Highlighting the atypical presentation of tuberculosis in the wrist underscores the importance of considering uncommon locations for the disease. This case emphasizes the need for vigilant clinical evaluation and awareness among healthcare professionals to ensure timely diagnosis and appropriate management, ultimately improving patient outcomes.
Dr. Palak Gupta, Department of Medicine, Maharishi Markandeshwar Institute of Medical Sciences and Research (MMIMSR), Ambala, Haryana, India. E-mail: palakg371@gmail.com
Introduction: Tuberculosis (TB) of the wrist joint is a rare presentation of extrapulmonary TB, accounting for about 1% of musculoskeletal TB cases. We present a case of wrist joint TB in a 15-year-old immunocompetent male patient.
Case Report: A 15-year-old boy presented with 6- month history of left wrist swelling and pain along with constitutional symptoms for 2 months. Examination showed swelling, tenderness, and reduced range of wrist motion. Investigations revealed elevated inflammatory markers, lytic lesions on wrist X-ray, and positive polymerase chain reaction ( ) for Mycobacterium tuberculosis in synovial fluid. Histopathology of synovial biopsy demonstrated caseating granulomas, confirming the diagnosis- treatment with 6 months of anti-tubercular therapy led to complete resolution.
Conclusion: Though rare, wrist joint TB should be a diagnostic consideration in patients with chronic wrist symptoms. A high index of suspicion and early diagnosis using microbiological, radiological, and histopathological investigations prevents morbidity.
Keywords: Tuberculosis, extrapulmonary, wrist joint, case report.
Tuberculosis (TB) remains a major global public health concern despite significant advances in diagnosis and treatment. In 2019, about 10 million people developed symptomatic TB disease, and 1.4 million died from it worldwide [1]. The etiological agent, Mycobacterium tuberculosis, most commonly affects the lungs, causing pulmonary TB, but can also affect other organs, causing extrapulmonary TB (EPTB) [2]. Around 15–20% of all TB cases are extrapulmonary, and musculoskeletal sites are the third most common location for EPTB, accounting for 10 –20% of cases after lymph nodes and pleural effusions [3, 4]. Any bone or joint can be involved in musculoskeletal TB, with the weight-bearing spine and large joints being more susceptible. Isolated involvement of the wrist joint is rare and is reported to occur in 1% or fewer cases of skeletal TB [5, 6]. Due to its rarity, atypical presentation, and radiological similarities with other conditions, wrist joint TB poses diagnostic challenges, often delaying timely treatment [7]. We present a case of wrist joint TB in a 15-year-old boy who was successfully treated with anti-tubercular therapy.
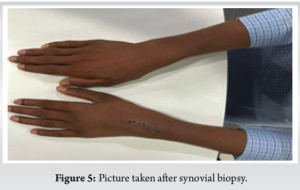
A 15-year-old boy presented with progressive swelling and pain of the left wrist for 6 months. He also complained of an evening rise in temperature, night sweats, and loss of appetite for 2 months. He denied any history of wrist trauma, TB contact, chronic cough, or treatment for TB in the past. On examination, there was a diffuse, mildly tender swelling of 4 ×4 cm, more pronounced over the dorsal aspect of the left wrist joint (Fig. 1-3). The local temperature was raised, and the overlying skin appeared inflamed. Wrist movements were painfully restricted (flexion/extension range 0-15°). Distal neurovascular status and systemic examination, including chest examination, were unremarkable. Blood counts and biochemical investigations were within the normal range, apart from raised erythrocyte sedimentation rates (ESR) (46 mm/h). Human immunodeficiency virus serology was non-reactive; the Mantoux test was positive (induration 12 mm). X-ray of the wrist joint showed destructive lytic lesions, mainly involving carpal bones and bases of the 2nd–5th metacarpals (Fig. 4). Synovial fluid analysis revealed turbid fluid with protein of 4.5 g/dL, glucose of 25 mg/dL (blood glucose 98 mg/dL), leucocytes 1200/cumm (90% neutrophils), and no crystals. The Ziehl-Neelsen (ZN) stain did not show acid-fast bacillus, while TB-polymerase chain reaction (PCR) was positive. A decision was made to go ahead with a synovial biopsy, open synovial biopsy was done (Fig. 5). Histology samples showed caseating granulomas comprising epithelioid cells, Langerhans giant cells, and lymphocytic aggregates. The diagnosis of EPTB affecting the carpal bones was made. The patient was started on anti-TB treatment, which was continued for 9 months and eventually stopped as symptoms resolved and subsequent TB-PCR was negative. He was immobilized with a wrist splint and underwent physiotherapy during treatment. At the final follow-up at 9 months, he was asymptomatic with no clinical signs of active disease and normal follow-up X-ray.

