An arthroscopic bursectomy is effective in recalcitrant snapping scapula syndrome.
Dr. Jojin Jose Chitten, Department of Orthopaedics, Al Azhar Medical College and Superspeciality Hospital, Thodupuzha, Kerala, India. E-mail: jojinjosec@gmail.com
Introduction: Snapping scapula syndrome (SSS) is a rare pathological condition characterized by palpable and/or audible crackling sensation during scapulothoracic movements. Scapulothoracic bursitis with or without osseous lesions is commonly associated with this syndrome. The initial management is always non-operative methods with anti-inflammatory medications and physiotherapy modalities. However, if the symptoms persist beyond 3–6 months of non-surgical treatment, it should be categorized as refractory or recalcitrant bursitis and necessitate either open or arthroscopic surgical excision of the lesion.
Case Report: We successfully managed five patients with SSS with arthroscopic scapulothoracic bursectomy.
Conclusion: Arthroscopic scapulothoracic bursectomy is a successful surgical intervention for patients with scapulothoracic bursitis who do not respond to the conservative mode of management.
Keywords: Scapula dyskinesia, scapulothoracic bursitis, snapping scapula syndrome
Snapping scapula syndrome (SSS) manifests as audible or palpable clicking of the scapula during movements of the scapulothoracic joint which can be associated with pain on rare occasions. It is an underdiagnosed and hence probably an under-reported condition [1]. The alignment and correct movement of the scapula are essential for the proper functioning of the glenohumeral joint. The scapulothoracic joint lacks true synovial articulation and is controlled by the dynamic periscapular muscles. The scapula glides on the posterior thorax covered with muscle layers which are facilitated by the infraserratus, subserratus, and trapezoid bursae [2]. The underlying pathology of SSS may be due to abnormalities of the muscular, bursal, and/or bony lesions around the scapula, and among these, the former two are the most common [3]. These can also lead to scapula dyskinesia. Scapular dyskinesia can be the cause or consequence of many forms of shoulder pain and dysfunction. It leads to alterations in the static scapular position and loss of dynamic control of scapular motion which can lead to an increase in anterior tilt and internal rotation and a decrease in scapular upward rotation. The anteriorly tilted scapula can compress the medial border against the ribcage and can lead to scapulothoracic bursitis which can result in persistent scapula dyskinesia [4]. SSS can also occur in patients with anatomical variations of scapula involving superomedial angle of scapula, retroscapular exostoses, Luschka’s tubercle, or Sprengel deformities [5, 6]. We present a case series of SSS which were treated arthroscopically after failed conservative management.
We had five patients who were diagnosed with SSS, out of which four were young male in the age group of 20–30 years, and one was a female who was 55 years old. Four of them had scapulothoracic bursitis and one had Lushka tubercle as the etiology. Two of them were swimmers, two were manual laborers, and one was a homemaker. On clinical examination, all the patients in the study demonstrated palpable and audible clicking sounds during scapulothoracic movements on the affected side (Fig. 1). None of them had any intra-articular pathology of the glenohumeral joint. Magnetic resonance imaging (MRI) revealed fibrous bands, thickened bursae, and ruled out any malignant conditions that may mimic scapulothoracic bursitis (Fig. 2). We performed MRI with contrast targeting the scapula, as routine shoulder MRI typically does not include the entire scapula with its medial border. T1- and T2-weighted fat-saturated sequences were performed in the coronal, sagittal, and axial planes of the scapula.

All the patients were initially treated with non-steroidal inflammatory oral medications, local ultrasound therapy, and short-wave diathermy along with scapula mobilization and periscapular muscle strengthening particularly focussing on scapular retractors. However, they were unresponsive to the treatment and hence planned for arthroscopy.
They were operated arthroscopically with scapulothoracic bursoscopy and bursectomy of both infraserrator and supraserratorbursae. The patient with an osseous lesion required additional superomedial resection of the scapula.
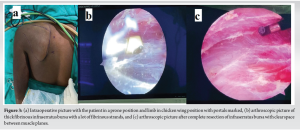
During the surgery, the patients were placed in a prone position with their arm in chicken winged position, two portals were made 3 cm medial to medial border of scapula, one just below the level of spine of scapula for arthroscope and one 5 cm below to that for the instrumentation (Fig 2). The bursoscopy revealed thick, inflamed bursae which were fibrotic with a lot of adherent fibrotic brands. Using a radiofrequency ablator and arthroscopic shaver, inflamed bursae were resected, and the scapula was freed from the thoracic wall regaining the full passive scapulothoracic motion (Fig. 3-6).


Postoperatively patients were given a broad arm sling for 2 weeks. Rehabilitation began on the 1st post-operative day. The passive exercises were initiated initially then escalated to active range of motion exercises at 1 week, followed by strengthening exercises by the end of the 1st month. The physiotherapy mainly focussed on restoring scapular kinematics and strengthening parascapular muscles.
