Course of treatment and rehabilitation of fractures of the femur, tibia, and ankle in the same lower limb.
Dr. Ryunosuke Fukushi, Department of Orthopaedic Surgery, Sapporo Medical University, School of Medicine, S1 W16, Sapporo, Hokkaido, 060-8543, Japan. E-mail: ryunosuke_fukushi_521@yahoo.co.jp
Background: Few studies have reported the treatment and rehabilitation of combined fractures of the femur, tibia, and ankle in the same lower limb.
Case Report: A 69-year-old man presented to our hospital with a fall injury due to high-energy trauma after falling from a 5 m ladder while painting and landing on both feet. Examination revealed right femoral supracondylar; left tibial plateau; right calcaneal; left ankle crush; first and third lumbar vertebrae burst; sacral; C7, Th1, and Th9 compression; and bilateral acetabular fractures. External fixation of both femurs and tibias was performed on the day of injury. After the patient’s general condition had stabilized, a two-stage operation was performed on the 8th day after injury for osteosynthesis of the left tibial plateau and right calcaneus fractures and ilizarov fixation of the left ankle crush fractures. In addition, the right femoral supracondylar fracture underwent osteosynthesis on day 15 after the injury, while the burst fractures of the first and third lumbar vertebrae underwent posterior fixation on day 24. The sacral fracture; C7, Th1, and Th9 compression fractures; and acetabular fractures were treated conservatively with a brace and no weight-bearing until the ilizarov apparatus was removed and gait training started. The ilizarov apparatus was removed 90 days after application. Mild passive and active assist rehabilitation on both toes and knees was started the day after the injury. Wheelchair transfer training was started 51 days after the injury. On day 60, trunk stability and swaying were eliminated and strength training in the sitting position was started. On day 107, the patient transferred without assistance (supervised). On day 121, weight-bearing and short-term standing training (right lower limb only) was started. On day 141, weight-bearing on both lower limbs was started. On day 148, the patient walked approximately 100 m using a walking aid. On day 176, the patient walked twice on parallel bars and 4 m with Lofstrand coupling while wearing a patellar-tendon-bearing orthosis. At 212 weeks, the patient walked long distances and use the Lofstrand for 100 m. The patient could also change direction smoothly.
Conclusion: This study reports the treatment and rehabilitation of an elderly patient with bilateral compound fractures of the lower leg. The patient underwent long-term rehabilitation on the floor using the ilizarov method; however, with appropriate rehabilitation, he recovered to the point where he could walk.
Keywords: Rehabilitation, bilateral, fractures, lower leg, ilizarov.
While combined fractures of the femur, tibia, and ankle in the same lower limb are often difficult to treat, few studies have reported the course of treatment and rehabilitation. Furthermore, few reports have described the management and rehabilitation of patients with compound bilateral lower leg fractures. We report a case of bilateral compound fractures of the lower leg in an elderly patient who was eventually able to walk and was discharged from the hospital, along with a detailed course of treatment and rehabilitation. In addition, such cases are often encountered in emergency situations, and orthopedic surgeons are required to make quick decisions and determine treatment plans. In this study, we will organize the treatment plans and rehabilitation for the severe bilateral lower leg injuries; we experienced and add a literature review.
A 69-year-old man presented to our hospital following a traumatic fall from a height (high-energy trauma). He had sustained injuries after falling from a 5 m ladder while painting. He landed on both feet. The patient was transported to our hospital by helicopter because of a deformity and swelling in both lower limbs. His medical history included diabetes mellitus, alcoholic hepatitis, emphysema, and post-operative gastric cancer. Physical examination upon arrival revealed that a Japan coma scale score of I-2, a Glasgow coma scale score of 4–4–6, blood pressure of 137/63 mmHg, pulse 85 beats/min, oxygen saturation of 100% (room air), no airway obstruction, no difference in chest movement between sides, no subcutaneous emphysema, no obvious external bleeding, Facial drooping, Arm weakness, Speech difficulties and Time score negativity, and no pelvic mobility were also observed. Chest radiography revealed no obvious hemopneumothorax and pelvic radiography revealed bilateral acetabular fractures. As no immediate D findings were available, the patient was referred for a second examination. Various close-up examinations were performed as both the knee and ankle joints were swollen, and lumbar back pain was observed. Close examination revealed a right femoral supracondylar fracture (Fig. 1a); left tibial plateau fracture (Fig. 1b); right calcaneal fracture (Fig. 1c); left ankle crush fracture (Fig. 2); first and third lumbar vertebrae burst fractures (Fig. 3); sacral fracture; C7, Th1, and Th9 compression fractures, and acetabular fractures (Fig. 4).

