Despite severe deformities associated with PPRD, fixation of fracture around proximal tibia restores bone stock and alignment for future joint replacement.
Dr. C Sitsabesan, Department of Orthopedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. E-mail: sitsabesan@sriramachandra.edu.in
Introduction: Progressive pseudorheumatoid dysplasia is an autosomal recessively inherited rare disorder with features of growth retardation, multiple joint deformities, and intra-articular loose bodies.
Case Report: This case study is about a 34-year-old man who presented to us following trauma to his right leg. On general assessment, he was short statured with multiple deformities of both upper and lower limbs with local signs suggestive of proximal tibial fracture over his right tibia. Blood values indicated low Vitamin D levels with normal serum calcium and alkaline phosphatase, inclusive of the inflammatory markers. X-rays showed platyspondyly, decreased bone stock, and significant joint space narrowing in addition to the displaced proximal tibial meta-diaphyseal fracture. He was managed surgically and went on to have an uneventful post-operative period with fracture healing but with a need for further intervention in the future to address his associated secondary knee arthritis.
Conclusion: To share the morphometrics and presentation of this rare disease. And to highlight the role of psychological and rehabilitative therapy in improving the disease outcomes.
Keywords: Pseudorheumatoid, synovial chondromatosis, growth retardation, multiple joint deformities, intra-articular loose bodies.
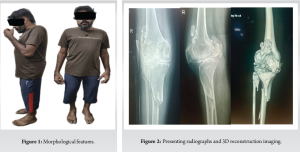
Progressive pseudo-rheumatoid dysplasia (PPRD) is a rare, non-inflammatory autosomal recessive inherited musculoskeletal disorder [1]. Its incidence is around 1/1000,000. Primary chondral dysplasia affects the articular cartilage of multiple joints of both the axial and appendicular skeleton. The onset of the disease is between 3 and 8 years of age and hence presents as growth retardation with short stature (Fig. 1). The common skeletal manifestations are, platyspondyly, kyphoscoliosis, bilateral coxa vara of hips, genu varum of the knee and planovalgus of the foot. Abnormal intra-articular calcium deposition (synovial osteochondromatosis) around the joints is a unique finding that helps to differentiate from the other forms of juvenile rheumatoid disease and seronegative polyarticular diseases. We report one such case who presented with a proximal tibial fracture secondary to a trivial trauma. Our aim is to share this rare disease to discuss its morphometrics of multiple dysplastic joints associated with multiple osteochondromatosis. Furthermore, the case study is to highlight the osteopenia and associated fracture possibilities in PPRD with the subsequent normal healing process and its challenges.
A 34-year-old gentleman presented to our out patient’s clinic with history of trivial trauma and a painful deformed right leg (Fig. 2) with associated multiple joint stiffness and deformities. On examination, patient was short stature. (Fig. 1) In the upper limbs, he had bilateral fixed flexion deformity of the elbows with gross restricted shoulder, elbow, and wrist movements. He was short-trunked without spinal deformity, but both hips with features of coxa vara and fixed flexion deformity of both knees. In addition, he had clinical signs of fracture proximal tibia on his right leg. His blood values showed low Vitamin D3 levels (5 ng/mL, reference range 25–80 ng/dL), normal levels of serum calcium (9.2 mg/dL, reference range 8.5–10.5 mg/dL) and serum phosphate (2.7 mg/dL, reference range 2.5–4.5 mg/dL) His erythrocyte sedimentation rate, C-reactive protein, and serum parathyroid hormone were within normal limits with negative RA factor.
Skeletal screening of the patient showed decreased bone stock, cortical thinning, and multiple loose bodies (osteochondromatosis knee) with significant joint space narrowing of the knee joints. The condyles showed dysplastic features suggestive of early-onset childhood disease. In the axial skeleton, spine showed elongated vertebras. (Platyspondyly) both in cervical and dorso- lumbar region. X-ray pelvis (Fig. 3) showed bilateral coxa vara with significant joint space narrowing and dysplastic proximal femur. Additional screening X-rays of both elbows showed dysplastic radial heads and distal humerus with significant joint loss and multiple osteochondromatosis.
Procedure
His ability to cope with his disabilities from multiple joint pathology has been taken into consideration for his age and fixation was planned. The aim was to restore alignment, reduce and to stabilize the fracture that it could allow mobilization, and also planned to consider future joint replacement. After taking an informed consent, his fractured proximal tibia was internally fixed despite his stiff knee joint associated with osteochondromatosis. The operative procedure involved fixation using a minimally invasive plate osteosynthesis technique with a locking compression plate. His fracture healed and he was restored to pre-injury mobility after 4 months (Fig. 4 and 5).

