Efficacy of using low-cost negative pressure dressing in sacral pressure injuries on wound management and functional recovery.
Dr. Arvind Kumar Sharma, Department of Physical Medicine and Rehabilitation, All India Institute of Medical Sciences, Raebareli, Uttar Pradesh, India. E-mail: draksusha2015@gmail.com
Introduction: Pressure injuries (PIs) continue to remain one of the most common and debilitating complications seen adding to the financial burden of the patients and caregivers. The available vacuum-assisted closure systems are expensive. In our case series, we have applied low-cost negative pressure dressing (NPD) for sacral PIs in five patients along with individualized rehabilitation protocol which resulted in accelerated healing of their PIs and improved functional outcome.
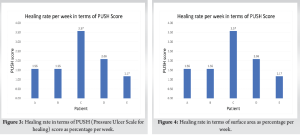
Materials and Methods: Five patients having PIs of Grade IV according to NPIAP classification in whom we applied NPD were included. Pressure ulcer scale for healing (PUSH), reduction of surface area of the wounds was recorded on a weekly basis. Functional independence measure (FIM) score of the patients was evaluated at admission and at discharge. Healing rate by means of PUSH score and surface area were recorded.
Results: Improvement in FIM score from the time of admission till at discharge was calculated to be 42.86% with a standard deviation of 16.84. Healing rate by means of PUSH score was the highest for Patient C at 3.57% per week and in terms of surface area for Patient C at 5.44% per week.
Conclusion: Low-cost negative pressure device has been observed to be a safe and effective method of managing PIs. It prevents further infection and helps to optimize and accelerate healing in PIs with the additional advantage of being cost-effective and easy to apply.
Keywords: Pressure injury, vacuum-assisted closure, low-cost negative pressure dressing, spinal cord injury, neurorehabilitation.
Pressure injury (PI) is defined as “localized damage to skin and underlying soft tissue, usually overlying a bony prominence or caused by contact with a medical device or another object, which develops due to intense and/or prolonged pressure or pressure combined with shearing.” It can present as intact skin or as open ulcers [1]. Despite recent advancements in the treatment of bedridden individuals, PIs continue to remain one of the most common and debilitating complications seen. PIs are mostly non-healing, adding to the financial burden of the patients and caregivers. Hence, economical methods are highly beneficial for the patient and their families. Vacuum-assisted closure (VAC)/negative pressure wound therapy (NPWT) is an alternative method for faster healing of chronic non-healing PIs. It is a wound dressing system that subjects the entire wound to sub-atmospheric pressure. It consists of a semi-occlusive adhesive cover, a system to collect fluid, and a suction pump. It involves application of negative pressure which causes increased tissue pressure and faster flowing of intravascular fluid thereby reducing the intravascular Hydrostatic pressure. This results in decreased edema at the site of the PI. In addition, it forces the edema away from the site of the injured tissues which improves oxygenation of the cells and thus enables faster healing [2]. NPWT impart a negative pressure of −60 to −125 mm Hg over the surface of the ulcer. Suction created enables removal of interstitial fluid, reduces edema, decreasing bacterial levels while increasing blood flow [3]. The available VAC systems are expensive and many affected individuals in developing countries find it difficult to afford. In our case series, we have applied low-cost negative pressure dressing (NPD) for sacral PIs in five patients along with individualized rehabilitation protocol which resulted in accelerated healing of their PIs and improved functional outcome.
In this study, five patients having PIs of Grade IV according to NPIAP classification were included [4]. All the patients included were admitted in the in-patient facility of Department of Physical Medicine and Rehabilitation (PMR) at All India Institute of Medical Sciences, Raebareli. Patients included were within the age group of 30–65 years. Patient information including history, physical examination, and necessary investigations were done. The wounds were optimized by daily cleaning and dressing under aseptic conditions, surgical debridement, and appropriate antibiotics were started according to culture reports from the wounds. Five patients having such PIs over the sacral region were treated with low-cost NPD applied under aseptic conditions. Pressure Ulcer scale for healing (PUSH) score was used to grade the severity of the PI based on area, tissue type, and exudate amount [5]. Reduction in surface area with time was also measured by simple ruler method where the maximum dimensions of length and width of the PI were assessed and recorded. Functional independence measure (FIM) scale was also recorded for all five patients [6]. All patients were also put on an individualized neurorehabilitation protocol aiming at improving functional recovery of the patients so that they could resume their activities of daily living.