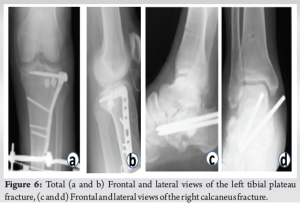
External fixation of both femurs and tibias was performed on the day of injury (Fig. 5). After the patient’s general condition had stabilized, a two-stage operation was performed on the 8th day after the injury, which included osteosynthesis of the left tibial plateau fracture and right calcaneus fractures (Fig. 6) and ilizarov fixation of the left ankle crush fractures (Fig. 7). In addition, the right femoral supracondylar fracture was treated with osteosynthesis on day 15 after the injury (Fig. 8a and b) while the burst fractures of the first and third lumbar vertebrae underwent posterior fixation on day 24 after the injury (Fig. 8c and d). The sacral fracture, C7, Th1, and Th9 compression fractures, and acetabular fractures were treated conservatively with a brace and no weight-bearing until the Ilizarov apparatus was removed and gait training started. The ilizarov apparatus was removed 90 days after its application.


Rehabilitation was started on the day after the injury. Mild passive and active assist rehabilitation was performed on both toes and both knees. On the 38th day after the injury, the same rehabilitation was added to both hip joints, with 20 repetitions on each side. On the 51st day, wheelchair transfer training was started. On the 60th day, when the trunk was stable and mobility had returned, strength training in a sitting position was started. On the 67th day after the injury, the patient was able to transfer to a wheelchair with an assistant. While on the 107th day, the patient started weight loading and short standing training (right lower limb only). On day 141, he was able to load with both lower limb orthoses. On day 148, he was able to walk with a walking aid for a distance of approximately 100 m. On day 176, he was able to perform two rounds on the parallel bars with the patellar-tendon-bearing orthosis. On day 177, he was able to walk 4 m with a Lofstrand coupling. On day 212, the patient was able to walk long distances of approximately 100 m with Lofstrand coupling and an applied gait and could also change direction smoothly. On day 214, the patient was transferred to the general ward and continued strength training of the antigravity muscles, balance training, and gait training and was discharged from the hospital.
Combined fractures of the femur and tibia in the same lower limb, also known as floating knee, were first described by Blake et al. in 1975 [1]. These fractures are often caused by high-energy trauma and are difficult to treat because they can lead to life-threatening conditions and are complicated by severe soft tissue damage [2]. The present case was not strictly a floating knee, as it did not involve a combination of the femur and tibia. However, we consider this to be a similar condition. Notably, the present case involved compound fractures in both lower legs. The complications that merit consideration include (1) multiple trauma and fractures, (2) vascular injuries, (3) soft tissue injuries, and (4) knee ligament injuries [3]. In the present case, the burst fractures of the first and third lumbar vertebrae, the sacral fractures, the compression fractures of C7, Th1, and Th 9, and both acetabular fractures were observed as multiple trauma and multiple fractures; however, vascular, soft tissue, and knee ligament injuries were not observed, nor did any patient present any vital abnormalities. In previous reports, the factors affecting functional prognosis included the presence or absence of knee fractures and the degree of open tibia fracture. The complications affecting life prognosis included infection and pulmonary complications (acute respiratory distress syndrome, pulmonary embolism) [4, 5]. During the course of treatment, pulmonary embolism is a complication that must be watched for. Patients with spinal cord injury who also have bilateral lower limb paralysis, venous thromboembolism occurs in 0.2–31% of cases [6] and the rate of pulmonary embolism is 0.06–18% [7], and the mortality rate has been reported to be 11.9% in Japan [8]. Pulmonary embolism may be accompanied by sudden back pain. Prevention is the most important thing when it comes to pulmonary embolism, and the authors have used foot pumps, early rehabilitation interventions, and anticoagulants to prevent DVT in all cases. D-dimer is also an effective marker for detecting venous thromboembolism and pulmonary embolism. The authors regularly measure D-dimer, and if D-dimer levels are elevated, they perform lower extremity ultrasound and contrast CT to assess for the presence of a blood clot. As a treatment strategy, Lundy et al. recommended first performing fixation of the femur in compound fractures of the lower leg. This is because the tibia and ankle joint can often be immobilized even in patients with poor general conditions and with intratibial fixation (especially intramedullary nails), with potential for soft tissue damage in the femur due to hyperflexion of the knee [9]. In the present case, external