare diagnosis with a high rate of neurological deficits and mortality. Advancements in emergency care, diagnostic methods, and treatment options have increased survival rates and the overall prognosis of AOD [3, 4]. Literature on AOD is rare, and pediatric L-AOD is much rarer [14]. Astur et al. [15] demonstrated eight pediatric patients (mean age: 5.2 years) with a type II (longitudinal) AOD, all treated with posterior occipitocervical fusion with internal fixation. Van de Pol et al. [16] demonstrated a case of L-AOD with dissociation in halo immobilization in a 4-year-old boy awaiting posterior C0-C1 fusion due to poor general condition. They carefully reduced the AOD under image intensification and performed an occiput C1-C2 fusion using internal fixation and allograft bone. Halo vests can help prevent further neurological damage in posttraumatic cervical spine instability in some cases [16-18]. Our institutional experience in using halo immobilization in vertically unstable O-C dissociation is that it could cause further distraction due to the rigid fixation of the halo/skull to the vest. The vest tends to migrate proximally when lying flat, displacing the halo ring and skull. We believe that the full visor orthosis, which is not rigidly attached to the skull, allows vertical cranial settling without distracting the head when lying down. Furthermore, tolerance of halo frame immobilization is concerning for some patients. Complications of halo vest are relatively high and include pin loosening, pin site infection migration, penetration, scalp infection, skull fracture, cerebral hemorrhage, paresthesia, and pressure sores [16-18]. In the present study, CT diagnosed LAOD, and an MRI demonstrated no spinal cord compromise. The complete tear of the apical ligament with fracture avulsion of the right alar ligament but only stripping of the anterior and the left posterior atlanto-occipital membrane and the proximal tectorial membrane without rupture was noted. Cervical lateral X-ray after applying visor orthosis (head-neck-chest) demonstrated a reduced LAOD. Considering no neurological deficit and well-reduced atlanto-occiput joint, careful observation and periodic X-rays to look for instability were decided. Over 3 months, periodic clinical examinations and X-rays in visor orthosis were done to assess the patient clinically and radiologically. At the end of 3 months, a follow-up CT scan and dynamic cervical spine flexion/extension and neutral X-rays were done, confirming enlocated/reduced normal atlanto-occiput joint. This case demonstrates a visor (head-neck-chest ) orthosis, and careful observation could be one treatment option for L-AOD. (Fig. 9).
L-AOD is a rare diagnosis with a high rate of neurological deficits and mortality. The advancements in emergency care, diagnostic methods, and treatment options have increased survival rates and overall prognosis AOD. A visor (head-neck-chest) orthosis and careful observation could be one of the treatment options for L-AOD.
L-AOD is a rare diagnosis with a high rate of neurological deficits and mortality. The advancements in emergency care, diagnostic methods, and treatment options have increased survival rates and overall prognosis of AOD. A visor (head-neck-chest) orthosis and careful observation could be one of the treatment options for L-AOD.
References
- 1.Donahue DJ, Muhlbauer MS, Kaufman RA, Warner WC, Sanford RA. Childhood survival of atlantooccipital dislocation: Underdiagnosis, recognition, treatment, and review of the literature. Pediatr Neurosurg 1994;21:105-11. [Google Scholar]
- 2.Papadopoulos SM, Dickman CA, Sonntag VK, Rekate HL, Spetzler RF. Traumatic atlantooccipital dislocation with survival. Neurosurgery 1991;28:574-9. [Google Scholar]
- 3.Ferrera PC, Bartfield JM. Traumatic atlanto-occipital dislocation: A potentially survivable injury. Am J Emerg Med 1996;14:291-6. [Google Scholar]
- 4.Labler L, Eid K, Platz A, Trentz O, Kossmann T. Atlanto-occipital dislocation: Four case reports of survival in adults and review of the literature. Eur Spine J 2004;13:172-80. [Google Scholar]
- 5.Jevtich V. Traumatic lateral atlanto-occipital dislocation with spontaneous bony fusion. Spine (Phila Pa 1976) 1989;14:123-4. [Google Scholar]
- 6.Kaufman RA, Dunbar JS, Botsford JA, McLaurin RL. Traumatic longitudinal atlanto-occipital distraction injuries in children. AJNR Am J Neuroradiol 1982;3:415-9. [Google Scholar]
- 7.Hazboun R, Muñoz A, Krafft PR, Harder S, Vannix R, Zouros A, et al. Craniocervical dissociation in pediatric patients: Pearls and pitfalls of diagnosis and management. Pediatr Emerg Care 2021;37:e602-8. [Google Scholar]
- 8.Traynelis VC, Marano GD, Dunker RO, Kaufman HH. Traumatic atlanto-occipital dislocation. Case report. J Neurosurg 1986;65:863-70. [Google Scholar]
- 9.Leventhal HR. Birth injuries of the spinal cord. J Pediatr 1960;56:447-53. [Google Scholar]
- 10.Wholey MH, Bruwer AJ, Baker HL Jr. The lateral roentgenogram of the neck. Radiology 1958;71:350-6. [Google Scholar]
- 11.Harris JH Jr., Carson GC, Wagner LK. Radiologic diagnosis of traumatic occipitovertebral dissociation: 1. Normal occipitovertebral relationships on lateral radiographs of supine subjects. Am J Roentgenol 1994;162:881-6. [Google Scholar]
- 12.Yelamarthy PK, Chhabra HS, Vaksha V, Agarwal Y, Agarwal A, Das K, et al. Radiological protocol in spinal trauma: Literature review and spinal cord society position statement. Eur Spine J 2020;29:1197-211. [Google Scholar]
- 13.Radcliff K, Kepler C, Reitman C, Harrop J, Vaccaro A. CT and MRI-based diagnosis of craniocervical dislocations: The role of the occipitoatlantal ligament. Clin Orthop Relat Res 2012;470:1602-13. [Google Scholar]
- 14.Joaquim AF, Schroeder GD, Vaccaro AR. Traumatic atlanto-occipital dislocation-a comprehensive analysis of all case series found in the spinal trauma literature. Int J Spine Surg 2021;15:724-39. [Google Scholar]
- 15.Astur N, Klimo P Jr., Sawyer JR, Kelly DM, Muhlbauer MS, Warner WC Jr. Traumatic atlanto-occipital dislocation in children: Evaluation, treatment, and outcomes. J Bone Joint Surg 2013;95:e194. [Google Scholar]
- 16.Van de Pol GJ, Hanlo PW, Oner FC, Castelein RM. Redislocation in a Halo vest of an atlanto-occipital dislocation in a child: Recommendations for treatment. Spine (Phila Pa 1976) 2005;30:E424-8. [Google Scholar]
- 17.Steinmetz MP, Verrees M, Anderson JS, Lechner RM. Dual-strap augmentation of a halo orthosis in the treatment of atlantooccipital dislocation in infants and young children. Technical note. J Neurosurg Spine 2002;96:346-9. [Google Scholar]
- 18.Babashahi A, Rezvani M, Vatankhah M, Kalani N, Kazeminezhad A. Complications of halo vest orthosis: A narrative study. Iran J Neurosurg 2021;7:131-8. [Google Scholar]