NPD procedure
NPD application and all following dressing-related procedures were carried out in the operation theatre under aseptic conditions. The fenestrated portion of the fluid drain of the closed wound suction unit was placed on the bed of the ulcer and its free end was made to exit through the skin at a distance of 100 mm from the ulcer. The other end was fixed with a drain below. A piece of foam of wound size was sterilized and kept over the base of the ulcer. Adhesive airtight sterile dressing was placed over the ulcer. The closed wound suction unit is charged to attain appropriate negative pressure. Six hourly charging of the closed wound suction unit was done. It was kept for 1 week and was reapplied every week or earlier if the need arose [7]. The NPD application was done on an average thrice for each wound.
Out of the five patients included, all were of Grade IV according to NPIAP staging. About 75% of the patients were diagnosed with spinal cord injury (SCI) and one patient (25%) with traumatic brain injury due to polytrauma. About 75% of the patients were men and 25% were women. Table 1 shows the details of patient characteristics demographic details of the patients included in the case series. (Fig. 1, 2)
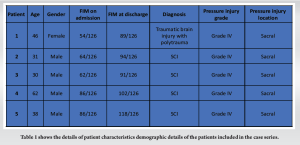
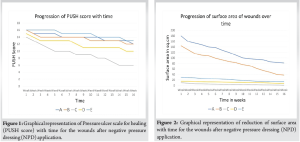
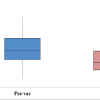
Mean improvement in FIM score from the time of admission till at discharge was calculated to be 42.86% with a standard deviation of 16.84. Healing rate by means of PUSH score was the highest for patient C at 3.57% per week and in terms of surface area for Patient C at 5.44% per week. Healing rate was calculated by using PUSH score and surface area on weekly basis which have been depicted graphically in Fig. 3 and 4.
One of the cases with TBI with polytrauma has been described
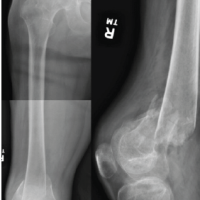
EW conservatively managed case left hemiplegia (Alleged history of head injury due to fall from height) with fracture pelvis with left distal radius fracture with healed Grade IV PI over sacrum with healing Grade II PI on posterior aspect of the left heel. A 46-year-old female patient was managed conservatively at a trauma center. Fig. 5 depicts her pelvis fracture X-ray showing fracture of bilateral superior and inferior pubic rami.

The left DER fracture was conservatively managed with plaster of Paris casts and was admitted under PMR for neurorehabilitation. Fig. 6 depicts the progression of the PI over the sacrum before and after NPD application. Patient was advised to get plastic surgery opinion, but due to financial constraints, the advice was not followed. Patient and caregiver were educated about postural care, cleaning, and dressing of the wound under aseptic precautions. Abdominal and trunk muscle strengthening, balance, and coordination exercises were taught to the patient. Therapeutic standing was initiated followed by gait training in parallel bars.
