The case underscores the complexity of managing Giant Cell Tumors (GCTs) of the bone, underscoring the necessity for comprehensive treatment strategies, vigilant monitoring for recurrence, and the potential for limb-saving interventions amidst challenging clinical scenarios.
Dr. Love Kapoor, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India. E-mail: lovekapoor871988@rediffmail.com
Introduction: Giant cell tumor (GCT) of the bone, although benign, poses significant challenges due to its locally aggressive nature and high recurrence rates post-surgical intervention. Among skeletal GCTs, those affecting the distal radius present unique difficulties, especially when fungating masses encase vital structures such as blood vessels.
Case Report: We present a case of a 28-year-old male with a recurring GCT of the distal radius, where limb-preserving surgery was successfully performed despite encasement of the radial artery. Surgical excision followed by wrist arthrodesis utilizing ulnar centralization resulted in satisfactory outcomes, emphasizing the importance of tailored surgical approaches for optimal functional preservation. Despite encountering local recurrence, subsequent excision and reconstruction utilizing vacuum-assisted closure and skin grafting achieved successful limb salvage with no evidence of further recurrence at the 18-month follow-up.
Conclusion: This case study contributes valuable insights into rare limb salvage techniques applicable to challenging GCT presentations, advocating for personalized treatment strategies to mitigate recurrence risk and preserve patient quality of life.
Keywords: Fungation, limb-salvage, recurrence local, distal end radius, giant-cell tumor.
The giant cell tumor (GCT) of bone is a non-malignant yet locally aggressive growth, often treated through lesion removal-either through curettage or complete resection followed by reconstruction. Among skeletal GCTs, the distal radius ranks third (representing 10% of cases), following the distal femur and proximal tibia [1]. Under the microscope, these tumors display a mix of spindle-shaped stromal cells, osteoclast-like multinucleated giant cells, and the cluster of differentiation-68 positive mononuclear cells. The GCT typically presents a well-defined, non-hardened edge, often eccentrically located in long bones, occasionally extending close to the joint surface, especially in patients with closed epiphyses, rarely crossing the joint itself [2]. The primary hurdle in managing GCT lies in its tendency to locally reappear after surgical intervention: Recurrence rates ranging from 27 to 65% after isolated curettage; 12–27% following curettage with adjuncts such as high-speed burr, phenol, liquid nitrogen, or polymethylmethacrylate; and 0–12% after complete removal [3]. Distal radius GCT cases usually manifest in relatively smaller or medium sizes. However, larger and ulcerating GCTs in this area have a higher propensity to infiltrate, destruct, and compromise neighboring tissues, elevating the chances of complications such as potential amputation [4]. Radical amputation procedures remain prevalent for extensive tumors that breach the skin, leading to significant morbidity and disability. At present, there is scarce literature available on limb-preserving surgeries for such fungating tumors. We document a case involving a recurring GCT of the distal radius presenting a fungating mass that underwent a limb-preserving surgical procedure. The patient consented in writing, acknowledging the possibility of publication.
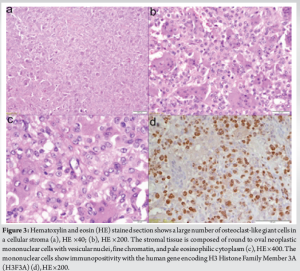
A 28-year-old right-handed male presented with a complaint of persistent pain and swelling in his right wrist over the past 6 months. The onset of symptoms was gradual, with the pain and swelling progressively worsening, and notably intensified in the last 1 month. Upon clinical examination, a globular swelling measuring 8 × 8 × 7 cm was observed on the right wrist. This swelling was tender to palpate, exhibited elevated local temperature, and was firmly attached to the underlying bone. The skin covering the swelling appeared stretched, with visible prominence of veins. Radiographic assessment through X-ray revealed an aggressive, expansive, osteolytic lesion affecting the epiphysis and extending into the metaphysis of the distal radius on the right side (Fig. 1). This lesion exhibited cortical breach and destruction of the bone just beneath the joint surface. Magnetic resonance imaging (MRI) imaging exhibited a tumor measuring 8.8 × 8.4 × 7.2 cm, showcasing cortical destruction and extension into adjacent soft-tissue areas (Fig. 2). Core needle biopsy was performed and subsequent histopathological analysis confirmed the diagnosis of GCT affecting the bone (Fig. 3).
The patient received two intravenous injections of zoledronic acid (4 mg) spaced 3 weeks apart. Following the second injection, a repeat X-ray revealed the lesion’s expansion and worsening condition, prompting the decision for surgical intervention. A wide resection of the tumor with meticulous dissection to save multiple encased tendons was performed with centralizing the ulna and conducting wrist arthrodesis using a 3.5 mm locking compression plate (Fig. 4).
