Exploring the impact of FHAVN post-COVID-19 on hip arthroplasty trends and creating an awareness to develop prophylactic measures to tackle the current burden and avert future occurrences.
Dr. R Aishwarya, Department of Orthopaedics, Jagadguru Jayadeva Murugarajendra Medical College, Davangere, Karnataka, India. E-mail: aish29ramki@gmail.com
Introduction: Coronavirus disease 2019 (COVID-19) infection or corticosteroid usage during the COVID-19 pandemic as risk factors for avascular necrosis (AVN) of the femoral head (osteonecrosis of the femoral head/femoral head AVN [FHAVN]), as well as its link to clinical and radiological outcomes, are poorly understood. Osteonecrosis, which results from a disruption in vascular supply to the femoral head, is a prevalent cause of hip joint deterioration and one of the most common reasons for total hip arthroplasty (THA)/total hip replacement in India and other Asian countries. This study will aid in understanding the condition’s epidemiology and statistically determining the risk of disease related with pandemic exposure.
Materials and Methods: This is a retrospective study of 100 hips diagnosed with osteonecrosis/osteoarthritis of the femoral head that underwent THA at a tertiary care center before and after the COVID-19 pandemic between February 2014 and February 2024.
Results: Late stages of FHAVN, when the diagnosis requiring THA, following the pandemic have increased exponentially. It has also switched from affecting the middle-aged to the younger age groups. Furthermore, the bilaterality necessitating THA has increased considerably. There is a clear shift in the presentation of this disabling illness, as well as the need for THA, which otherwise is rarely carried out on younger people. Furthermore, data on how much corticosteroids were used in the treatment is disturbingly scant, and how it may have contributed to this ailment in India is still questionable.
Conclusion: The COVID-19 pandemic could be the most serious threat, causing late-stages FHAVN (stages 3 and 4 of the Ficat and Arlet classification), in an accelerated manner, necessitating THA and overburdening existing medical care.
Keywords: COVID-19, pandemic, osteonecrosis, femoral head, osteonecrosis of the femoral head/femoral head avascular necrosis, India, Asia, total hip replacement/total hip arthroplasty.
Osteonecrosis of the femoral head (ONFH) is a crippling hip joint disease primarily affecting young people [1]. The genesis, natural history, and epidemiology of ONFH remain largely unknown. ONFH is associated with a wide range of conditions and drugs. The emergence and resurgence of coronavirus disease 2019 (COVID-19) infection, which is still prevalent globally in low-grade form, is one such condition that has occurred recently. While COVID-19 infection and avascular necrosis (AVN) are prevalent, little research has been published on their association. AVN or osteonecrosis has been observed in several joints, including the knees, shoulders, and spine. However, the hip joint is the most commonly affected [2-6]. Although many issues with COVID-19 remain unanswered, numerous research and reports have indicated a substantial prothrombotic condition on both a micro and macrovascular level in patients with this infection. There is limited evidence that COVID-19 can cause AVN. The most frequent cause of ONFH is the judicial use of corticosteroids, which were once again extensively used during the pandemic to treat COVID-19 infection because they were a life-saving medication. According to new research, COVID-19 has a deleterious effect on multiple body systems as part of “long COVID-19.” The phrase “long COVID-19” refers to the long-term consequences of COVID-19 infection that linger for several weeks or months following the patient’s recovery. In addition, it was described by the National Institute for Health and Care Excellence as symptoms that persisted for longer than 12 weeks [7-9]. ONFH risk increased in tandem with the COVID-19 infection. It is impossible to ignore the connection between COVID-19 infection and ONFH given the incomplete understanding of its sequelae. In light of this, research on the etiopathogenesis of ONFH in the population of south India is lacking, especially with regard to its connection to COVID-19 infection. Treatment options for hip osteonecrosis are many in number, ranging from joint preservation measures and non-operative care to total hip replacement (THR). When an early diagnosis is made before the lesion has grown too large or there is radiographic evidence of femoral head collapse, non-operative or joint-conserving treatment may enhance the results. Primary THR is frequently the only effective therapy option available because many individuals present after the illness has progressed, especially for Stage 3 and 4 of Ficat and Arlet classification for osteonecrosis femoral head [10-12]. As a result, the recent increase in THR caused by ONFH piqued our interest in conducting this study.