Case 2
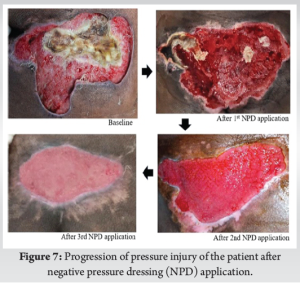
Seven-month-old elsewhere operated case of traumatic SCI (cause: Fall from height) with neurogenic bowel and bladder with Grade III PI over sacral region. Sensory level T10, motor level T10, NLI: T10. AIS Grade A. Dimensions of Grade III PIs over sacral region: 7 cm × 3 cm. Daily cleaning and dressing of the wounds were done under aseptic conditions. During the course of his hospitalization, 3 weeks post-admission, the patient developed a fall in blood pressure along with an increased respiratory rate. The condition of the patient was assessed and fluid resuscitation was started in the ward itself. There was no improvement in his BP despite fluid resuscitation, due to which inotropic drugs were started to maintain BP and to prevent multiple organ dysfunction syndrome. Renal function tests showed deranged electrolytes and raised creatinine. The patient was assessed and qSOFA was calculated as two. The patient was transferred to the intensive care unit (ICU) for further care and was diagnosed with septicemia with septic shock. He underwent PRBC transfusion in view of low Hb 7 g/dL. The patient was treated aggressively with fluid resuscitation, with strict input output monitoring, and inotropic noradrenaline. On day 3, inotrope support was weaned off, his condition improved and he was stable. Appropriate antibiotic medication was administered as per sensitivity reports after calculating creatinine clearance. After stabilization in ICU, he was then managed in the PMR ward during which renal and liver function tests normalized, total count decreased, and blood and urine cultures were sterile. NPD was applied over his sacral PI following which considerable improvement was noted which has been shown in Fig. 7. Standing with support in walking frame, strengthening exercises were taught to the patient. The patient was discharged with stable vitals, healthy PIs having granulation tissue, and a decreased surface area. Patient was given bilateral hip knee ankle foot orthosis for therapeutic standing and home-based neurorehabilitation program.
PIs can be non-healing and chronic posing a major challenge for functional recovery in patients. PIs commonly recur and are difficult to manage and prevent, thus affecting the overall well-being of the affected individual. In a developing nation, most patients present only when the PI is of Grade III or IV and is of considerable size [8]. Patients need to be educated about the maintenance of hygiene around the wound, perineal hygiene, and care of insensate limbs. Pressure offloading every half-hourly must be done while sitting on a wheelchair and every 2 h while on bed. Pressure-relieving mattresses and cushions should be utilized, and clothing and linens should be kept smooth to minimize shear stress [9]. All wounds in this study were found to have a positive culture and were treated with antibiotics according chosen as per sensitivity as infections in PIs are a major threat to cause in sepsis [10]. NPWT dressings can prove to be financially daunting for most individuals. Low-cost NPD is a user-friendly method of using negative pressure to drain out the secretions from the wound. It is cost-effective and specially designed to be used in a resource-constrained setting [8]. In this study, on average, NPD was applied for three consecutive weeks during their hospital stay, after which the patient was followed up on outpatient department basis. There were no episodes of fever or any complications such as deterioration of the ulcer or infection at the site of the PI. Decreased size with of regeneration of tissue type, appearance of healthy granulation tissue, and reduced amount of exudate was noted, resulting in an overall reduction of PUSH score. The NPD covered the wound in such a way that it ensured asepsis, prevention of infection and kept the wound moist while ensuring that excessive exudate was drained out. On follow-up, healthy margins were seen to be approximating and epithelialization of the wounds was observed. Management of PIs requires a comprehensive approach covering physical, personal, and environmental aspects of the patient. Wound management along with early initiation of rehabilitation has shown to bring improvement in functional recovery for the patient. In addition, functional independence for carrying out routine tasks and reduces the burden and strain on the caregiver. Patients find it difficult to access super-specialties, such as plastic surgery, for wound management and face a long waiting time for surgical interventions. Thus, low-cost NPD is a more feasible option for economical wound healing at a faster rate.
Low-cost negative pressure device has been observed to be a safe and effective method of managing PIs. It prevents further infection and helps to optimize and accelerate healing in PIs with the additional advantage of being cost-effective and easy to apply. Surgical interventions such as tissue graft and flaps lead to additional weakness due to muscle transfer from other areas or the patient may have an insensate limb resulting in an increased chance of breakdown of the skin integrity. In addition due to increased tone, there is an increase of tangential forces over the grafted skin resulting in failure of surgical procedure or reoccurrence of PIs. Hence, surgical option of wound may not be feasible for such patients. It ensures compliance from the end of the patient and their attendants and helps to improve their functional outcome and progress in neurorehabilitation.