fixation was performed on both lower legs to reduce swelling, followed by planned internal fixation; however, because it was a local hospital and there was a shortage of staff, and it took a long time for the internal fixation materials to arrive after we ordered, the femur was not fixed in the right femoral supracondylar fracture, which did not cause any problems. In this case, the comminuted fracture of the left ankle joint was selected to undergo the ilizarov procedure, as the degree of comminution was so severe that internal fixation would be difficult. This procedure is well-known for its advantages, which are: (i) minimal surgical invasion with less infection owing to the use of durable wires; (ii) easy handling and maintenance of the correct position and orientation of bone fragments; (iii) accurate correction, secure bone fusion, and bone lengthening; and (iv) use in patients with complex deformities and bone defects. In the present case, the patient could only be rehabilitated in bed for the duration of the ilizarov procedure, which is a concern because the patient was elderly. However, the patient recovered and was able to walk even though weight training was started 121 days after the injury. The ability of a patient to receive sensory input from the outset without significant sensory loss is an important factor. In recent years, reports have proposed electrical stimulation therapy, such as functional and therapeutic electrical stimulation, in cases where multiple traumas to both lower limbs have resulted in prolonged bed rest after injury. Electrical stimulation therapy is in addition to early muscle strengthening, joint mobilization, and gait training to prevent muscle and nervous system decline. In addition, a gait rehabilitation robot combined with the aforementioned functional electrical stimulation was developed and implemented at the author’s collaborating institution [10]. The combined use of functional electrical stimulation and robots can significantly reduce knee and hip joint torque and provide effective rehabilitation. In the future, this combination of medical technologies may provide more effective rehabilitation. Early gait training may be possible in cases such as the present case, in which the patient is still forced into a period of unloading after bone union. The secondary effects of early gait training are expected to include (1) reduced spasticity, (2) normalized heart rate and blood pressure regulation, (3) improved urinary and bowel function, (4) increased bone density and osteoporosis prevention, (5) contributions to lifestyle-related diseases (such as improved blood sugar and lipid metabolism), (6) psychological effects, and (7) pressure sore prevention.
This study reports the treatment and rehabilitation of an elderly patient with bilateral compound fractures of the lower leg who was eventually able to walk and was discharged from the hospital. The patient underwent long-term rehabilitation on the floor using the Ilizarov method; however, with appropriate rehabilitation, he recovered to the point where he could walk.
For cases of severe trauma to both lower limbs, it is important to provide appropriate initial treatment and decide on a treatment plan.
References
- 1.Blake R, McBryde A Jr. The floating knee: Ipsilateral fractures of the tibia and femur. South Med J 1975;68:13-6. [Google Scholar]
- 2.Fraser RD, Hunter GA, Waddell JP. Ipsilateral fractures of the femur and tibia. J Bone Joint Surg Br 1978;60-B:510-5. [Google Scholar]
- 3.Paul GR, Sawka MW, Whitelaw GP. Fractures of the ipsilateral femur and tibia: Emphasis on intra-articular and soft tissue injury. J Orthop Trauma 1990;4:309-14. [Google Scholar]
- 4.Karlstrom G, Olerud S. Ipsilateral fracture of the femur and tibia. J Bone Joint Surg Am 1977;59:240-3. [Google Scholar]
- 5.Carter RE. Respiratory aspects of spinal cord injury management. Paraplegia 1987;25:262-6. [Google Scholar]
- 6.Solaru S, Alluri RK, Wang JC, Hah RJ. Venous thromboembolism prophylaxis in elective spine surgery. Glob Spine J 2021;11:1148-55. [Google Scholar]
- 7.Inoue H, Watanabe H, Okami H, Kimura A, Takeshita K. The rate of venous thromboembolism before and after spine surgery as determined with indirect multidetector CT. JB JS Open Access 2018;3:e0015. [Google Scholar]
- 8.Stahel PF, VanderHeiden T, Flierl MA, Matava B, Gerhardt D, Bolles G, et al. The impact of a standardized “spine damage-control” protocol for unstable thoracic and lumbar spine fractures in severely injured patients: A prospective cohort study. J Trauma Acute Care Surg 2013;74:590-6. [Google Scholar]
- 9.Lundy DW, Johnson KD. “Floating knee” injuries: Ipsilateral fractures of the femur and tibia. J Am Acad Orthop Surg 2001;9:238-45. [Google Scholar]
- 10.Inoue J, Kimura R, Shimada Y, Saito K, Kudo D, Hatakeyama K, et al. Development of a gait rehabilitation robot using an exoskeleton and functional electrical stimulation: Validation in a pseudo-paraplegic model. Prog Rehabil Med 2022;7:20220001. [Google Scholar]









