Valgus deformity of the trochanter is a rare deformity of the proximal femur which can present with unique challenges during total hip arthroplasty. The reverse sleeve of S-ROM proves to be a reliable technique to secure adequate stem fixation negating the need for corrective osteotomies, and brings satisfying clinical outcomes.
Dr. Adarsh Krishna K Bhat, Department of Orthopaedics, Apollo Hospitals, Bannerghatta Road, Amalodbhavi Nagar, Bengaluru - 560076, Karnataka, India. E-mail: adarshbhat118@gmail.com
Introduction: It is rare to encounter a patient with severe valgus deformity of the greater trochanter with severe osteoarthritis of the hip joint. The treatment, that is total hip arthroplasty (THA) in such a case presents with a surgical challenge in proper placement of the femoral stem. Traditionally, an osteotomy procedure to correct the femoral deformity was warranted followed by THA. There are not many reported articles on such a case in English literature.
Case Report: A 75-year-old gentleman a known case of diabetes and hypertension, with a body mass index of 31.6 presents with a painful right hip joint. History reveals an osteotomy of the proximal femur done approximately 30 years back. After a thorough clinical and radiological examination, he underwent THA at our center.
Discussion: Trochanter valgus deformity is a rare deformity to come across. Often femoral osteotomy is considered to correct the deformity to aid in the insertion of the femoral stem. In this report, we state a different technique wherein the sleeve of the S-ROM femoral component (DePuy Orthopedics, Warsaw, Indiana) is placed in reverse fashion to overcome this complex situation, negating the need for osteotomy correction.
Conclusion: Deformity of the proximal femur can pose a significant technical challenge during THA. Modularity at the stem sleeve junction in the DePuy S-ROM system can prove to be efficient to secure good fixation in a femoral canal with deformities. Reverse sleeve placement proves to be reliable in the valgus deformity of the trochanter.
Keywords: Total hip arthroplasty, Trochanter valgus deformity, Reverse sleeve, S-ROM hip.
Valgus deformity of the trochanter is a rare type of proximal femoral deformity [1, 2]. For practical classification of complex total hip arthroplasty (THA), Berry [3] defined “deformed femur” as the femur that requires a special technique or implant due to the abnormal shape or size during arthroplasty. Proximal femoral deformities – mainly varus or valgus occur secondary to infection during childhood, fracture malunions, or after an osteotomy procedure. Before the advent of ceramics, highly cross-linked polyethylene and newer techniques in THA, valgus osteotomy of the trochanter was a useful treatment for developmental dysplasia of the hip and osteonecrosis of the femoral head [4,5]. In the presence of femoral deformities, THA is challenging due to the risk of intraoperative femoral fractures or perforations, stem malpositions, and failed stem fixations [3,6-10]. An appropriate type of femoral component can avoid such complications and improve clinical outcomes. The S-ROM femoral component is a cementless, modular, and cylindrical prosthesis specially designed for proximal femoral deformities [11]. Modularity at the stem sleeve junction allows the surgeon to decide the anteversion of the femoral stem independent of the sleeve position, which can best fit and occupy proximal femoral metaphysis. We report here a case of osteoarthritis (OA) of the right hip joint with valgus trochanter deformity with silver wainwright osteotomy plate and screws in situ which was treated with implant removal and primary THA.
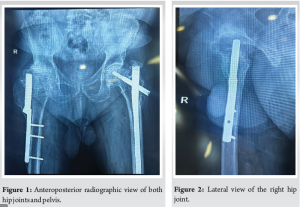
A 75-year-old male, with a known case of hypertension and Type II diabetes presented to our center with c/o pain in the right hip joint and difficulty in ambulation. On the elicitation of history, the patient had undergone a valgus osteotomy procedure of the right proximal femur after the history of fall, 30 years back and had an implant in situ. The details of the surgery and its indication were not available and couldn’t be recalled by the patient. He also sustained an intertrochantric fracture of the left proximal femur 10 years back which was treated with proximal femoral nailing. Clinical examination of the right hip joint revealed a linear scar of size approximately 20 cm on the lateral aspect of the proximal thigh. Range of movements of the hip was severely restricted and painful, with the abduction of 10°, 10° of adduction, 20° of flexion, and 5° of external and internal rotations with an antalgic gait. Limb length discrepancy was minimal. The pre-operative modified Harris Hip score recorded is 34. Radiological examination with X-rays of the pelvis with both hips and right hip lateral view (Fig. 1 and 2) revealed severe OA of the right hip with deformed head, valgus trochanter deformity with silver wainwright plate and screws in situ. Left hip shows united intertrochanteric fracture with OA changes in the hip joint with proximal femoral nail in situ.
After a detailed explanation of the risks and benefits to the patient and relatives, Implant removal and THA were planned and performed. The patient was followed up post-operative in 1st month, 3rd month, and 6th month and was assessed clinically and radiologically.
