Thorough evaluation of the elbow joint, along with careful reading and knowledge of plain radiography, would not have allowed us to miss the diagnosis of elbow dislocation or subluxation, even of a subtle nature. The importance of correct radiological views and landmarks of the elbow joint has been highlighted in this case report.
Dr. Asad Khan, Department of Orthopaedic Surgery, Faculty of Medicine, J. N. Medical College, AMU, Aligarh - 202 002, Uttar Pradesh, India. E-mail: khanasad53@gmail.com
Introduction: Chronic elbow dislocation is a profoundly debilitating condition characterized by severe instability, limited elbow function, and significant pain. The term “neglected dislocation of the elbow” refers to a traumatic elbow dislocation that has gone untreated for three weeks or longer. Successfully treating this condition presents a challenge, as it involves restoring elbow stability and achieving a decent range of motion, which can be particularly complex.
Case Report: We present a case involving a 34-year-old male patient who experienced a complex dislocation of his right elbow joint. Initial diagnosis at our emergency department missed the elbow dislocation, but a follow-up visit three weeks later revealed the true extent of the injury. Fortunately, successful closed reduction resulted in the patient regaining full range of motion, with a Mayo Elbow Performance Score of 90.
Conclusion: This case report serves to underscore the essential nature of accurate diagnosis and treatment of elbow dislocations, both clinically and radiologically, to prevent future complications.
Keywords: Elbow dislocation, missed, complex, subtle.
The elbow joint ranks as the second most frequently dislocated joint in adults, following the shoulder. Each year, approximately 6.1 dislocations involving the elbow joint occur per 100,000 individuals [1]. Elbow dislocations are categorized into two types – simple and complex [2]. A simple dislocation lacks fractures, while a complex dislocation manifests as intra-articular fractures of the radial head or neck, distal humerus, and coronoid process. Neglected dislocations occur when the elbow joint remains dislocated for three weeks or longer without medical attention [3]. In underdeveloped and some developing nations, these presentations are more common, often due to factors such as low literacy rates, low socioeconomic status, delayed treatment, and a shortage of accessible specialized medical services [4]. If an elbow dislocation remains unreduced, there is a potential for rapid onset of arthritic changes [5]. The primary therapeutic goals, which involve achieving a stable, concentric joint and restoring a satisfactory arc of motion, may initially appear conflicting. Consequently, the successful management of chronic elbow dislocations presents a significant clinical challenge.
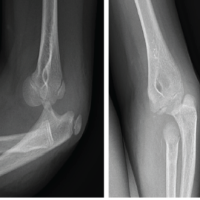
A 34-year-old male sustained a right elbow injury with significant pain and diminished range of motion subsequent to a fall on stairs. He later presented to the emergency and trauma centre of our hospital. Initial assessment revealed no signs of neurovascular compromise in the affected limb. Clinical examination revealed tenderness and edema around the right elbow joint without apparent deformity. The elbow demonstrated restricted motion, with discomfort beyond a range of 30° to 90°. An initial radiographic evaluation (Fig. 1) indicated a radial head fracture, notwithstanding the regrettable oversight of the diagnosis of elbow dislocation. In light of the prevailing COVID-19 circumstances, a conservative management strategy was pursued, entailing the application of an above-elbow plaster cast for a duration of 3 weeks. A subsequent radiographic examination at the 3-week follow-up identified a “subtle” posterior elbow subluxation in addition to the radial head fracture (Fig. 2). Consequently, the decision was made to arrange for the patient’s admission for elbow reduction, aiming to preserve joint function.