Objectives
To study the change in trend among patients who underwent total hip arthroplasty (THA) (THR) before and after COVID-19 pandemic. That is
- To analyze the presentation of osteonecrosis femoral head pre- and post-COVID-19 pandemic
- To study the demographic variation, in the indication of total hip surgery
- To understand the association of COVID-19 infection with osteonecrosis femoral head
- To study the association of corticosteroid intake during pandemic, to osteonecrosis femoral head.
This study includes 100 hips that underwent THR at our center.
Study design
This was a retrospective comparative study.
Study period
The study period was between February 2014 and February 2024 (5 years before and 5 years after COVID-19 pandemic, 2019 as a reference point).
Statistical analysis
Analysis of variance Statistical Packages for the Social Sciences (SPSS) version 25.00
Sample size
The sample size was 30 in each group Group I- pre-COVID 70 cases considered and Group II – post-COVID 30 cases considered). Using the sample size formula, with prevalence of 0.00019 with 3% margin of error, minimum number to conduct this study was too small, hence sample size of 30 considered.
An application for the study was submitted to the local Ethics Committee and approved.
Inclusion criteria
All elective primary THRs were included in the retrospective comparative study.
Exclusion criteria
All THRs of secondary to periprosthetic fractures, impending fractures secondary to malignant diseases, simultaneous THR on the contralateral side or simultaneous total knee replacement, same patient undergoing THR to the contralateral side (were not included more than once), complex operations not considered to be standard procedures were excluded from the study.
Statistical analysis
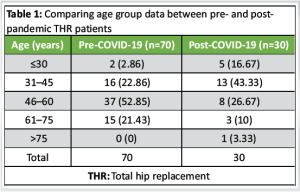
The data collected were entered into an excel sheet and analyzed using SPSS version 25.0. Qualitative variables were expressed as frequencies (percentages) and quantitative variables as mean ± standard deviation or median (interquartile range [IQR]). Our analysis shows that the number of patients requiring THA post-pandemic is more among the age group of 31–40 years; while pre-pandemic it is the age group of 46–60 contributing the highest (Table 1 and Fig. 1).
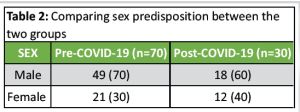
 We found that the ratio of male to female requiring THA pre-pandemic was 7:3, while post-pandemic it is 3:2, as there is a mild increase in females undergoing THA (Table 2 and Fig. 2).
We found that the ratio of male to female requiring THA pre-pandemic was 7:3, while post-pandemic it is 3:2, as there is a mild increase in females undergoing THA (Table 2 and Fig. 2).
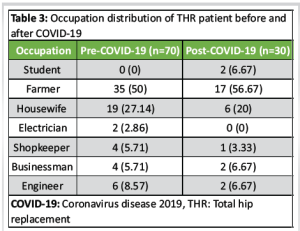
At our set-up it’s the farmer occupation that has undergone THA the maximum in both the groups (Table 3).
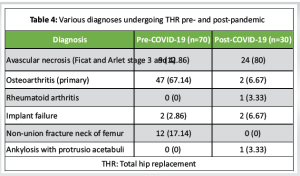
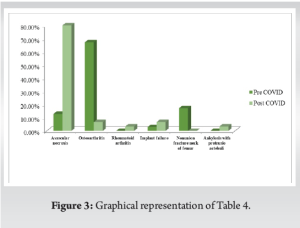
 With regards to the multiple diagnoses requiring THA, we have realized that it was primary osteoarthritis the maximum before the pandemic, whereas post-pandemic almost 80% were diagnosed to have femoral head AVN (FHAVN) (Table 4 and Fig. 3).