The management of chronic non-healing pressure ulcers presents a complex challenge that requires a comprehensive, multidisciplinary approach. This approach should extend beyond the wound itself to address the individual as a whole, considering biological, psychological, and social factors that influence healing.
In the rehabilitation of patients with pressure ulcers, rehabilitation physicians must carefully evaluate cost-effective strategies for prevention and treatment. Low-cost negative pressure dressings have demonstrated accelerated healing of sacral pressure ulcers. As an adjunctive therapy, these dressings can help optimize the healing environment and promote better outcomes.
By enhancing the healing process, negative pressure therapy can improve a patient’s quality of life and functional recovery. This approach provides a valuable tool in the comprehensive management of chronic pressure ulcers, offering both clinical and economic benefits for patients and healthcare systems alike.
References
- 1.Andrews KL, Derby KM, Jacobson TM, Sievers BA, Kiemele LJ. Prevention and management of chronic wounds. In: Cifu DX, editor. Braddoms Textbook of Physical Medicine and Rehabilitation. 6th ed. Philadelphia, PA: Elsevier; 2021. p. 474. [Google Scholar | PubMed]
- 2.Normandin S, Safran T, Winocour S, Chu CK, Vorstenbosch J, Murphy AM, et al. Negative pressure wound therapy: Mechanism of action and clinical applications. Semin Plast Surg 2021;35:164-70. [Google Scholar | PubMed]
- 3.Plikaitis CM, Molnar JA. Subatmospheric pressure wound therapy and the vacuum-assisted closure device: Basic science and current clinical successes. Expert Rev Med Devices 2006;3:175-84. [Google Scholar | PubMed]
- 4.National Pressure Ulcer Advisory Panel. Pressure Ulcer Stages Revised by NPUAP; 2016. Available from: https://www.npuap.org/resources/educational-and-clinical-resources/pressure-injury-staging-illustrations [Last accessed on 2016 Jun 01]. [Google Scholar | PubMed]
- 5.Stotts NA, Rodeheaver GT, Thomas DR, Frantz RA, Bartolucci AA, Sussman C, et al. An instrument to measure healing in pressure ulcers: Development and validation of the Pressure Ulcer Scale for Healing (PUSH). J Gerontol A Biol Sci Med Sci 2001;56:M795-9. [Google Scholar | PubMed]
- 6.Yang W, Houtrow A, Cull DS, Annaswamy TM. Quality and outcome measures for medical rehabilitation. In: Cifu DX, editor. Braddoms Textbook of Physical Medicine and Rehabilitation. 6th ed. Philadelphia, PA: Elsevier; 2021. p. 104. [Google Scholar | PubMed]
- 7.Dwivedi MK, Bhagat A, Srivastava RN, Raj L. Management of grade IV pressure ulcers with a novel negative pressure device in traumatic paraplegia subjects. Cureus 2020;12:e9327. [Google Scholar | PubMed]
- 8.Srivastava RN, Dwivedi MK, Bhagat AK, Raj S, Agarwal R, Chandra A. A non-randomised, controlled clinical trial of an innovative device for negative pressure wound therapy of pressure ulcers in traumatic paraplegia patients. Int Wound J 2016;13:343-8. [Google Scholar | PubMed]
- 9.Martin M, Wuermser LA, Priebe MM, Castillo T, McFarlin J. Medical management of pressure ulcers. In: Lin VW, editor. Spinal Cord Medicine Principles and Practice. New York: Demos; 2021. p. 574-79. [Google Scholar | PubMed]
- 10.Kaya PK, Kaya M, Girgin NK, Kahveci FŞ, Akalın EH, İşçimen R. Sepsis episodes caused by pressure injuries in critical illness: A retrospective observational cohort study. Wound Manag Prev 2023;69:4-9. [Google Scholar | PubMed]