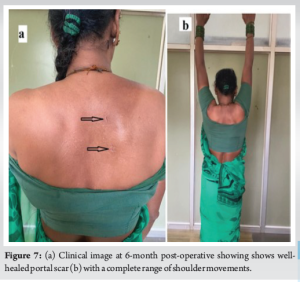
All the patients were followed up postoperatively till 1 year and at the end of 1 year, all the patients had a constant score above 90 and were completely relieved of snapping around the scapula having full pain-free movements at the shoulder and scapulothoracic joints (Fig. 4 and 7).
Many causes have been attributed to SSS, one of which being repetitive above-shoulder movement activities, which result in microtraumas and local bursitis that can generate a bony spur at the level of muscle attachment on the scapula [7]. In severe cases of SSS, this constellation of pathologies may result in SICK scapula (scapular malposition, inferomedial prominence of scapula, coracoid tenderness, and scapular dyskinesia) [8]. Management of SSS starts with a trial of conservative treatment. Rehabilitation includes stretching and manipulation of spastic muscles around the scapula which includes pectoralis minor and major, levator scapulae, upper trapezius, latissimus dorsi, sternocleidomastoid, rectus capitis, and scalene muscles. In addition, muscles which are wasted must be strengthened which includes rhomboids, mid and lower trapezius, serratus anterior, teres minor, infraspinatus, posterior deltoid, and longus colli or longus capitis. A trial of corticosteroid injections too can be given if it is secondary to symptomatic scapulothoracic bursitis [9]. In case of failed non-operative management for 3–6 months, surgical treatment is a viable option in symptomatic scapulothoracic bursitis. Surgical options include open or arthroscopic scapulothoracic bursectomy with or without resection of the superomedial angle of the scapula. Arthroscopic release of pectoralis minor too has definitive role in cases of scapular dyskinesia resulting from tight pectoralis minor and weak serratus anterior [10]. However, in our case, there was no pectoralis minor tightness as evidenced by the absence of coracoid tenderness, and therefore, pectoralis minor release was not necessary. Open approaches are comparatively invasive and involve splitting the trapezoid muscle while preserving the spinal accessory and dorsal scapular nerves, allowing the rhomboid and levator scapulae to be elevated and bursal tissue removed. This requires post-operative immobilization in a shoulder sling for at least 4 weeks to facilitate muscle healing. Active motion can be reached in 8 weeks [11]. Arthroscopic techniques have gained popularity due to its less invasive approach and faster recovery compared to the open technique. The main advantage of the arthroscopic procedure is that it preserves the muscle attachments, thereby eliminating the need for immobilization in the post-operative period and having a shorter rehabilitation period. There are few case series, reviews, and clinical studies which have proved these advantages of arthroscopic scapular debridement and resection with significant functional improvements in the majority of the patients [12-14]. Since the first description of arthroscopic bursectomy with partial scapulectomy for SSS in 1999 by Harper et al., there have been limited outcome studies [15]. Several authors have reported satisfactory outcomes after arthroscopic treatment for SSS. In a study, Merolla et al. evaluated 10 patients who were treated with arthroscopic surgery after having failed non-operative therapy and found that all post-operative scores had significantly improved compared with pre-operative scores [16]. Pearse et al. reported good outcomes in pain and function in nine patients out of 13 patients who underwent arthroscopic bursectomy [13]. Pavlik et al. reported the outcomes of 10 patients in whom the superior portal was used for resection of the superomedial corner of the scapula. The patients were followed up for an average of 11.5 months (range, 3–23 months). Scapulothoracic crepitus resolved in two patients and decreased in 8 [17]. There was a reduction in pain in all cases, and all patients reported that the procedure was worthwhile. Although our study has a lesser number of patients, the results of our study show consistency with these findings. In addition, Nicholson and Duckworth and Lethinen et al. pointed out that bony resection of the superomedial corner of the scapula may not always be necessary for the treatment of painful SSS and that a bursectomy alone can give satisfactory results to selected patients [18]. On the technical side, access to the superomedial corner of the scapulothoracic space is simple and reproducible. It is most easily accomplished by working through two superiorly based portals. Full internal rotation of the affected extremity through the chicken-wing position is important to lift the scapula up from the chest wall which creates a potential workspace. The important bony landmarks, identified with palpation, are the superomedial angle and scapular spine. Furthermore, the general trend of recent studies seems to be moving toward early detection and early intervention with either non-operative techniques or arthroscopic surgery, as an increased delay in treatment and increased age are associated with poorer outcomes [19, 20]. Hence, early pre-operative imaging is necessary to detect these lesions and the appropriate treatment should be initiated as early as possible.