With regards to the multiple diagnoses requiring THA, we have realized that it was primary osteoarthritis the maximum before the pandemic, whereas post-pandemic almost 80% were diagnosed to have femoral head AVN (FHAVN) (Table 4 and Fig. 3).
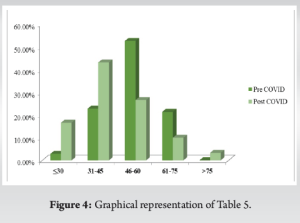
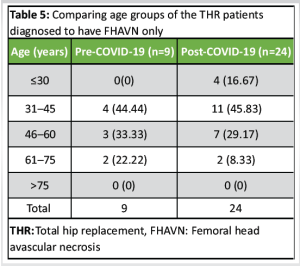
 While comparing the age groups of FHAVN patients requiring THA in either group, it has come to our notice that 31–45 years contribute the highest (Table 5 and Fig. 4).
While comparing the age groups of FHAVN patients requiring THA in either group, it has come to our notice that 31–45 years contribute the highest (Table 5 and Fig. 4).
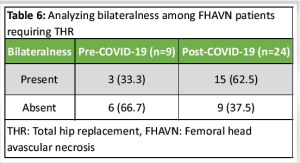
 On an attempt to analyze the bilateral presentation of FHAVN requiring THA, results show that it has drastically increased post-pandemic, such that the ratio has almost inversed (Table 6).
On an attempt to analyze the bilateral presentation of FHAVN requiring THA, results show that it has drastically increased post-pandemic, such that the ratio has almost inversed (Table 6).
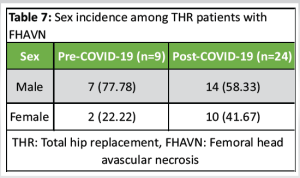
 Furthermore, there is an increment in females with FHAVN undergoing THA post-pandemic (Table 7).
Furthermore, there is an increment in females with FHAVN undergoing THA post-pandemic (Table 7).
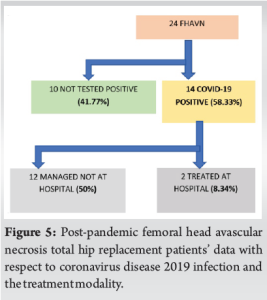
 Out of 24 patients in post-pandemic group, with Stage 3 and 4 FHAVN, 14 patients (58.33%) were tested COVID-19 positive, of which 2 patients (8.34%) were hospitalized and conservatively treated (further information not available), 12 patients (50%) had a history of medication as per physician advice, but whether it was corticosteroid, information was not available and 10 patients (41.66%) had no history of COVID-19 infection (Fig. 5).
Out of 24 patients in post-pandemic group, with Stage 3 and 4 FHAVN, 14 patients (58.33%) were tested COVID-19 positive, of which 2 patients (8.34%) were hospitalized and conservatively treated (further information not available), 12 patients (50%) had a history of medication as per physician advice, but whether it was corticosteroid, information was not available and 10 patients (41.66%) had no history of COVID-19 infection (Fig. 5).
 Following are the results of time duration of presentation (in months) among THR patients with FHAVN:
Following are the results of time duration of presentation (in months) among THR patients with FHAVN:
Pre-COVID: 42 (36, 48 IQR) months
Post-COVID: 6.5 (5.75, 12 IQR) months
Post-COVID infection: 6 months.
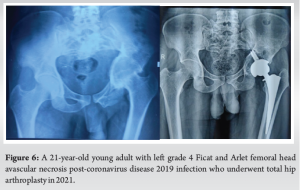
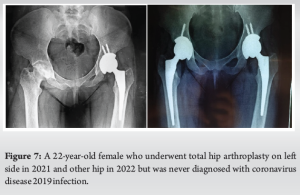
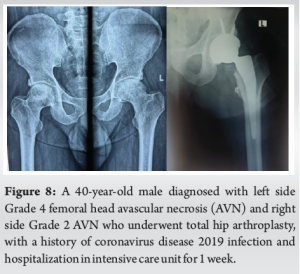
By which we have realized that post-pandemic FHAVN patients present to the hospital at late stages, much faster than before. On an attempt to study the association of corticosteroid intake with post-pandemic group specifically, we found that 12 patients who were managed by isolation and treatment at home, neither knew about medications nor did they have any substantiating documents at the time of the surgery. Even the two patients who were treated at the hospital apparently did not have any medical documents. Therefore, we could not analyze this association in any amount. Among 24 FHAVN patients in post-pandemic group, only five patients had a history of alcohol consumption and smoking, out of whom only two were tested positive for COVID-19 infection. Various instances were met during the investigation, and some examples have been illustrated here to offer an understanding of what and why we were inquisitive to perform this research (Fig. 6-8).