Our Management
The medical team initially endeavoured closed reduction without anaesthesia, albeit without success, despite administering analgesics. Subsequently, a second closed reduction attempt was undertaken with success in the operating room under general anaesthesia and muscle relaxants. The patient demonstrated the stability of the elbow joint throughout the full range of motion assessment without any discernible limitations in mobility. During the reduction maneuver, the patient was positioned in a supine posture, allowing for the arm to hang by the side of the table. Deliberate downward pressure was exerted on the olecranon, concomitantly with distal traction on the wrist to effectuate the reduction of the elbow joint. Subsequently, a smooth K-wire was utilized to transfix the ulna-humeral joint, coupled with the application of an extended forearm slab to facilitate soft-tissue convalescence (Fig. 3). The decision was formulated to abstain from addressing the radial head fracture in contemplation of potential compromise to joint stability stemming from further soft tissue disruption. Furthermore, post reduction, the radial head fracture was found to be in an acceptable position. The subsequent removal of the K-wire after a duration of 3 weeks paved the way for the initiation of active and active-assisted elbow mobilization exercises. Following a 3-week interval of intensive physiotherapy, the patient attained comprehensive restoration of elbow motion with concomitant alleviation of nociceptive manifestations. Fig. 4 depicts follow-up radiographic evaluations conducted 1-year post-K-wire extraction, complemented by clinical illustrations in Fig. 5, thereby substantiating associated clinical outcomes.


Clinical and radiological parameters
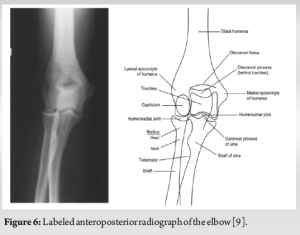
It has been noted that in cases where the active range of motion, encompassing flexion, extension, pronation, and supination, remains within acceptable normal limits, there may exist a lack of necessity for radiologic imaging investigations to ascertain elbow fractures and dislocations [6] In accordance with alternative clinical prediction criteria espoused by Arundel et al., the absence of bruising, normal complete elbow extension, and the lack of soreness over specific anatomical landmarks within the elbow region serve to exclude the presence of a fracture in an adult, thereby obviating the need for imaging [7]. However, in our patient, the active range of motion elicited discomfort, and also, due to restricted full elbow extension, obtaining a radiological image became imperative. Noteworthy is the assertion by Arundel et al. that while clinical gestalt displays sensitivity in diagnosing fractures, applying a clinical prediction rule amplifies specificity (identifying which persons do not require imaging), thereby reducing the number of negative radiographs required [8]. The identification of most acute elbow dislocations encountered in an emergency setting is viably achievable through standard radiographic examinations. The customary minimal radiography series is known to encompass anteroposterior (AP), and lateral images, and it is worth considering that an oblique radial head-capitellar view contributes to the revelation of minute fractures by diminishing osseous overlap of the radial head and coronoid. In the AP view, it is crucial to confirm that the elbow is fully extended and the forearm is placed in a supinated position. This will allow for the best possible view of the lateral and medial epicondyles, the radiocapitellar joint, and makes it easier to measure the carrying angle [9] (Fig. 6).
The anterior humeral line refers to a line traced along the anterior cortex of the distal humerus in plain radiography. It is identified as intersecting the middle third of the capitellum in a lateral view, as demonstrated in Fig. 7 [10] (Table 1).
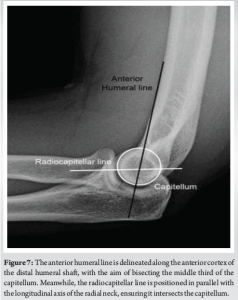
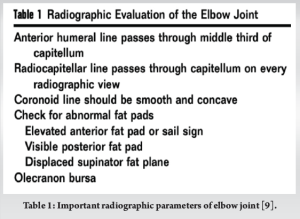
In the case of our patient, the radiocapitellar line appeared intact in the anteroposterior view of the initial x-rays, but was not maintained in the lateral views. This discrepancy may be attributed to the possible absence of properly executed true lateral x-rays. Therefore, obtaining precise anteroposterior and lateral views is imperative. Furthermore, in the AP view, there was an overlap of the radial head and capitellum, obscuring the normal humeroradial joint space.