The musculoskeletal system ranks as the third most prevalent site for TB , following the lungs and lymph nodes, constituting approximately 10–20% of EPTB cases [1]. Among these, bone TB predominantly affects weight-bearing joints, with a notable impact on large joints, such as the spine, hip, and knee. Wrist TB, a rarity accounting for nearly 1% of EPTB instances, poses diagnostic challenges during the initial assessment. The complexity arises due to multiple potential differentials, including subacute or chronic suppurative arthritis, osteochondrosis, rheumatoid arthritis, Kaposi sarcoma, and benign bone tumors [8], and all the differentials were ruled out in our patient. Patients typically present with non-specific local symptoms such as joint pain, swelling, stiffness, and wound discharge, often accompanied by systemic manifestations, such as fever, night sweats, and weight loss [7]. Inflammation commonly results in elevated ESR and C-reactive protein levels, though atypical TB may exhibit normal values. Clinical investigation’s sensitivity varies, with Z N staining showing only 20%, PCR 63%, histological examination 65%, and mycobacterium culture 80% sensitivity [9]. Approximately, one-third of wrist TB cases coincide with pulmonary infection, while two-thirds manifest in isolation [10, 11]. Initial evaluation involves plain radiography of the wrist, complemented by a chest radiograph to ascertain concomitant pulmonary TB. Plain wrist radiography typically reveals sclerosis and osteolytic lesions in the carpal and other affected bones, although such findings are non-specific and may mimic conditions, such as pyogenic osteomyelitis, inflammatory arthritis, or malignancy [11]. While computed tomography and Magnetic Resonance Imaging scans lack specificity, they aid in assessing swelling extent, and ultrasound serves as an additional tool for evaluating swelling. Confirmation of diagnosis involves identifying M. tuberculosis in cultures and observing a histological pattern typical for TB. This pattern typically consists of necrotizing granulomatous inflammation characterized by epithelioid histiocytes surrounding a central caseating necrotic zone, accompanied by multinucleated giant cells (Langerhans cells) and lymphocytes [12]. Treatment for wrist TB is primarily non-operative, involving a regimen of anti-TB medications. The World Health Organization’s 2019 guidelines recommend a 2-month intensive phase with rifampicin, isoniazid, ethambutol, and pyrazinamide, followed by a 4-month continuation phase with rifampicin and isoniazid [13]. Most cases (approximately 75%) respond successfully to medication, resulting in favorable hand and wrist functional outcomes. Surgery is advised in cases involving nerve compression, impending bone collapse, or the necessity for joint debridement, drainage of large abscesses, or deformity correction in the context of healed disease [13].
TB of the wrist joint is uncommon, constituting about 1% of skeletal TB. Due to the unusual location and vague initial symptoms, diagnosis is often delayed, leading to morbidity. Our case highlights the need for maintaining a high index of suspicion for TB in endemic countries. Targeted investigations exploring cytological, microbiological, radiological, and histological aspects are essential to confirm the diagnosis. Timely and proper treatment ensures excellent outcomes in the majority without the need for surgery. Reporting of such cases will help improve understanding and management of this rare manifestation of EPTB.
TB tenosynovitis in the wrist is an uncommon manifestation, making this case report valuable for highlighting the diversity of presentations of TB. The rarity of the condition underscores the need for awareness among clinicians. Since pain and swelling of the wrist joint arouse a number of differentials that are much more common compared to TB of the wrist, it can be misdiagnosed, leading to delay in treatment, worsening of conditions, and unnecessary use of drugs. Hence, it is important to bring this condition to light so that physicians can also consider it while diagnosing, especially in TB-prone regions.
References
- 1.World Health Organization. Global Tuberculosis Report 2020. Geneva: World Health Organization; 2020. [Google Scholar]
- 2.Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). 2015;78(2):47-55. doi:10.4046/trd.2015.78.2.47. [Google Scholar]
- 3.Golden MP, Vikram HR. Extrapulmonary tuberculosis: An overview. Am Fam Physician 2005;72:1761-8. [Google Scholar]
- 4.Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis 2009;49:1350-7. [Google Scholar]
- 5.Sankaran B. Tuberculosis of bones and joints. Indian J Tuberc 1993;40:109-18. [Google Scholar]
- 6.Davidson PT, Horowitz I. Skeletal tuberculosis. A review with patient presentations and discussion. Am J Med 1970;49:77-84. [Google Scholar]
- 7.Moorthy LN, Vallurupalli S. Isolated tuberculosis of wrist without obvious osseous involvement: A rare presentation. BMJ Case Rep 2013;2013:bcr2013009743. [Google Scholar]
- 8.Tuli SM. General principles of osteoarticular tuberculosis. Clin Orthop Relat Res 2002;398:11-9. [Google Scholar]
- 9.Farghaly NF, Shedid HH. Undetected wrist tuberculosis for three decades. Egypt Rheumatol 2019;41:197-9. [Google Scholar]
- 10.Cheung H, Pho RW, Lee SS. Tuberculous infection of the wrist--a case report. Hand Surg 2002;7:261-5. [Google Scholar]
- 11.Karki DB, Singh RK, Jha BK. Outcome of wrist tuberculosis treated conservatively in sporadic cases: Cohort study. J Global Infect Dis 2018;10(3):129-33. Jain R, Sawhney M, Berry M. Computed tomography of isolated tuberculosis of capitate. Australas Radiol 1993;37:201-2. [Google Scholar]
- 12.Blakemore R, Story E, Helb D, Kop J, Banada P, Owens MR, et al. Evaluation of the analytical performance of the Xpert MTB/RIF assay. J Clin Microbiol 2010;48:2495-501. [Google Scholar]
- 13.World Health Organization. WHO Consolidated Guidelines on Drug-resistant Tuberculosis Treatment. Geneva: World Health Organization; 2019. Available from: https://apps.who.int/bookorders [Google Scholar]