Surgical technique
After thorough pre-operative templating and planning, an incision was done over the previous scar site of about 20 cm. A posterolateral approach to the hip joint followed. The incision was deepened, soft tissue retracted and the implant was visualized, which had bony ingrowth. The bony ingrowth was removed using a chisel and the implant along with the screws removed (Fig. 3).
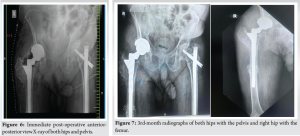
The femoral head was dislocated posteriorly and femoral neck osteotomy was performed. Acetabulum was exposed and serially reamed from 38 mm to 54 mm reamers. After ascertaining adequate inclination and anteversion, the trial of an acetabular cup of size 54 mm was inserted and assessed. The trial was removed and the acetabulum was packed with gauze. The entry site in the trochanter was identified and a small size reamer passed into the medullary canal. Subsequently, reamer size increased until the cortical bone of the proximal femur reached. During the reaming of the canal, the femoral shaft sustained a fracture at the distalmost screw site region; hence, further reaming was done holding the fracture site in a reduction to insert a longer stem that bypasses the fracture site. Proximal metaphyseal preparation was then carried. As the medial cortex is not able to support the S-ROM sleeve, the sleeve is placed in reverse fashion in the greater trochanter (Fig. 4). The calcar medially was resurfaced and the protruding bone osteotomised. To prevent subsidence, a large-size sleeve was adopted. The stem trial was done in an appropriate anteversion. The prosthetic components finally used were Pinnacle Porocoat Acetabular shell 54 mm with cancellous bone screw of size 6.5 × 35 mm, Pinnacle Marathon Polyethylene Acetabular Liner (+4 offset, 10° posterior lip), S-ROM porous coated proximal sleeve (Cone: B, Triangle: Large), S-ROM femoral stem Standard neck of size 18 × 13 × 215 mm and Biolox Delta Ceramic Femoral Head 36 mm. The stability of the joint (Fig. 5) and fracture site was ascertained after which the wound closed in layers after adequate hemostasis. No other perioperative complications were experienced except the intraoperative fracture shaft femur. The post-operative anterior-posterior view radiograph (Fig. 6) of both hip and pelvis revealed a well-placed acetabular cup, metaphyseal sleeve, and stem. The teardrop and lesser trochanter were at the same level compared to the contralateral side. Clinically there wasn’t recordable limb length discrepancy.
The patient was advised strict non-weight-bearing for the first 6 weeks, followed by clinical and radiological examination. Radiological examination revealed callus formation at the fracture site, after which he was mobilized partial weight bearing with walker support. 3rd month X-rays (Fig. 7) revealed a well-fixed prosthesis with well-formed callus and clinically patient was able to ambulate independently and carry out his routine activities using a stick with minimal discomfort or pain.
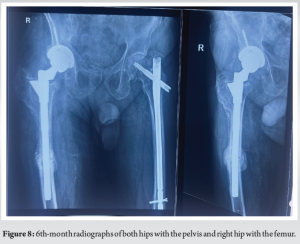
The 6th month X-rays (Fig. 8) revealed a united shaft of femur fracture with consolidated callus. The prosthesis components are well fixed with no evidence of loosening or subsidence. Clinically patient is completely pain-free and is able to carry out routine activities with comfort. At the 6th month follow-up, the recorded modified Harris Hip score was 77, which had improved significantly compared to the pre-operative state.
Deformity of the proximal femur raises significant challenges during THA. The strategy of THA varies along with the severity and position of the trochanter deformity [3]. Hip preserving surgeries that were performed on young patients with dysplastic hips, Avascular Necrosis of femoral heads, later present with arthritis with residual proximal femoral deformity, which poses technical challenges to the following THA [12]. Before the advent of newer prosthetic designs, if traditional tapered stems could not be passed inside the deformed femoral canal, a corrective osteotomy was warranted. This presented with a set of complex problems including a technically demanding surgery, risk of non-union, infections, increased operative time, and economic burden and this resulted in significantly inferior long-term outcomes. Customized prosthesis may provide an effective solution for severe femoral deformity [13-15]. Financial concerns however restrict the widespread use of customized prosthesis. As per the design of S-ROM, the angle formed between the femoral stem and sleeve can be adjusted as per the requirements, but in practice, it is rarely used beyond 90°. This method wherein we have placed the sleeve in the reverse fashion of 180° is seldom reported. Advantages of this technique include a well-fitting stem and sleeve with minimal bone loss. The need for osteotomy before THA is negated. The patient can be mobilized early and hence the recovery time is early. In our case, it has resulted in good clinical outcomes in 3rd month and 6th month follow-up. Limitations of this technique are that it may not be feasible to place the sleeve in reverse fashions in all the kind of deformities. Second, there is an increase in offset as the trochanter valgus deformity isn’t corrected, which can lead to trochanteric bursitis and pain. Third, there is a risk of intraoperative fractures. Limitations of our study include the unavailability of the details of the patient’s previous surgery and the lack of long-term follow-up of the patient.