Treatment protocol
In regions with limited access to advanced medical care, elbow dislocations are often treated by traditional bonesetters rather than skilled medical professionals. When an elbow dislocation occurs within three weeks of an injury, most surgeons recommend closed reduction. After 3 weeks, closed reduction becomes more challenging due to tissue contractures and localized osteoporosis, increasing the risk of bone fractures or joint damage during manipulation [11]. Treatment options include closed reduction, open reduction with internal fixation using K-wire, triceps lengthening with the release of the collateral ligament, creation of an intra-articular “cruciate” ligament to stabilize the joint, hinged external fixation, excisional arthroplasty, arthrodesis, and total elbow arthroplasty. Experts typically recommend total elbow arthroplasty, excisional arthroplasty, or arthrodesis for elbow dislocations occurring after three months [12]. In this specific case, the patient’s elbow dislocation was close to the 3-week mark, prompting an attempt at closed reduction to avoid potential complications associated with open reduction. The radial head fracture was managed through conservative methods.
This case report involves the discussion of a 3-week-old case with a subtle and complex posterior elbow dislocation. It underscores the crucial importance of promptly diagnosing and managing elbow dislocations to avoid complications that could compromise the functionality of the elbow. It also emphasizes the significance of obtaining proper X-ray views and conducting a thorough clinical examination and aims to highlight the necessity of these measures. It is highlighted that the effective and stable reduction of the elbow joint can be achieved within 3 weeks of the injury, as observed in the specific case presented. The report notes that as a result of the treatment, the patient was able to regain an excellent range of motion and obtain a stable elbow joint, resulting in a Mayo elbow performance score of 90.
Thorough evaluation of the elbow joint, along with careful reading and knowledge of plain radiography, would not have allowed us to miss the diagnosis of elbow dislocation or subluxation, even of a subtle nature. The importance of correct radiological views and landmarks of the elbow joint has been highlighted in this case report.
References
- 1.Josefsson PO, Nilsson BE. Incidence of elbow dislocation. Acta Orthop Scand 1986;57:537-8. [Google Scholar | PubMed]
- 2.Hildebrand KA, Patterson SD, King GJ. Acute elbow dislocations: Simple and complex. Orthop Clin North Am 1999;30:63-79. [Google Scholar | PubMed]
- 3.Krishnamoorthy S, Bose K, Wong KP. Treatment of old unreduced dislocation of the elbow. Injury 1976;8:39-42. [Google Scholar | PubMed]
- 4.Coulibaly NF, Tiemdjo H, Sane AD, Sarr YF, Ndiaye A, Seye S. Posterior approach for surgical treatment of neglected elbow dislocation. Orthop Traumatol Surg Res 2012;98:552-8. [Google Scholar | PubMed]
- 5.Jupiter JB, Ring D. Treatment of unreduced elbow dislocations with hinged external fixation. J Bone Joint Surg Am 2002;84-A:1630-5. [Google Scholar | PubMed]
- 6.Lennon RI, Riyat MS, Hilliam R, Anathkrishnan G, Alderson G. Can a normal range of elbow movement predict a normal elbow x ray? Emerg Med J 2007;24:86-8. [Google Scholar | PubMed]
- 7.Arundel D, Williams P, Townend W. Deriving the East riding elbow rule (ER2): A maximally sensitive decision tool for elbow injury. Emerg Med J 2014;31:380-3. [Google Scholar | PubMed]
- 8.Greenspan A, Norman A. Radial head-capitellum view: An expanded imaging approach to elbow injury. Radiology 1987;164:272-4. [Google Scholar | PubMed]
- 9.McKinnis LN. Fundamentals of Musculoskeletal Imaging. United States: FA Davis; 2013. [Google Scholar | PubMed]
- 10.Nagaraj G, Mitchelson JP, Mcfarland CM, Silver MA. Image diagnosis: Capitellar fracture. Perm J 2016;20:84. [Google Scholar | PubMed]
- 11.Naidoo KS. Unreduced posterior dislocations of the elbow. J Bone Joint Surg Br 1982;64:603-6. [Google Scholar | PubMed]
- 12.Freeman BL III. Old unreduced dislocations. In: Crenshaw AH, editor. Campbell’s Operative Orthopaedics. 9th ed. St. Louis: Mosby; 1998. p. 2673-4. [Google Scholar | PubMed]