PPRD was first described by Wynne-Davies et al. [2] It is an autosomal recessive disorder with gene mutations of Wnt1-inducible signaling pathway protein 3 (WISP3). Shahi and Sehgal [1] reported a case of PPRD with biallelic pathogenic mutations in CCN6 which supported the diagnosis of PPRD where the patient received genetic counseling and psychological counseling which plays a key role to increase the ability to cope with the disease and in its prevention. El Dessouki et al. [3] studied PPRD and found to have a loss of function pathogenic mutations in the WISP3 (CCN6) gene, on chromosome 6q22 from 23 unrelated Egyptian patients and found 11 distinct sequence variants in the WISP3 (CCN6) gene emphasizing the role of genetic study in cases of PPRD. Giray et al. [4] showed severity being more in male siblings in the expressivity of PPRD and highlighted the benefits of early rehabilitation, and patient education in improving the functional outcome. Different types of homogenous or heterogenous mutational variants have been analyzed to be the cause of phenotypic variations in this disorder [5]. The impaired bone homeostasis is due to dysfunctional mesenchymal stem cell with increased expression of Type 1 collagen in osteoblast of PPRD [2, 6]. Characteristic radiological findings of PPRD include dysplastic epiphyseal widening, platyspondyly with coxa vara, and feature of osteoarthritis of joints. In addition, feature of synovial chondromatosis of large joints with essence of multiple loose chondroid bodies was pathognomonic of this disorder. Radiological findings are accurate but possible differential diagnosis includes seronegative spondyloarthritis, Mucopolysaccharidosis, Scheuermann kyphosis for the spine involvement, and other forms of juvenile arthritis. PPRD can be confirmed using molecular genetic testing and for exclusion needs other enzyme studies. Stickler’s syndrome is yet another differential diagnosis with multiple joint involvement [7]. Treatment of PPRD is palliative and focused on physical therapy in the early stages. Associated disuse osteopenia of long bones can predispose for extra-articular fractures from trivial trauma. Unfortunately, bisphosphonates will not be of use to counter the osteoporosis [8]. Intraoperative reduction and fracture fixation can be challenging task but bone healing remains normal. Physical therapy and rehabilitation are encouraged to preserve joint mobility and lifestyle modifications should be advised. Genetic diagnosis and counseling can be done to explain chance of offspring having the same disease. Further surgical techniques such as early arthroplasty and osteotomies can be attempted. Realignment of the fracture tibial shaft and relatively a stable fixation prepares for an early joint replacement. Prognosis will depend of the age of onset, severity, and progression of the disease and subsequent rehabilitation. Multiple joint replacements may be warranted for the severe form of PPRD at a younger age to improve the quality of life [9]. Although spine surgery is not commonly performed when spinal canal stenosis compromises the cord function it may warrant decompression and stabilization [10].
Presenting a rare case involving multiple limb deformities and degenerative complications, this case emphasizes the importance of thorough evaluation for early diagnosis. It also underscores the necessity of a multidisciplinary approach to management in order to achieve favorable long-term outcomes.
This rare disease might present with various joint deformities and should be differentiated from other arthropathies and metabolic disorders. Genetic and psychological counseling along with physical therapy and rehabilitation can improve quality of life.
References
- 1.Shahi P, Sehgal A. Delayed-onset progressive pseudorheumatoid dysplasia with secondary synovial chondromatosis. BMJ Case Rep 2020;13:e234461. [Google Scholar]
- 2.Wynne-Davies R, Hall C, Ansell BM. Spondylo-epiphysial dysplasia tarda with progressive arthropathy. A “new” disorder of autosomal recessive inheritance. J Bone Joint Surg Br 1982;64:442-5. [Google Scholar]
- 3.El Dessouki D, Amr K, Kholoussi N, Rady HM, Ali Temtamy S, Abdou MM, et al. Clinical and molecular characterization in a cohort of patients with progressive pseudorheumatoid dysplasia. Am J Med Genet A 2023;191:2329-36. [Google Scholar]
- 4.Giray E, Yağcı I, Elçioğlu HN. Progressive pseudorheumotoid dysplasia: A presentation of four cases with slow and rapid progression and effects of early rehabilitation program. Turk J Phys Med Rehabil 2019;65:290-7. [Google Scholar]
- 5.Liu Z, Chen X. Progressive pseudorheumatoid dysplasia: A case series report. Transl Pediatr 2021;10:1932-9. [Google Scholar]
- 6.Pulsatelli L, Manferdini C, Gabusi E, Mariani E, Ursini F, Ciaffi J, et al. Mesenchymal stromal cells from a progressive pseudorheumatoid dysplasia patient show altered osteogenic differentiation. Eur J Med Res 2022;27:57. [Google Scholar]
- 7.Segarra NG, Mittaz L, Campos-Xavier AB, Bartels CF, Tuysuz B, Alanay Y, et al. The diagnostic challenge of progressive pseudorheumatoid dysplasia (PPRD): A review of clinical features, radiographic features, and WISP3 mutations in 63 affected individuals. Am J Med Genet C Semin Med Genet 2012;160C:217-29. [Google Scholar]
- 8.Torreggiani S, Torcoletti M, Campos-Xavier B, Campos-Xavier B, Baldo F, Agostoni C, et al. Progressive pseudorheumatoid dysplasia: A rare childhood disease. Rheumatol Int 2019;39:441-52. [Google Scholar]
- 9.Outrequin A, Manon J, Paulmier A, Putineanu D, Docquier PL, Cornu O. Multiple joint replacements for progressive pseudorheumatoid dysplasia: A case report. J Orthop Case Rep 2024;14:18-23. [Google Scholar]
- 10.Yang X, Song Y, Kong Q. Diagnosis and surgical treatment of progressive pseudorheumatoid dysplasia in an adult with severe spinal disorders and polyarthropathy. Joint Bone Spine 2013;80:650-2. [Google Scholar]