ONFH synonymously called FHAVN is a prevalent disabling illness that causes patients a severe pain. FHAVN is a multifactorial disease that has been mentioned in the literature for over a century and corticosteroids usage is a well-documented cause of this disease. The key pathological hallmarks of FHAVN include osteocyte death and bone marrow composition changes caused by arterial blood supply loss or interruption, as well as venous blood stasis. Femoral head collapse indicates a breakdown in the biomechanical qualities of subchondral bone, which eventually leads to dysfunction of the affected hip joint. That is when THA is the most reliable and last resort for restoring hip joint function, especially for Stages 3 and 4 of Ficat and Arlet classification [13-16]. While FHAVN is a poorly understood disease due to its complex nature, following the COVID-19 pandemic, there have been numerous reports and research indicating a possible relationship. Furthermore, during the pandemic, the World Health Organization approved the use of corticosteroids to suppress the inflammatory response in critical COVID-19-infected patients thus alarming an enhanced FHAVN risk in SARS-CoV-2-infected patients [17,18]. Most investigations have shown that COVID-19 infection, either directly or indirectly, is to blame for the well-known presentation of FHAVN leading to THR [16,19]. The following are plausible etiologies:
- Hypercoagulability (thromboembolism)
- Endothelial injury
- Complement pathway and mast cell activation
- Corticosteroid therapy.
Our research focuses on long-term COVID-related orthopedic problems, specifically ONFH. At our set-up, FHAVN as a diagnosis for THA has increased dramatically to 80% post-pandemic (roughly 6 folds more), from 12.86% pre-pandemic. We discovered that the age range of people presenting with late-stage FHAVN had shifted from 46-60 years pre-pandemic to 31-45 years post-pandemic. Between the two groups, there is an increase in patients under the age of 30 undergoing THA. Both before and after the pandemic, the 31–45 age group continues to contribute the most to FHAVN resulting to THR, which validates with another study done among north-Indian population [16]. Contrary to our study, Okewunmi et al. concluded that there is an increase in THA due to FHAVN in older population in USA [20]. In addition, where males were the more likely to present with this condition, there has been a surge in the number of females having THR for the same diagnosis. Males continue to be the most typically affected by FHAVN, both before and after the pandemic. Following the pandemic, the number of bilateral FHAVN requiring THA increased significantly in our study center. We found that 58.33% of FHAVN patients tested positive for COVID-19, with the majority receiving medical care outside of the hospital. The average duration of FHAVN presentation necessitating THR has decreased significantly to 6.5 months, which is almost 6-fold faster. Although smoking and alcohol intake are strongly associated with FHAVN, only handful of the post-pandemic population had such a history [21]. We tried to analyze the usage of corticosteroid, the well-known risk factor for FHAVN, but there were no documentations of the same to investigate [22,23]. It was only recorded if patients were anytime during the pandemic were tested positive for COVID-19 infection or not. Suggested by different authors the COVID-19 pandemic could be a multi-factorial cause of FHAVN, increasing the burden of THR. Dhanasekararaja et al. [24] studied 22 patients who developed femoral head osteonecrosis after receiving corticosteroids to treat COVID-19. According to Agarwala et al., osteonecrosis in COVID-19 occurred even with a lower dose of corticosteroid treatment [25]. Sulewski et al. concluded that COVID-19 infection alone may serve as a risk factor for femoral head osteonecrosis [5]. ONFH has the potential to be the most bothersome “long-COVID-19” not just for orthopedic surgeons but also for the general public, especially when in our setup it is the farmers (belonging to low socioeconomic status) who present the highest for THA due FHAVN [26,27].