Arthroscopic bursoscopy and bursectomy is an effective surgical procedure in recalcitrant scapulothoracic bursitis with failed conservative management.
Arthroscopic scapulothoracic bursectomy should be advised for patients with recalcitrant SSS.
References
- 1.Tashjian RZ, Shin J, Broschinsky K. Minimal clinically important differences in the American shoulder and elbow surgeons, simple shoulder test, and visual analog scale pain scores after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 2020;29:1406-11. [Google Scholar]
- 2.Kuhn JE, Plancher KD, Hawkins RJ. Symptomatic scapulothoracic crepitus and bursitis. J Am Acad Orthop Surg 1998;6:267-73. [Google Scholar]
- 3.Spiegl UJ, Petri M, Smith SW, Ho CP, Millett PJ. Association between scapula bony morphology and snapping scapula syndrome. J Shoulder Elbow Surg 2015;24:1289-95. [Google Scholar]
- 4.Blønd L, Rechter S. Arthroscopic treatment for snapping scapula: A prospective case series. Eur J Orthop Surg Traumatol 2013;24:159-64. [Google Scholar]
- 5.Gaskill T, Millett JP. Snapping scapula syndrome: Diagnosis and management. J Am Acad Orthop Surg 2013;21:214-24. [Google Scholar]
- 6.Nascimento AT, Claudio GK. Snapping scapula. Arthroscopic resection of osteochondroma of the subscapularis superomedial angle. Case report and literature review. Rev Bras Orthop 2017;52:220-3. [Google Scholar]
- 7.De Carvalho SC, Castro AD, Rodrigues JC, Cerqueira WS, Santos DD, Rosemberg LA. Snapping scapula syndrome: Pictorial essay. Radiol Bras 2019;52:262-7. [Google Scholar]
- 8.Carbone S, Postacchini R, Gumina S. Scapular dyskinesis and SICK syndrome in patients with a chronic type III acromioclavicular dislocation. Results of rehabilitation. Knee Surg Sports Traumatol Arthrosc 2015;23:1473-80. [Google Scholar]
- 9.Conduah AH, Baker CL 3rd, Baker CL Jr. Clinical management of scapulothoracic bursitis and the snapping scapula. Sports Health 2010;2:147-55. [Google Scholar]
- 10.Elhassan BT, Dang KH, Huynh TM, Harstad C, Best MJ. Outcome of arthroscopic pectoralis minor release and scapulopexy for the management of scapulothoracic abnormal motion. J Shoulder Elbow Surg 2022;31:1208-14. [Google Scholar]
- 11.Manske RC, Reiman MP, Stovak ML. Nonoperative and operative management of snapping scapula. Am J Sports Med 2004;32:1554-65. [Google Scholar]
- 12.Lien SB, Shen PH, Lee CH, Lin LC. Effect of endoscopic bursectomy with mini-open partial scapulectomy on snapping scapula syndrome. J Surg Res 2008;150:236-42. [Google Scholar]
- 13.Pearse EO, Bruguera J, Massoud SN, Sforza G, Copeland SA, Levy O. Arthroscopic management of the painful snapping scapula. Arthroscopy 2006;22:755-61. [Google Scholar]
- 14.Bell SN, van Riet RP. Safe zone for arthroscopic resection of the superomedial scapular border in the treatment of snapping scapula syndrome. J Shoulder Elbow Surg 2008;17:647-9. [Google Scholar]
- 15.Harper GD, McIlroy S, Bayley JI, Calvert PT. Arthroscopic partial resection of the scapula for snapping scapula: A new technique. J Shoulder Elbow Surg 1999;8:53-7. [Google Scholar]
- 16.Merolla G, Cerciello S, Paladini P, Porcellini G. Snapping scapula syndrome: Current concepts review in conservative and surgical treatment. Muscles Ligaments Tendons J 2013;3:80-90. [Google Scholar]
- 17.Baldawi H, Gouveia K, Gohal C, Almana L, Paul R, Alolabi B, et al. Diagnosis and treatment of snapping scapula syndrome: A scoping review. Sports Health 2022;14:389-96. [Google Scholar]
- 18.Nicholson GP, Duckworth MA. Scapulothoracic bursectomy for snapping scapula syndrome. J Shoulder Elbow Surg 2002;11:80-5. [Google Scholar]
- 19.Lazar MA, Kwon YW, Rokito AS. Snapping scapula syndrome. J Bone Joint Surg Am 2009;91:2251-62. [Google Scholar]
- 20.Menge TJ, Horan MP, Tahal DS, Mitchell JJ, Katthagen JC, Millett PJ. Arthroscopic treatment of snapping scapula syndrome: Outcomes at minimum of 2 years. Arthroscopy 2017;33:726-32. [Google Scholar]