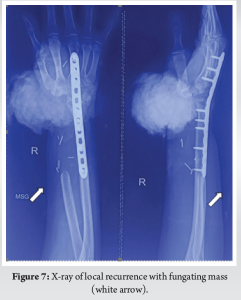
The patient was discharged after 5 days with a well-healing wound. Post-operative histopathological analysis indicated a 4.5 cm proximal bony margin and a <0.1 cm soft-tissue margin of the tumor. No malignant transformation was seen. Three months after the initial surgery, the patient reported swelling over the dorsal aspect of the wrist. Subsequent imaging (Fig. 5) suggested local recurrence, which was confirmed by histopathological analysis. Surgical excision of the recurrence was performed 3 months follow-up. The patient was lost to follow-up for the subsequent 6 months and later reappeared with a substantial, proliferating mass accompanied by active bleeding (Fig. 6). An urgent X-ray (Fig. 7) and MRI were performed, revealing a heterogeneous mass located in the distal radius, exhibiting a large exophytic component that extended to involve the right wrist and the first metacarpophalangeal joint. In addition, there was an indication of involvement in the distal radius artery segment, measuring 5.5 cm. The MRI did not visualize the flow void of the radial artery, possibly indicating thrombosis. However, the ulnar arteries displayed normal flow voids (Fig. 8). The patient was informed about the challenging prognosis for limb salvage. Following a thorough discussion of available treatment options, another attempt at excision was suggested.

A wide local excision of the mass was performed, followed by the application of vacuum-assisted closure (VAC). After 3 weeks of VAC treatment, the exposed area was covered with a split-thickness skin graft. Unfortunately, the radial artery had to be sacrificed during the surgical procedure. The histopathological analysis showed no atypical cells representing malignant transformation. The patient has been regularly attending outpatient department follow-ups for the past 18 months. No clinical and radiological sign of local recurrence or lung metastasis has been observed (Fig. 9). The hand function is satisfactory, with only mild weakness observed in thumb extension. At the final follow-up, the functional outcome was assessed using the Musculoskeletal Tumor Society scoring system [5], yielding a score of 27/30 (Fig. 10).
GCT of the distal radius presents challenges due to its local aggressiveness, high recurrence rates post-intralesional excision (curettage), and propensity for distant metastasis, frequently observed in the lungs. Inadequate residual subchondral bone support post-curettage may lead to joint collapse, degenerative osteoarthritis, and tumor recurrence [6]. In cases where extensive extraosseous involvement causes significant volar and dorsal cortical destruction, compromising structural integrity and joint viability, en bloc resection becomes necessary when curettage is unfeasible [7]. Multiple potential factors influencing the local recurrence of GCT have been documented, such as Campanacci grade [8], pathologic fracture, tumor location, adjuvant type [9], and whether the tumor is primary or recurrent. However, many studies that discuss these factors have a higher risk of confounding bias because they involve GCTs from all locations, thereby reducing the reliability of these factors in predicting recurrence [10]. Surgeons are continuously refining the preferred surgical approach to balance the risk of recurrence against the treatment’s morbidity. In situations where curettage is not feasible, salvaging the joint becomes challenging, requiring en bloc resection followed by effective reconstruction to maximize hand function preservation [7]. The literature outlines various wrist reconstruction methods, broadly categorized as restoring a flexible wrist or achieving a stable, immobile wrist through arthrodesis. Wrist arthrodesis involves different techniques, such as using bridging grafts such as allografts, vascularized or non-vascularized fibular autografts, iliac crest bone grafts, tibial cortical strut autografts, or utilizing the ipsilateral ulna through translocation or centralization [11-13]. In our study, we performed a procedure that involved wide excision of the tumor and utilizing a wrist fusion technique emphasizing the centralization of the ulna. Intravenous injections of zoledronic acid (4 mg) were given before first excision. However, radiation therapy was not used in this case. This methodology aims to minimize disruption to the muscles attached to the ulna, thereby preserving its vascular supply similar to a vascularized graft. This strategic approach maintains an advantageous biological milieu by safeguarding the ulnar blood supply and using compression plates to ensure stable fixation. Consequently, this promotes osseous union at the fusion site. In addition, repositioning the ulna contributes to a reduction in wrist dimensions, facilitating enhanced coverage of soft tissues and effective skin closure during the reconstructive phase, especially for patients with extensive soft-tissue involvement. Ultimately, this approach eliminates the need for additional soft-tissue procedures. Kapoor et al. [7] concluded that centralization of the ipsilateral ulna with wrist arthrodesis is a simple and effective modality of reconstruction after resection of distal radial tumors. It provides good functional outcomes and preservation of good hand grip strength, with low complication rates. In our case, we successfully preserved a limb affected by a recurring fungating mass that had encased the radial artery. Typically, amputation is the prevalent approach for handling extensive GCT tumors due to their advancing and harmful characteristics [2]. However, since GCT is not classified as a true malignancy and exhibits a low recurrence and metastasis rate, there exists a greater potential to maintain both the structure and function of the limb. Consequently, opting for limb salvage surgery represents a promising strategy for addressing large and fungating GCT cases [4]. The circulation to the hand was sustained through the utilization of ulnar arteries and their collateral vessels. The findings from this study are anticipated to inspire fellow surgeons to consider engaging in limb salvage surgery for fungating GCT masses with encased vessels, particularly in young and physically active patients. Furthermore, our experience sheds light on rarely reported limb salvage surgical approaches applicable to these specific cases.
