Atlantoaxial instability is a significant and potentially severe complication in individuals with neurofibromatosis type 1. Early recognition and evaluation are crucial to address this condition effectively
Dr Sankalp Lal, Department of Orthopaedics, Dr SN Medical College, Jodhpur, Rajasthan, India. E-mail: sankalp26@live.com
Introduction: Neurofibromatosis (NF) is a cluster of conditions in which tumors grow in the nervous system. Even though the spine is the most common site of skeletal involvement in NF type 1 (NF-1), cervical spinal anomalies are infrequent.
Case Report: The atlantoaxial joint is a critical transitional zone in the cervical spine and is prone to instability. We report the case of a 49-year-old gentleman with atlantoaxial instability due to NF-1 who presented with quadriparesis and was managed by reduction with skull traction followed by C1-C2 Goel-Harms fixation.
Conclusion: In the present case, there was substantial bleeding and significant vertebral dysplasia, which makes the case distinctly unique. Skull traction and C1-C2 Goel-Harms fixation with fusion should be considered for patients with NF-1 complicated by atlantoaxial instability.
Keywords: Atlantoaxial instability, neurofibromatosis, Goel-Harms technique.
Neurofibromatosis (NF) is a cluster of conditions in which tumours grow in the nervous system. Two distinct forms of NF have been reported. NF type 1 (NF-1) is referred to as peripheral NF, whereas NF type 2 is referred to as central NF. NF-1 is an autosomal dominant disorder typically presenting with café-au-lait spots, neurofibroma, and bony anomalies [1]. Even though the spine is the most common site of skeletal involvement in NF-1, cervical spinal anomalies are infrequent [2]. The atlantoaxial joint is an important transitional zone in the cervical spine and is prone to instability. Atlantodens interval (ADI) refers to the distance between the odontoid process and the posterior border of the anterior arch of the atlas. >3 mm is considered unstable; surgery is indicated when it is >5 mm. The instability is generally congenital but can also be due to an acute traumatic event or degenerative disease. Atlantoaxial instability in NF-1 is extremely rare, with only a handful of case reports available in the literature [3-5]. Atlantoaxial instability in NF-1 is speculated to be due to mesodermal dysplasia ± presence of NF tissue anterior to the odontoid process [6]. The radiological evaluation may reveal vertebral scalloping, foraminal enlargement, the collapse of entire vertebral bodies, loss of normal lordosis, cervical kyphosis, fixed anterior spondylolisthesis, atlantoaxial rotatory subluxation, and atlantooccipital subluxation which can occur in isolation or various combinations [7]. We report the case of a 49-year-old gentleman with atlantoaxial instability due to NF-1 who presented with quadriparesis and was managed by reduction with skull traction followed by C1-C2 Goel-Harms fixation.
A 49-year-old gentleman presented to our orthopaedic outdoors with gradually progressive quadriparesis associated with multiple lesions all over the body, which were present since birth (Fig. 1). Clinical examination revealed a conscious, oriented patient with spasticity in all four limbs. He had power of 2/5 in upper limbs and 1/5 in lower limbs, exaggerated reflexes, and extensor plantar response. He also satisfied the updated National Institutes of Health diagnostic criteria (2021) for NF-1 [8].
Radiographs revealed cervical kyphosis and an increased distance between the anterior arch of the atlas and the odontoid process. Lateral dynamic radiographs revealed atlantoaxial instability, with an alteration of the relationship of the atlas to the axis (Fig. 2). A pre-operative radiograph after skull traction suggested reducibility (Fig. 3). A computed tomography scan confirmed an increased distance (12.7 mm) between the anterior arch of the atlas and the dens (Fig. 4 and 5). Pre-operative angiography was done to examine the arterial and venous structures near the C1-C2 region (Fig. 6 and 7). Magnetic resonance imaging revealed a decreased spinal canal diameter and narrowing of the cord (Fig. 8 and 9).

The patient was advised of surgery to prevent the progression of myelopathy caused by atlantoaxial instability. After a thorough pre-anaesthetic check-up, written informed consent was obtained, and the patient was scheduled for surgery.