This study strongly suggests that the COVID-19 pandemic as a whole increases the likelihood of developing femoral head osteonecrosis. Our findings also point to an accelerated presentation of FHAVN after the pandemic. COVID-19 infection leads to the necessity for THA much earlier than the other reported etiologies. We may witness an increase in the incidence of osteonecrosis as an indication for THA. The world may have succeeded in combatting COVID-19 virus, but not the sequalae. We must screen patients for FHAVN to reduce THR-related morbidity, among young working adults (requiring strenuous day-to-day activities) in particular.
Drawbacks
- Our study is a retrospective study, with a small sample size, hence falls short of analyzing various other confounders, such as doses of corticosteroid usage in the treatment.
- We suggest comprehensive studies to investigate further into the contributions of COVID-19 pandemic.
Even though FHAVN, particularly the idiopathic type, is common in our country, perhaps FHAVN had not plagued our system to the same extent as it does today. There is cause for concern as COVID-19 is either directly or indirectly contributing to the rise in cases. All patients with groin pain (ruling out most common pathologies) must be screened for FHAVN to identify them as soon as possible, retain functional natural joints and delay THR.
References
- 1.Hassan AA, Khalifa AA. Femoral head avascular necrosis in COVID-19 survivors: A systematic review. Rheumatol Int 2023;43:1583-95. [Google Scholar | PubMed]
- 2.Disser NP, De Micheli AJ, Schonk MM, Konnaris MA, Piacentini AN, Edon DL, et al. Musculoskeletal consequences of COVID-19. J Bone Joint Surg Am 2020;102:1197-204. [Google Scholar | PubMed]
- 3.Angulo-Ardoy M, Ureña-Aguilera Á. Knee osteonecrosis after COVID-19. Fam Pract 2021;38:i45-7. [Google Scholar | PubMed]
- 4.Ghosh S, Gupta SS, Mehta N, Khodaiji S. COVID-19-associated bone marrow necrosis-A case report. Indian J Radiol Imaging 2021;31:725-8. [Google Scholar | PubMed]
- 5.Sulewski A, Sieroń D, Szyluk K, Dąbrowski M, Kubaszewski Ł, Lukoszek D, et al. Avascular necrosis bone complication after active COVID-19 infection: Preliminary results. Medicina (Kaunas) 2021;57:1311. [Google Scholar | PubMed]
- 6.Baimukhamedov C, Botabekova A, Lessova Z, Abshenov B, Kurmanali N. Osteonecrosis amid the COVID-19 pandemic. Rheumatol Int 2023;43:1377-8. [Google Scholar | PubMed]
- 7.National Institute for Health and Care Excellence. COVID-19 Rapid Guideline: Managing the Long-term Effects of COVID-19; 2021. Available from: https://www.nice.org.uk/guidance/ng188 [Google Scholar | PubMed]
- 8.Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: A review. J R Soc Med 2021;114:428-42. [Google Scholar | PubMed]
- 9.Agarwala SR, Vijayvargiya M, Pandey P. Avascular necrosis as a part of ‘long COVID-19’. BMJ Case Rep 2021;14:e242101. [Google Scholar | PubMed]
- 10.Cho YJ, Nam DC, Jung K. Arthroplasty in femoral head osteonecrosis. Hip Pelvis 2014;26:65-73. [Google Scholar | PubMed]
- 11.Beaulé PE, Amstutz HC. Management of Ficat stage III and IV osteonecrosis of the hip. J Am Acad Orthop Surg 2004;12:96-105. [Google Scholar | PubMed]
- 12.Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD, et al. Osteonecrosis of the hip: Management in the 21st century. Instr Course Lect 2003;52:337-55. [Google Scholar | PubMed]