In the realm of bone pathology, GCT is often distinguished from typical malignancies due to its distinct clinical behavior and histopathological features. While it lacks the classical hallmarks of malignancy, such as uncontrolled growth and metastatic potential, GCT can exhibit locally aggressive behavior, notably when involving vascular structures. In clinical scenarios where GCTs encase blood vessels, particularly in younger, physically active patients with a promising life expectancy, limb salvage procedures should be vigorously pursued. This approach aligns with the objective of preserving limb function and quality of life while addressing the local aggressive nature of GCT. However, meticulous assessment and individualized treatment strategies remain crucial to effectively manage these cases and minimize the risk of recurrence or functional impairment.
Vigorous pursuit of limb salvage is recommended for GCT encasing blood vessels in young, active patients to preserve function and quality of life.
References
- 1.Salunke AA, Shah J, Warikoo V, Chakraborty A, Pokharkar H, Chen Y, et al. Giant cell tumor of distal radius treated with ulnar translocation and wrist arthrodesis. J Orthop Surg (Hong Kong) 2017;25:2309499016684972. [Google Scholar]
- 2.Rangaswamy N, Kumar VS, Banjara R, Majeed A, Goyal D, Khan SA. Limb salvage surgery in fungating giant cell tumors: A report of three cases. J Orthop Case Rep 2021;11:19-23. [Google Scholar]
- 3.Zhang J, Li Y, Li D, Xia J, Li S, Yu S, et al. Clinical effects of three surgical approaches for a giant cell tumor of the distal radius and ulna. Mol Clin Oncol 2016;5:613-7. [Google Scholar]
- 4.Budi MN, Abidin A. Limb salvage surgery in large and fungating giant cell tumors of distal radius: A case series. Indones J Cancer 2023;17:133-9. [Google Scholar]
- 5.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993;286:241-6. [Google Scholar]
- 6.Agrawal AC, Garg AK, Choudhary R, Verma S, Dash RN. Giant cell tumor of the distal radius: Wide resection, ulna translocation with wrist arthrodesis. Cureus 2021;13:e15034. [Google Scholar]
- 7.Kapoor L, Banjara R, Sahoo B, Kumar VS, Ansari MT, Khan SA. Functional outcomes of centralization of the ulna as a method of reconstruction following resection of campanacci grade 3 giant cell tumor of the distal radius. J Hand Surg Am 2024;49:63.e1-9. [Google Scholar]
- 8.Teixeira LE, Vilela JC, Miranda RH, Gomes AH, Costa FA, de Faria VC. Giant cell tumors of bone: Nonsurgical factors associated with local recurrence. Acta Orthop Traumatol Turc 2014;48:136-40. [Google Scholar]
- 9.Arbeitsgemeinschaft Knochentumoren, Becker WT, Dohle J, Bernd L, Braun A, Cserhati M, et al. Local recurrence of giant cell tumor of bone after intralesional treatment with and without adjuvant therapy. J Bone Joint Surg Am 2008;90:1060-7. [Google Scholar]
- 10.Zou C, Lin T, Wang B, Zhao Z, Li B, Xie X, et al. Managements of giant cell tumor within the distal radius: A retrospective study of 58 cases from a single center. J Bone Oncol 2018;14:100211. [Google Scholar]
- 11.Grandizio LC, Maschke S. Wrist arthrodesis with femoral head structural allograft after failed total wrist arthroplasty. Tech Hand Up Extrem Surg 2017;21:116-20. [Google Scholar]
- 12.Clarkson PW, Sandford K, Phillips AE, Pazionis TJ, Griffin A, Wunder JS, et al. Functional results following vascularized versus nonvascularized bone grafts for wrist arthrodesis following excision of giant cell tumors. J Hand Surg Am 2013;38:935-40.e1. [Google Scholar]
- 13.Qu H, Guo W, Li D, Yang Y, Wei R, Xu J. Functional results of wrist arthrodesis versus arthroplasty with proximal fibula following giant cell tumour excision of the distal radius. J Hand Surg Eur Vol 2019;44:394-401. [Google Scholar]