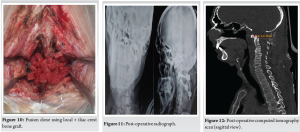
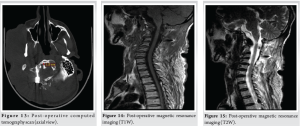
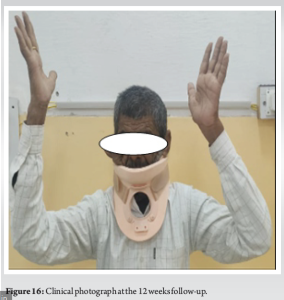
The patient was placed prone under skull traction with elevation of the head end of the table. Skull traction maintained the neck in an optimum position, avoided pressure on the face and eyes, and reduced venous congestion and atlantoaxial instability. Atlanto-axial fixation was done using the technique described by Dr. Atul Goel and Dr. Jürgen Harms (Goel-Harms technique) [9,10]. After the insertion of screws, the posterior surfaces of the laminae and arch of the atlas were decorticated, and a bone graft (local + iliac crest) was placed (Fig. 10). Substantial bleeding was encountered during the surgery, which was managed by hypotensive anaesthesia, taking preliminary sutures around lesions, ligation of a limited number of feeding vessels and gauze compression. Meticulous closure was done in layers, and a drain was placed and removed on the second post-operative day. Post-operative radiographs, computed tomography and magnetic resonance imaging, revealed a satisfactory outcome (Fig. 11-15). The patient was advised to avoid all neck movements and given a rigid cervical collar for 12 weeks. The patient was discharged after suture removal on the fifteenth post-operative day and advised to follow-up every 4 weeks (Fig. 16). At the last follow-up, at 2 years, the patient showed significant improvement in his neurological deficit and returned to his usual work.
Friedrich Daniel von Recklinghausen described NF for the 1st time in 1882. It is an autosomal dominant disease that affects the connective tissue derived from the three embryonic layers; hence, it is multisystemic. It results from an abnormality in the long arm of the 17th chromosome. Involvement of the thoracic spine is the most common skeletal manifestation in patients of NF-1, and the cervical spine is rarely involved. Atlanto-axial instability is a rare complication in patients with NF-1. Etiopathogenesis of atlantoaxial instability in NF-1 is unclear but speculated to be due to mesodermal dysplasia ± presence of NF tissue anterior to the odontoid process. ADI >3 mm is considered abnormal in an adult, and >10 mm implies the destruction of the entire atlantoaxial ligamentous complex.
In the present case, there was substantial bleeding and significant vertebral dysplasia, which makes the case distinctly unique. Skull traction and C1-C2 Goel-Harms fixation with fusion should be considered for patients with NF-1 complicated by atlantoaxial instability.
In patients with NF-1, be proactive in screening for atlantoaxial instability, especially if they present with neck pain, neurological symptoms, or a history of trauma. Regular cervical spine evaluations through imaging are critical to detect instability early. Prompt diagnosis and intervention are essential to prevent potential severe neurological outcomes.
References
- 1.Gutmann DH, Ferner RE, Listernick RH, Korf BR, Wolters PL, Johnson KJ. Neurofibromatosis type 1. Nat Rev Dis Prim 2017;3:1-7. [Google Scholar | PubMed]
- 2.Elefteriou F, Kolanczyk M, Schindeler A, Viskochil DH, Hock JM, Schorry EK, et al. Skeletal abnormalities in neurofibromatosis type 1: Approaches to therapeutic options. Am J Med Genet 2009;149:2327-38. [Google Scholar | PubMed]
- 3.Isu T, Miyasaka K, Abe H, Ito T, Iwasaki Y, Tsuru M, Kitaoka K, et al. Atlantoaxial dislocation associated with neurofibromatosis: Report of three cases. J Neurosurg 1983;58:451-3. [Google Scholar | PubMed]
- 4.Ding C, Guo Y, Wu T, Wang B, Huang K, He J, et al. Atlantoaxial dislocation associated with type 1 neurofibromatosis: Case report and review of the literature. World Neurosurg 2020;143:261-7. [Google Scholar | PubMed]
- 5.Goel A, Dandpat S, Shah A, Bhambere S, Darji H. Atlantoaxial and subaxial cervical spinal instability in two cases with neurofibromatosis-type 1. Neurol India 2021;69:1763-6. [Google Scholar | PubMed]
- 6.Hunt JC, Pugh DG. Skeletal lesions in neurofibromatosis. Radiology 1961;76:1-20. [Google Scholar | PubMed]
- 7.Lykissas MG, Mavrogenis AF, Megaloikonomos PD, Gelalis ID, Lykomitros V. Spinal deformities in neurofibromatosis type 1. Clin Cases Mineral Bone Metab 2018;15(3):348-352. [Google Scholar | PubMed]
- 8.Legius E, Messiaen L, Wolkenstein P, Pancza P, Avery RA, Berman Y, et al. Revised diagnostic criteria for neurofibromatosis type 1 and Legius syndrome: An international consensus recommendation. Genet Med 2021;23:1506-13. [Google Scholar | PubMed]
- 9.Goel AL, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir 1994;129:47-53. [Google Scholar | PubMed]
- 10.Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine 2001;26:2467-71. [Google Scholar | PubMed]