- 13.Wang P, Wang C, Meng H, Liu G, Li H, Gao J, et al. The role of structural deterioration and biomechanical changes of the necrotic lesion in collapse mechanism of osteonecrosis of the femoral head. Orthop Surg 2022;14:831-9. [Google Scholar | PubMed]
- 14.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 1995;77:459-74. [Google Scholar | PubMed]
- 15.Brinker MR, Rosenberg AG, Kull L, Galante JO. Primary total hip arthroplasty using noncemented porous-coated femoral components in patients with osteonecrosis of the femoral head. J Arthroplasty 1994;9:457-68. [Google Scholar | PubMed]
- 16.Goyal T, Singh A, Sharma R, Kundu Choudhury A, Arora S. Osteo-necrosis of femoral head in North Indian population: Risk factors and clinico-radiological correlation. Clin Epidemiol Global Health 2019;7:446-9. [Google Scholar | PubMed]
- 17.Sapra L, Saini C, Garg B, Gupta R, Verma B, Mishra PK, et al. Long-term implications of COVID-19 on bone health: Pathophysiology and therapeutics. Inflamm Res 2022;71:1025-40. [Google Scholar | PubMed]
- 18.Zhang S, Wang C, Shi L, Xue Q. Beware of steroid-induced avascular necrosis of the femoral head in the treatment of COVID-19-experience and lessons from the SARS epidemic. Drug Des Devel Ther 2021;15:983-95. [Google Scholar | PubMed]
- 19.Lykissas MG, Gelalis ID, Kostas-Agnantis IP, Vozonelos G, Korompilias AV. The role of hypercoagulability in the development of osteonecrosis of the femoral head. Orthop Rev (Pavia) 2012;4:e17. [Google Scholar | PubMed]
- 20.Okewunmi JO, Duey AH, Zubizarreta N, Kodali H, Poeran J, Hayden BL, et al. Did the COVID-19 pandemic coincide with an increase in osteonecrosis as indication for total hip arthroplasty in older patients? J Arthroplasty 2023;38:2634-7. [Google Scholar | PubMed]
- 21.Muthu S, Jeyaraman M, Selvaraj P, Jeyaraman N, Potty AG, Gupta A. Dose-response meta-analysis of corticosteroid effects in SARS outbreak: A model for risk stratification and screening strategy for osteonecrosis of femoral head post-corticosteroid therapy for COVID-19. Life (Basel) 2023;13:907. [Google Scholar | PubMed]
- 22.Veizi E, Erdoğan Y, Sezgin BS, Karaman Y, Kılıçarslan K, Fırat A. The painful joint after COVID-19 treatment: A study on joint osteonecrosis following COVID-19-related corticosteroid use. Jt Dis Relat Surg 2023;34:75-83. [Google Scholar | PubMed]
- 23.Kingma TJ, Hoch V, Johnson C, Chaudhry B. Avascular necrosis of the hip: A post COVID-19 sequela. Cureus 2022;14:e29976. [Google Scholar | PubMed]
- 24.Dhanasekararaja P, Soundarrajan D, Kumar KS, Pushpa BT, Rajkumar N, Rajasekaran S. Aggressive presentation and rapid progression of osteonecrosis of the femoral head after COVID-19. Indian J Orthop 2022;56:1259-67. [Google Scholar | PubMed]
- 25.Agarwala S, Vijayvargiya M, Sawant T, Kulkarni S. Bisphosphonates for Post-COVID osteonecrosis of the femoral head: Medical management of a surgical condition. JB JS Open Access 2022;7:e22.00060. [Google Scholar | PubMed]
- 26.Koutalos AA, Stefanou N, Malizos KN. Postacute sequelae of SARS-CoV-2 infection. Osteonecrosis must not be overlooked. Int J Infect Dis 2022;121:11-3. [Google Scholar | PubMed]
- 27.Jeyaraman M, Selvaraj P, Jeyaraman N, Gollahalli Shivashankar P, Muthu S. Assessment of risk factors in post- COVID-19 patients and its associated musculoskeletal manifestations: A cross-sectional study in India. J Orthop 2022;33:131-6. [Google Scholar | PubMed]