THA in deformities of the proximal femur is a challenging procedure. Depuy S-ROM modular hip prosthesis system can prove to be efficient with flexibility in the sleeve position in respect with the femoral stem. The reverse sleeve of S-ROM was found to be a reliable technique for patients with severe valgus deformity of the trochanter and has proven to bring satisfying clinical outcomes in early and midterm follow-ups. Proper patient education and counseling regarding the need for specialized prosthetic components, increased duration of surgery, risk of perioperative fractures, infections revision surgeries, and information about post-operative rehabilitation protocols, are of paramount importance.
Management of hip OA with a deformity of the proximal femur can be challenging, due to the rarity of its occurrence and the limited availability of specialized prosthetic components to secure a good fixation. Depuy S-ROM with modularity in its sleeve placement can prove beneficial in such cases and can yield satisfactory results.
References
- 1.Iwase T, Hasegawa Y, Iwasada S, Kitamura S, Iwata H. Total hip arthroplasty after failed intertrochanteric valgus osteotomy for advanced osteoarthrosis. Clin Orthop Relat Res 1999;364:175-81. [Google Scholar]
- 2.Suzuki K, Kawachi S, Matsubara M, Morita S, Jinno T, Shinomiya K. Cementless total hip replacement after previous intertrochanteric valgus osteotomy for advanced osteoarthritis. J Bone Joint Surg Br 2007;89:1155-7. [Google Scholar]
- 3.Berry DJ. Total hip arthroplasty in patients with proximal femoral deformity. Clin Orthop Relat Res 1999;369:262-72. [Google Scholar]
- 4.Torchia ME, Klassen RA, Bianco AJ. Total hip arthroplasty with cement in patients less than twenty years old. Long-term results. J Bone Joint Surg Am 1996;78:995-1003. [Google Scholar]
- 5.Jingushi S, Sugioka Y, Noguchi Y, Miura H, Iwamoto Y. Transtrochanteric valgus osteotomy for the treatment of osteoarthritis of the hip secondary to acetabular dysplasia. J Bone Joint Surg Br 2002;84:535-9. [Google Scholar]
- 6.Papagelopoulos PJ, Trousdale RT, Lewallen DG. Total hip arthroplasty with femoral osteotomy for proximal femoral deformity. Clin Orthop Relat Res 1996;332:151-62. [Google Scholar]
- 7.Mortazavi SM, Restrepo C, Kim PJ, Parvizi J, Hozack WJ. Cementless femoral reconstruction in patients with proximal femoral deformity. J Arthroplasty 2011;26:354-9. [Google Scholar]
- 8.Kim JT, Yoo JJ. Implant design in cementless hip arthroplasty. Hip Pelvis 2016;28:65-75. [Google Scholar]
- 9.Khanuja HS, Vakil JJ, Goddard MS, Mont MA. Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am 2011;93:500-9. [Google Scholar]
- 10.Zhao HY, Kang PD, Shi XJ, Zhou ZK, Yang J, Shen B, et al. Effects of total hip arthroplasty on axial alignment of the lower limb in patients with unilateral developmental hip dysplasia (Crowe type IV). J Arthroplasty 2019;34:2406-14. [Google Scholar]
- 11.Biant LC, Bruce WJ, Assini JB, Walker PM, Walsh WR. The anatomically difficult primary total hip replacement: Medium-to long-term results using a cementless modular stem. J Bone Joint Surg Br 2008;90:430-5. [Google Scholar]
- 12.Chan-Woo P, Seung-Jae L, Youn-Soo P. Modular stems: Advantages and current role in primary total hip arthroplasty. Hip Pelvis 2018;30:147-55. [Google Scholar]
- 13.Wettstein M, Mouhsine E, Argenson JN, Rubin PJ, Aubaniac JM, Leyvraz PF. Three-dimensional computed cementless custom femoral stems in young patients: Midterm followup. Clin Orthop Relat Res 2005;437:169-75. [Google Scholar]
- 14.Flecher X, Argenson JN, Parratte S, Ryembault E, Aubaniac JM. Custom cementless stem for osteoarthritis following developmental hip dysplasia. Rev Chir Orthop Reparatrice Appar Mot 2006;92:332-42. [Google Scholar]
- 15.Flecher X, Parratte S, Aubaniac JM, Argenson JN. Cementless total hip arthroplasty using custom stem and reinforcement ring in hip osteoarthritis following developmental dysplasia. Hip Int 2007;17 Suppl:S120-7. [Google Scholar]